Luncheon keynote (Beware: loud forks & knives banging on plates during first few minutes). Download MP3 or listen online here. Full transcript mildly edited for clarity below.
Dr. Virginia Hall: I want to welcome you to this afternoon’s session. The topic is something that you may not think is appropriate for lunch, a very somber, but important topic—physician suicide. There’s more than 400 physicians lost every year to suicide—a crisis we can no longer ignore. Today I’m pleased to introduce Dr. Pamela Wible, a family physician from Eugene, Oregon, who works in physician suicide prevention. I’m not going to steal from her story, because it’s quite an interesting one. If any of you have been on Facebook and lots of people know Dr. Pamela Wible. She has done an investigation of well over 1,100 physician suicides.
She comes to this work because her mom was a psychiatrist and her dad a general practitioner-turned-pathologist-addictionologist. She’s going to talk about her database with highest-risk specialties—and solutions. In addition to treating patients in her own community clinic (which itself is unique) she also runs a free doctor suicide prevention hotline. She has helped countless medical students and physicians heal from anxiety, depression, post traumatic stress disorder, and suicidal thoughts—so they can enjoy practicing medicine again.
She has been featured on major media, including The Washington Post and Time Magazine, and I understand two TED Talks. She is an inspiration to the next generation. In 2015, Dr. Wible was named one of the Women Leaders in Medicine by the American Medical Student Association and also by the Women’s Physician Section. Please join me in giving a warm welcome to Dr. Pamela Wible.
Dr. Pamela Wible: Thank you so much, Dr. Virginia Hall. And also where is Heather? Heather Wilson who put this all together, our Executive Director at the Foundation for the Pennsylvania Medical Society. Thank you all for creating such a sacred opportunity for physicians to come together and heal. So a big round of applause please for Heather and those who made this possible.
As physicians we’re used to being there delivering tough news for our patients. We’re used to being in the midst of some very traumatic conversations and diagnoses. We’re there for our patients at their most vulnerable and anxious moments of their lives. And what’s interesting is we’re very used to that context. We’re not so used to being the people who are experiencing loss ourselves, having lost maybe a colleague to suicide. These sorts of topics can bring up a lot of anxiety, confusion, and fear among physicians. And so how perfect is it that we’re sitting here over lunch breaking bread together, and joining with our brothers and sisters in medicine in a safe space where we feel nurtured and loved by wonderful food and the beautiful scene that we have in this courtyard? It was very important to me that we feel safe and connected while discussing such a topic that can bring up so many emotions.
I am going to share for the first time today the results of seven years of my investigation into physician suicide. A project that I sort of fell into because I wanted to know why so many doctors were dying by suicide. My results from investigating nearly 1,300 doctor suicides reveal the number one reason why I believe doctors are dying by suicide and also three very simple things that we can all do at the individual and institutional levels to prevent these deaths.
First I must say, It’s wonderful to be home. I’m actually from Pennsylvania (though I live in Oregon now). So after two planes, two trains, and an Uber to get here so I’m very happy to be here—finally!) Pennsylvania is the place where you can “pursue your happiness,” according to the new state slogan. So I want to introduce you to one of the people who I know that is the happiest person in Pennsylvania—my dad, Ted Krouse. It was very hard to get him out of Pennsylvania, even to come to my wedding, or to leave Pennsylvania for any reason, because he absolutely loves it here. Buried outside of Philadelphia, he was 91 when he died and spent most of his time practicing medicine in Pennsylvania. I want to thank the Pennsylvania Medical Society for having him as a member for 66 years!
He graduated med school in 1948. I believe that’s around the time that he joined this medical society—on your centennial year! The Pennsylvania Medical Society began way back in 1848. Here we are 171 years later. Of course, I love the name PAMED—it’s a combination of my name, PAM, and my dad’s name, TED. Plus all the good drugs end with PAM, lorazePAM, diazePAM, right?
My mom is a psychiatrist. So, I was constantly exposed to mental illness (tagging along to work at the Pennsylvania State Hospital). A few things about my dad I’d like to share so you understand my motivation and interest in suicide. He really set the stage for me to be somebody who could fearlessly investigate doctor suicides. He lived his natural life (did not die by suicide) and he was a pathologist who took me to work as a child. I was raised in a morgue. I know that sounds very weird, but I just tagged along with him and really loved the sacred moments that we shared in a somber place where nobody really wanted to interrupt us.
In the morgue my dad would introduce me to his patients. We’d be there talking to these dead people. I was a little kid, like six years old. He then would take me to the methadone clinic where he worked in Camden, New Jersey. He’d sit me between his clients, and himself, kind of as a little therapy dog (always fun to have a happy child sitting next to you at work in the morgue and methadone clinic). He’s introduced me as a doctor in training to the clients, then he’d tell them to show me their track marks. We did this over and over again. When I share this story with people who are not in the medical field, most wonder why CPS (Child Protective Services) didn’t remove me from my parents. But I just thought this kind of childhood was awesome as a blossoming young doctor (though these scenes probably scarred by nonphysician siblings).
My dad also worked at the jail. Before breathalyzers, they actually had to have physicians on site at the jail. Do any of you know the Roundhouse in Philadelphia? Have you heard of that place? (at least one guy in the back raised his hand). We used to be there every eighth night when he was on call. We were checking in drunk drivers together. I thought it was fascinating. I think this is what drew me into medicine. My mom as a psychiatrist took me to work at the State Hospital, and my dad took me to all these odd jobs. I just thought Wow! This is so cool! My parents were talking to people at these crazy moments in their lives, and because they’re able to give advice and be there listening, they helped transform these people’s lives. Their lives were turned around and improved for having crossed paths with my parents.
I wanted to do the same thing. I wanted to be there during people’s most vulnerable moments. Unlike most children, who probably read happily-ever-after story books with their parents, my mom was reading psychiatry journals to me. She would stop on every pharmaceutical ad in 1970s psych journals, and she’d ask me to tell her what’s going on. Look at the woman’s face. What do you think is going on with her? Then I had to tell her a story. So, I think I got very good at looking at people’s faces and trying to figure out what they needed. My dad also definitely set the stage for me to do this work. Here’s a man who reminds me a little bit of my dad—Benjamin Shaffer.
He’s a very funny, sort of a neurotic Jewish guy like my dad, and a brilliant, brilliant doctor, an orthopedic surgeon. He actually was known as “Dr. Smiles.” Here he is in high school voted “most likely to succeed.” And so he was actually voted “most school spirit” in middle school, a very charismatic, and loving guy, top DC surgeon.
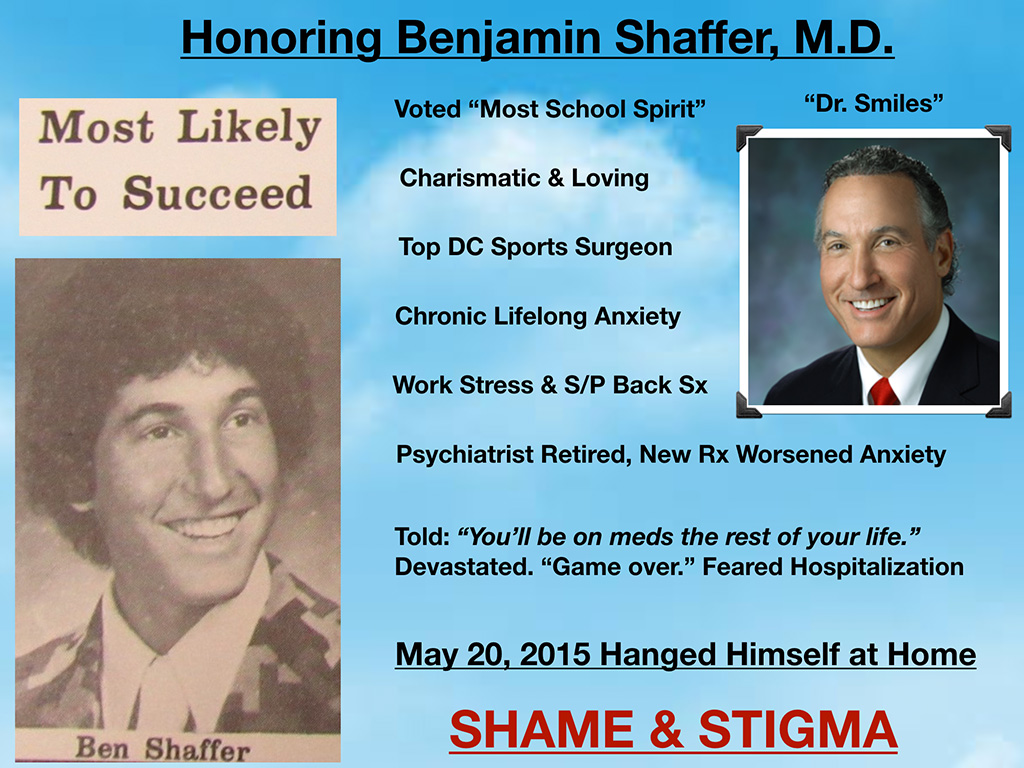
Ben had chronic lifelong anxiety, which I think many of us have a little bit of anxiety, OCD, that’s what makes us good doctors. Unfortunately, he developed some additional anxiety due to a recent surgery and work stress. He had a psychiatrist who retired, and passed him over to a new psychiatrist, who then changed two of his medications. Suddenly his anxiety worsened, he had insomnia that was terrible. At the time he was told “You will be on meds the rest of your life,” which he thought was sort of a devastation. He feared hospitalization. He would not admit to anyone that he was struggling. And unfortunately on May 20th, 2015, he hanged himself at home. And he died of a treatable condition. This was an unnecessary death of a colleague. He died due to shame and stigma. We are losing very brilliant, loving, incredible physicians to shame and stigma. These should be never events.
And so this is actually a wall in my home office covered with the photos of doctors who have died by suicide, and medical students. And I want to share with you my journey. How it happened that I would then have a wall like this.

People are like “Don’t tell anyone it’s in your house. They’ll think you’re weird.” This is what I stare at when I go into my home office. I am working on their behalf. I’ll just take you through my journey. I started with only three pictures here after I ended up at a memorial service for the third physician that we lost to suicide in my small town. I’m sitting there in the second row of the memorial service and everyone was whispering why. We all knew how he died. He died a very public death, a gunshot wound to the head in a public park. He was a top-rated physician and shot himself in the middle of the day. They all knew that he died by suicide. But nobody knew why. And he was a such a great doctor.
The whispering just sort of got to me. I couldn’t get the why out of my mind so I just started counting how many doctors I personally knew who died by suicide, or circumstances extremely suspicious for suicide. I ended up in just five minutes with 10 that I personally knew. I was about age 40 at the time. Right then and there, it was like a light-bulb moment—October 28th, 2012, at 3:00 pm. I have not been the same since. All I’ve thought about since then is trying to answer why—for me. I didn’t know that my quest for this answer would necessarily be useful for anyone else. I wanted to know why are all my friends dying by suicide—and they’re all physicians! And by the way two of those 10 were men I dated in medical school. Those men that I dated in medical school died by suicide, not while I was dating them. They were married, left children and wives behind. Shocking.
I’ve never lost a patient to suicide. I don’t know any nonphysicians who have died by suicide—only physicians. So, I left that memorial with 10. Five years later, I had 547 doctors on a suicide registry. How did I end up with hundreds of names on a doctor suicide registry you might wonder? It all started with one blog post. I wrote a blog post with 35 reasons why doctors die by suicide based on these 10 deaths. (I had my blog for a year or so before I wrote that post and I don’t think anyone ever went to my blog. Nobody ever commented. Nobody read my blog).
But then I wrote that one blog—Why physicians commit suicide—which by the way I phrased it wrong. It should be died by, or died of suicide, not committed suicide. Committed stigmatizes suicide as a crime (like committed rape or burglary). I was educated on that by a psychiatrist mother who lost her resident son to suicide. She was one of the 80 comments I got on that blog. I felt compelled to keep going since I was on a personal quest and now had 80 responses for the first time on my blog. I kept writing and speaking about suicide and I became ground zero for people wanting to talk about their loved ones’ dead by suicide in medical training. So that’s why I ended up with 547.
And then January of last year, I had 757 suicides. I wrote another article about what I had learned about doctor suicide five years later. Another 35 more in-depth reasons why doctors die by suicide. The Washington Post (kind of cool) asked, “Hey, do you mind if we republish your very well-written blog?” I’m like, “Sure.” And so we edited down a bit to 17 reasons and they placed it on the front page of the Health/Science section. The article started a deeper conversation on this taboo topic.

Since January of last year, I have now close to 1,300 doctor suicides on my registry. And this is just the tip of the iceberg. These are just the ones that organically come to me from people just randomly saying, “My colleague died.” Here’s what I’ve learned.
First, I’m going to share what I knew as of last year, in January when this was published. I know a bit more now. Of course, my understanding is deepening. High rates of doctor suicide have been reported since 1858. That’s 10 years after the Pennsylvania Medical Society was established. We’ve known about the doctor suicide crisis for a long time. I think we’ve been a little scared to dive into it. It’s taken a while for us to be able to talk about this. Physician suicide is a public health crisis that annually impacts one million Americans or more.
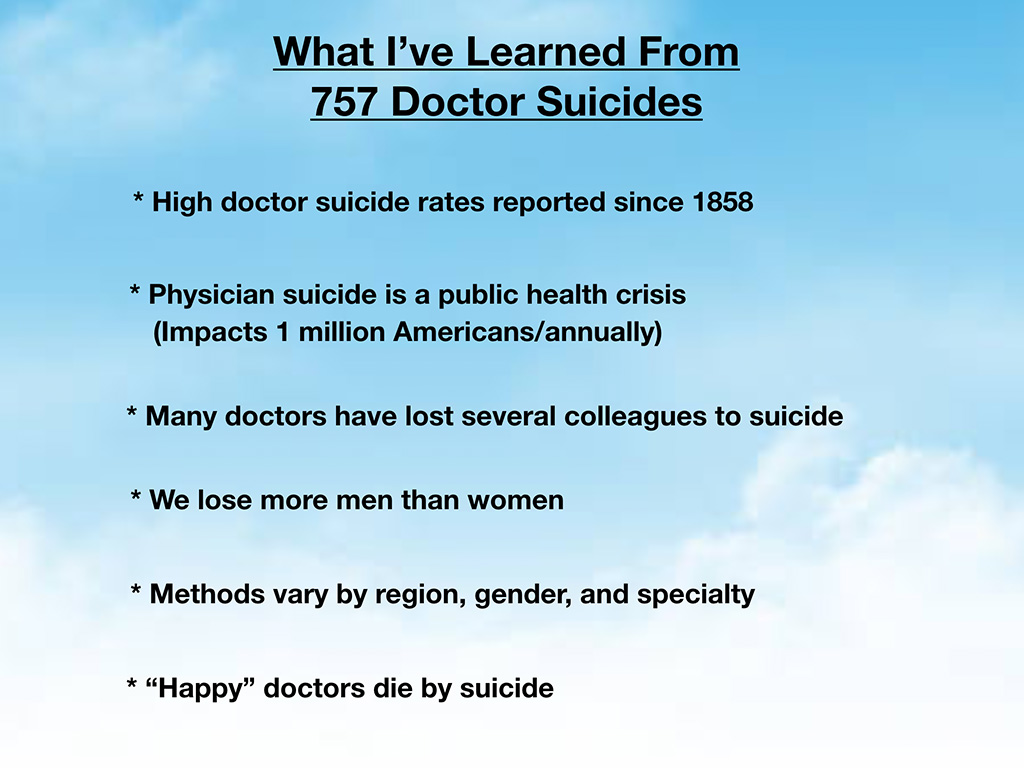
Here’s how I came up with that number. First 400 is probably an underestimate of annual US doctor suicides. Largely because we’re covering up some of these suicides as accidents. Our own medical examiners are minimizing suicides by claiming them as accidents on death certificates. Since none of us really know what somebody is thinking when they drive off a bridge, colleagues preserve the victim’s reputation and help families get the life insurance payouts by claiming the deaths are accidents (when obviously they could have actually been suicide). Of course, doctors know how to die by suicide. Doctors also know how to make their suicides look like accidents.
We have an underreporting issue (in addition to a the lack of a national doctor suicide registry). However, let’s just say it’s 400 US doctors annually. With an average patient panel of 2300 (in family medicine, for example). Just do the math. This doesn’t include medical students, and it’s an underestimate. So, you’re looking at a million Americans calling for an appointment with their doctor and being told: “Pick another doctor.” No explanation. They’re never told what happened to their doctor. I get a lot of emails from patients wanting to know, “Is my doctor on your list? Because I haven’t seen him in years, I can’t find him online. If he died by suicide, I want to know. I named my child after him. He delivered my first baby.” These are patients who loved their doctors, and they’re never able to grieve or understand what happened. Many doctors have lost several colleagues to suicide. I’ve had an anesthesiologist email me reporting, “I’ve lost eight colleagues to suicide.” That’s something that a family doc has never told me by the way. We lose more men than women.
The methods vary by region, gender, and specialty. Happy doctors die by suicide. I think that’s the thing that really trips people out the most. It’s like “Wait a minute. He was just cracking jokes with me yesterday. What do you mean he’s dead?” And so I want to draw your attention to this article that I wrote, Why ‘Happy’ Doctors Die by Suicide. It’s one of the top 10 from Medscape in 2018. It’s very short, but it definitely puts into perspective why you might lose the happiest doctor in your group, the one you least expect to die by suicide. I want to share a quote from that piece:
 Well, doesn’t that paint a picture of the doctors that are really good at keeping everyone else happy! Thumbs up to the surgical team and they’re dying inside. This brings up memories of Robin Williams, and I’m sure you know people like this. Our top-rated beloved doctors are dying by suicide. These are not fringe characters who are dying. These doctors develop occupationally induced PTSD, anxiety depression, suicidality. They have personal life problems often fueled by their professional demands. Patient deaths hurt doctors due to self-blame, and of course, second victim syndrome is what we’re learning about,with Dr. Stacia Dearman here today as well. Thank you so much for being here.
Well, doesn’t that paint a picture of the doctors that are really good at keeping everyone else happy! Thumbs up to the surgical team and they’re dying inside. This brings up memories of Robin Williams, and I’m sure you know people like this. Our top-rated beloved doctors are dying by suicide. These are not fringe characters who are dying. These doctors develop occupationally induced PTSD, anxiety depression, suicidality. They have personal life problems often fueled by their professional demands. Patient deaths hurt doctors due to self-blame, and of course, second victim syndrome is what we’re learning about,with Dr. Stacia Dearman here today as well. Thank you so much for being here.
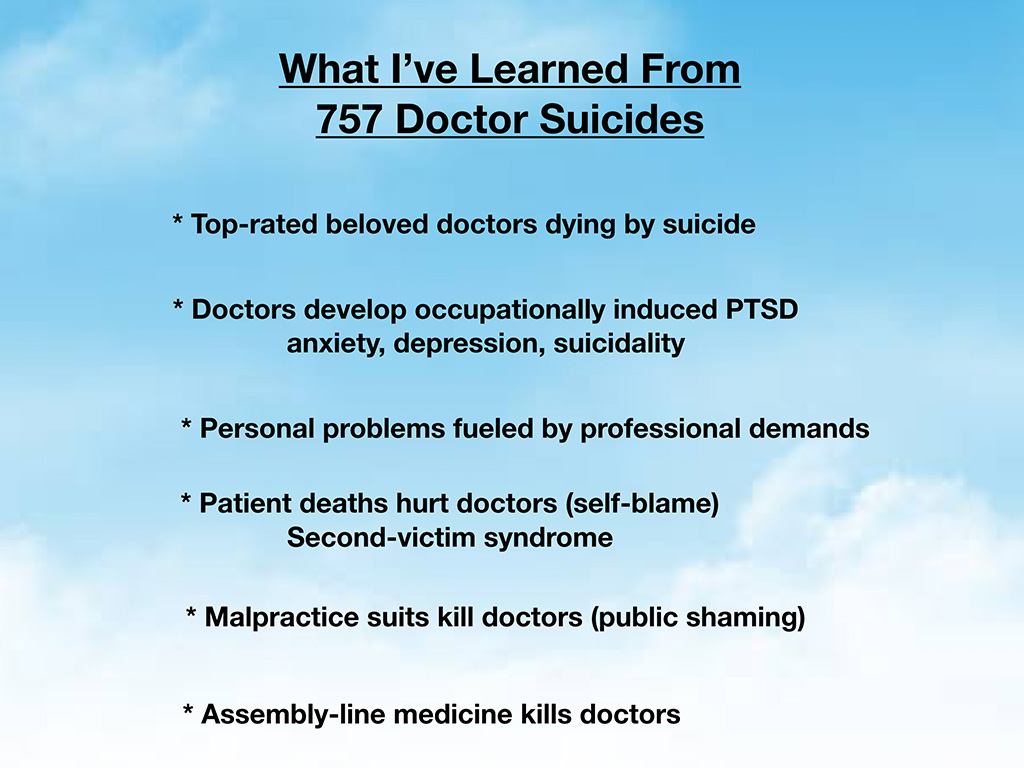
Malpractice suits do kill doctors. There are innocent doctors on my registry who killed themselves. They didn’t do anything wrong and were in the middle of a suit. They couldn’t take it. And they couldn’t live with themselves. It wasn’t even their fault. Suicide is the ultimate self-punishment. And assembly-line medicine kills doctors. That’s why I personally was suicidal in 2004. I hated my job as an assembly-line worker doling out medical “care” in seven-minute increments. I’m not a cubicle worker. That’s probably obvious now. I don’t think any of us went into medicine to be cubicle workers. However, physicians all seem to be funneled into cubicle work now. And that kills the souls of doctors who want to be real healers, connected to their patients on an emotional, physical, and spiritual level.
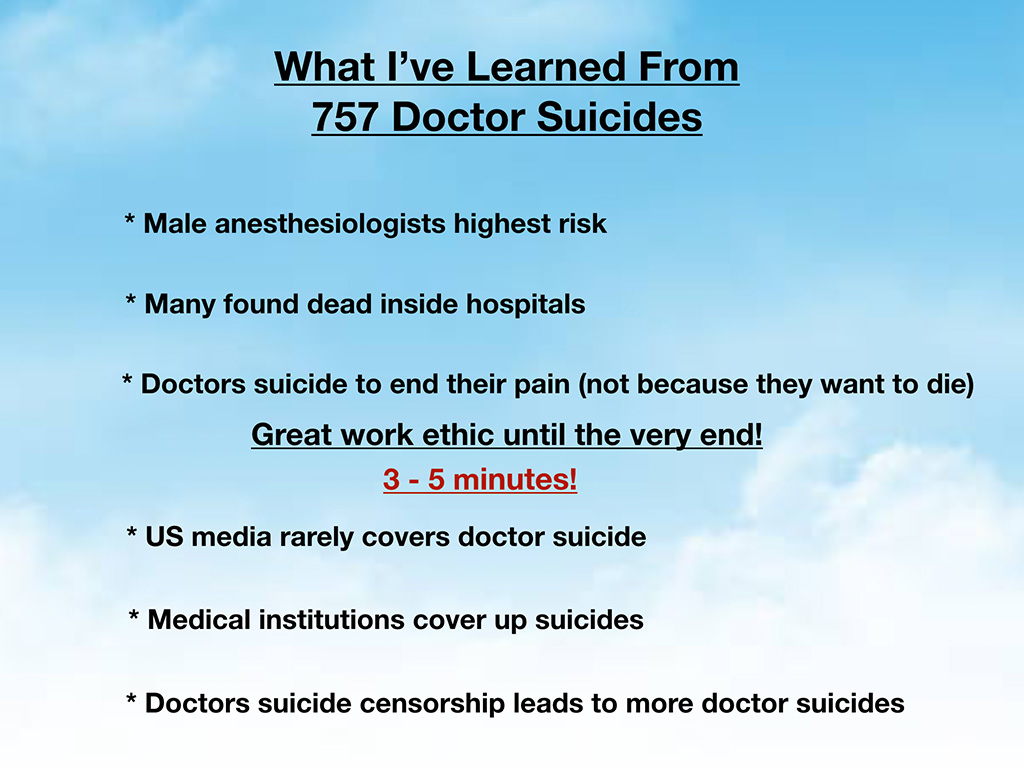
Male anesthesiologists are at the highest risk of dying by suicide. Many are found dead inside of hospitals. Google “doctor found dead in hospital,” and you’ll see a bunch of articles come up, that are very short, maybe a paragraph. Most of these hospital suicides are never reported in the media, but the articles that do come up, I can guarantee they’re male anesthesiologists for the most part. Doctor suicides happen because doctors want to end their pain. They don’t necessarily even really want to die, they just want to stop the pain. They don’t understand any other way to get out of the pain that they’re in.
Many of us (like medical boards and physician health programs) are concerned about physician impairment. All of us, of course, we want our physicians to be alert, oriented, and ready to serve, not impaired. I want to reassure you (if this is reassuring at all) the last skill that doctors lose is their work ethic. They will go into work on the day of their suicide. They will drive to work on Sunday, buy a rope at the hardware store, go in to finish all their chart notes, call their patients back with abnormal labs, leave everything done perfectly, and then hang themselves in their office. The average person who is a nonphysician doesn’t behave that way before suicide. Our work ethic is exceptional even up until the end. It’s hard to believe.
I’ve interviewed a lot of physicians, all male, who survived their suicide attempts. And I asked them “Hey, how long between when you decided ‘That’s it. I’m going to overdose. I’m going to die. This is the day.’ How long between when you made the decision, and you actually grabbed the pills, grabbed the gun?” And they said, “Three to five minutes.”
If we wait until the last three to five minutes of a doctor’s life to intervene, we’ve missed the boat. I would encourage you all to intervene as early as possible. Assume that all of us have had some troubled times in medical school or residency. Just from the statistics that Dr. Tate Shanafelt showed earlier you see that we came in with normal mental health, and by year two of medical school, our mental health is worse than our peers. Something is happening during our training. We must intervene as soon as possible in medical school to prevent these suicides. And the US media, unfortunately, rarely covers doctor suicides, although that’s changing. Finally we’re getting more traction on this topic. Medical institutions often cover up suicide because what hospital wants to be known as the place where all the doctors jump from the roofs? You can understand why they don’t want anyone to really talk about that.
Yet doctor suicide censorship leads to more doctor suicides, because it drives this whole topic underground and leads to more isolation and despair among those who are suffering. By the way in 2004, when I was a suicidal physician, I thought I was the only suicidal physician that ever existed on the planet, until eight years later when I put the three pictures up on my wall. I just thought I was sensitive and odd, an idealist with eccentric physician parents. I didn’t know other physicians were suffering from suicidal feelings.
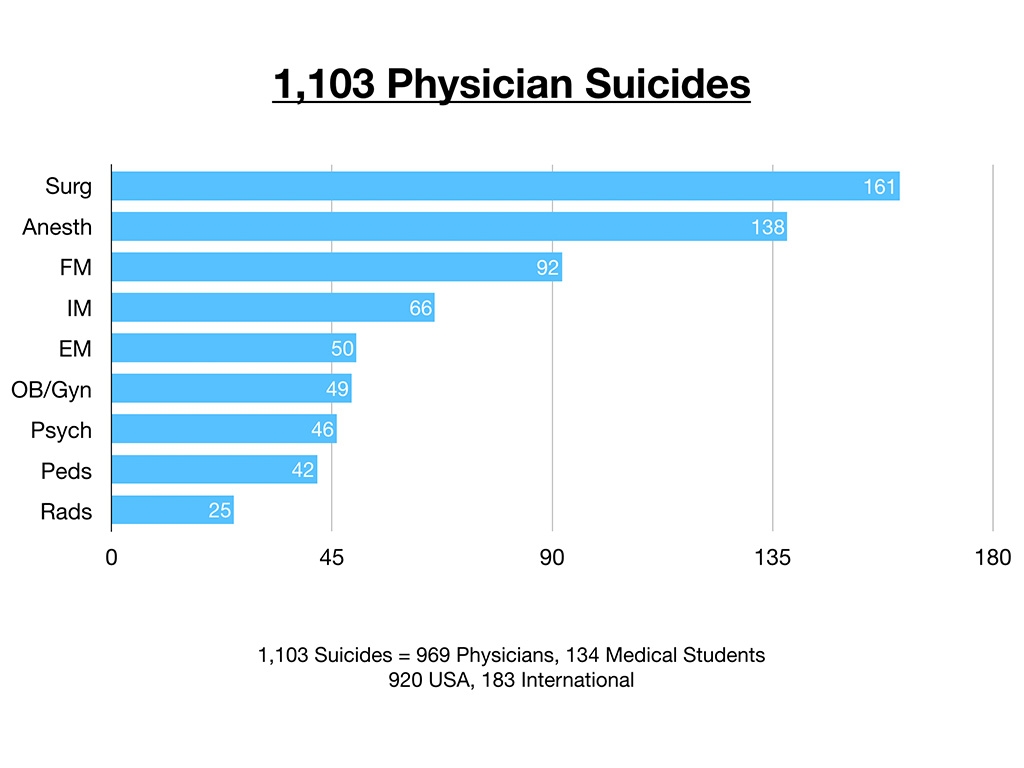
So above is a graph of the first 1,103 physician suicides that I collected by specialty. This is organic, just coming to me through spontaneous submissions. The breakdown is 969 physicians and 134 medical students. Of course the 134 medical students are not specialty-specific. Of the first 1,103 submissions, 920 of are from the USA, 183 international cases. And by and large the greatest number that come to me are surgeons, then anesthesiologists. I mean, this is interesting, but not as telling as the next slide. below.
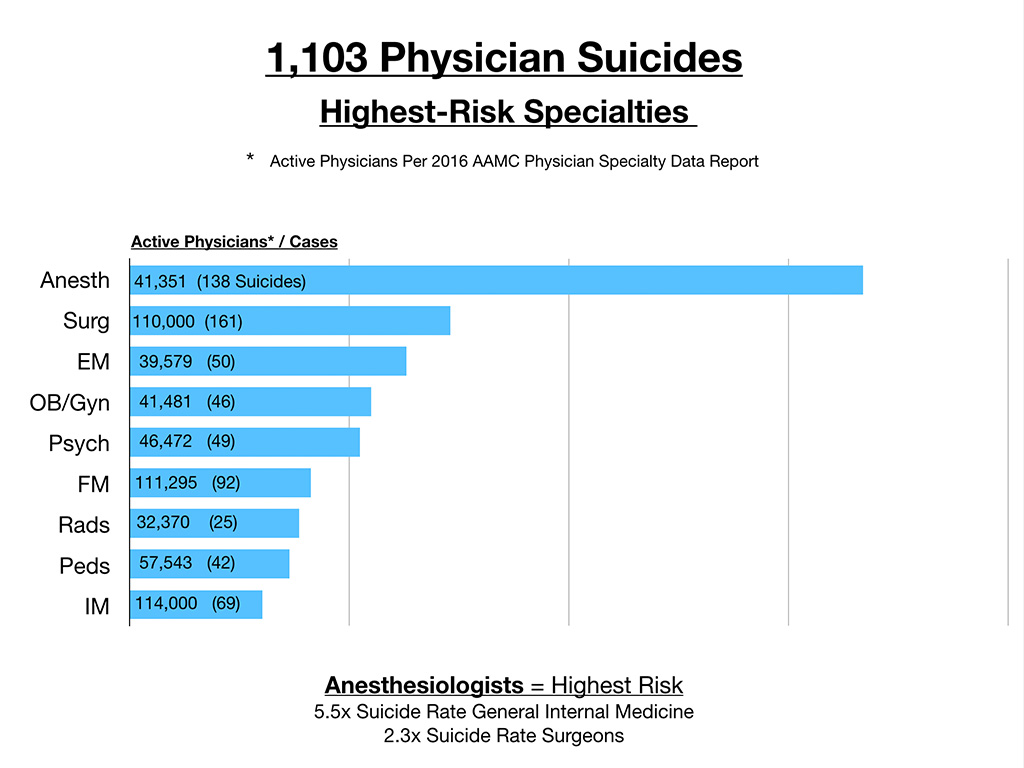
When you break this down by active physicians per 2016 AAMC physician specialty data (by the number of active physicians in the largest specialties) and compare that with the number of cases I’m getting then anesthesiologists are through the roof. They have the highest rate. Anesthesiologist die by suicide at 5.5 times greater rate than general internal medicine physicians and 2.3 times the rate of surgeons. And again, this is just from organic submissions of first 1,103 cases that came to me.
Even before I put the above graph together, I had this hunch that male anesthesiologists were number one because of the sheer volume of emails I get from anesthesiologists telling me that they’ve lost six, eight, nine of their colleagues to suicide. Some of them are CNRA’s (they’re not always all physicians) but they lose a lot of colleagues to suicide.
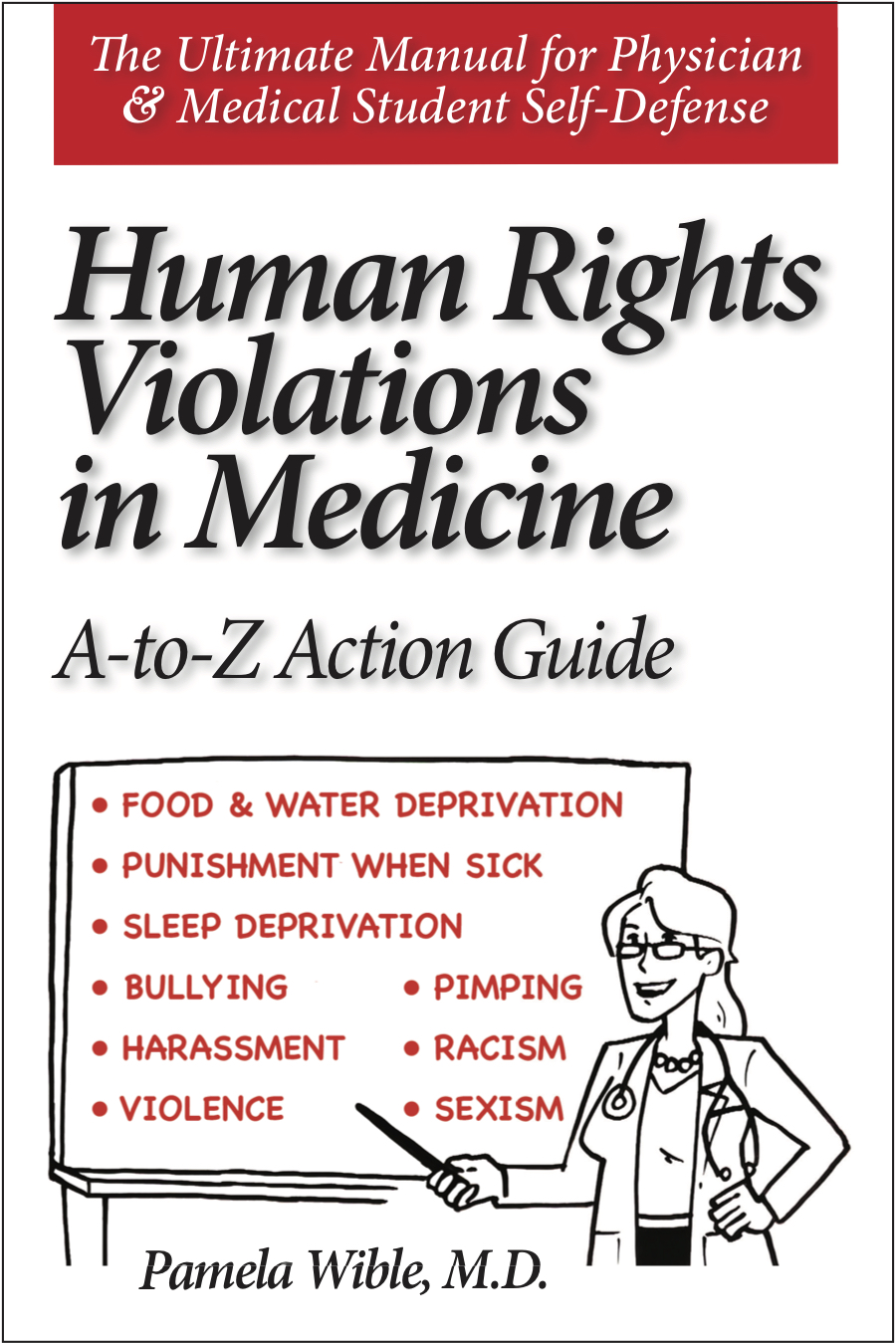
So what causes doctor suicides? That’s the question that I wanted to answer for myself. I can’t just have 1,300 victims on this suicide registry for 1,300 different reasons. There’s got to be some common themes. I’m somebody that likes to look for patterns. I’m a very curious person. And so, of course, each one of these cases has some very different reasons. But, I kept searching for some unifying theme. What became obvious to me is that essentially these people have suffered human rights violations in medical practice and in medical training (especially residency).” I know this must sound kind of harsh. But I’m going to go through why I’m claiming this. And also this is the subject of a book that I have coming out in two weeks, Human Rights Violations in Medicine: A to Z Action Guide. I’ve identified 40 different human rights violations that are ongoing in our medical education system and fully documented in the book—with simple legal and behavioral solutions.
No blame. I’m just saying this is how we evolved. I’m not somebody that likes to demonize anyone. I just think we’re in a tough spot, and we need to tell the truth about what’s not working about our profession, our beloved profession.
Essentially human rights are universal moral principles that apply to the treatment of all human beings, no matter sex, ethnicity, religion, culture—or profession. Just because you’re a physician, doesn’t mean that you’re not going to be scarred by these experiences, breaches of your human rights, basic freedoms, and standards of human behavior protected by law from birth until death.
I’m just going to share some excerpts from the manuscript of my book (please forgive any typos). In 1948, the Universal Declaration of Human Rights set the international standards for human rights, so that we might have freedom, justice, and peace in our world. All individual nations have additional documents, like we have the U.S. Constitution, we have the Americans with Disabilities Act, the Civil Rights Act that helps us have a somewhat sane, peaceful environment hopefully in the U.S. We agree to follow these sorts of precepts.
Yet physicians are even held to a higher code then the general public when it comes to our behavior. Since we have to be there for the most vulnerable, we’re held to the highest standards that safeguard our patients lives. Yet how odd that physicians, and medical students experience human rights violations that endanger their own lives. I’m going to give some examples here.

These are just a few. I know this is overwhelming. However, I would bet many of you have experienced extreme sleep deprivation, which leads some doctors to have seizures, hallucinations. I spoke to a physician who had a seizure due to sleep deprivation in residency. She almost died from a seizure, was on a vent, so very serious. Then went to follow up with a neurologist and he said “Oh, you’re in residency. We see this all the time in residents.” Why are we allowing our profession to place our own people in harm’s way with life-threatening events like seizures just to make it through the training?
Food and water deprivation, sexism, there are all sorts of human rights violations that go on. While one of these might be tolerable, it’s the cumulative effect of having sustained many of them. And not just for one year, not just during a war-time crisis. This is seven-plus years, the minimal amount of medical training from four years of medical school, three years in the shortest family medicine residency. I went to a great residency program. Sometimes people think I must have had a really bad experience in training. Though medical school was a little rough, I loved my residency. I don’t have any bad feelings about my training. However other doctors did not fare as well as me. (I have had years of therapy to recover from the trauma if the first few years of medical school).
It’s quite obvious to me that seven-plus years of not feeling safe to go to the bathroom, eat normally, or sleep, can have lifelong effects. People don’t recover from their insomnia. And plus, being a doctor is not like baking wedding cakes. We’re seeing people die and having to deal with terrible catastrophes with very little sleep, and hypoglycemia, dehydrated, and we’re trying to make life-and-death decisions while our own body is failing. We can’t trust our own brain to think properly under some of these circumstances. And we’re perfectionists. We fall into self-blame from not being able to cope with our faltering physiology under these circumstances. But it does lead to, I will assure you, long-term health impacts. Even in a medical student or trainee who felt like they had the best experience in their training, I think none of us get out of medical training without at least one violation of our human rights.
Think of Maslow’s hierarchy of needs. At the bottom rung is sleep, air, water. Then there’s a safety rung above that. I think we’re sort of thrown below the Maslow’s hierarchy of needs for seven-plus years. Some of the things that you see in the physician’s health program and other services that are there to help physicians, you’re dealing with the end-stage effects of people who have gone through what almost feels like surviving a war.
Last night at dinner, I shared that I had a medical student who wrote me, “I felt less stressed in Afghanistan during active sniper fire then as a medical student.” Which was such a harsh statement for me to read. I called her up to find out why, and it was because she knew that her comrades had her back. If she died in war, they’d bring her home, covered with American flag. She’d have a proper burial. But in medical school training, we don’t feel like our comrades have our back, like they do in the military. We never know when somebody is going to stab us in the back is kind of the overall feeling of isolation and fear that we have with each other.
I just want to share some very common human rights violations that you might recognize in some of your clients when they come to you in PHPs. This is overwork, I think that’s kind of obvious, right? Complete mental and/or physical exhaustion in a medical professional from too much work. And some examples, just to give you some guidelines here. We have labor laws to try to help people in most professions not overwork because it’s dangerous, deadly.
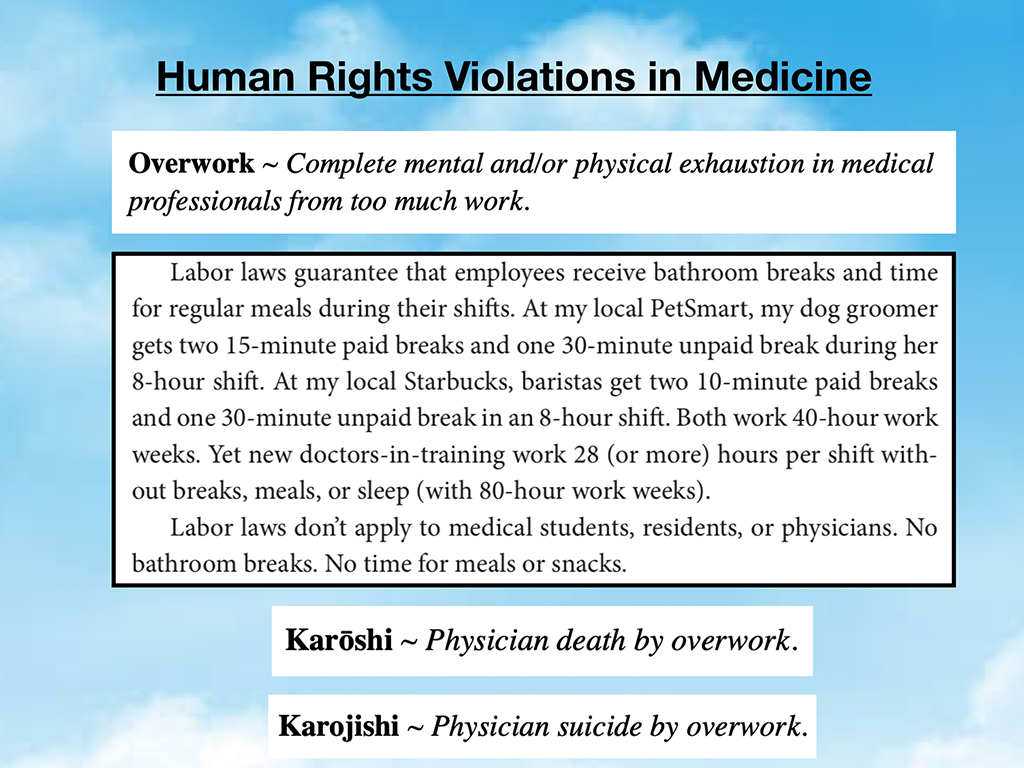
I went to interview the manager at PetSmart to find out how long my dog groomer could work on a shift. And they can only work eight hours. I asked, “Ever longer than that in a week?” Ten hours at Christmas when all the dogs come in and have to look fluffy under the tree. But they get a 30-minute unpaid break. They get 15-minute paid breaks. Similar situation at Starbucks (same labor laws). But I asked her, “What happens when they work more than ten hours?” She’s like “Well, they can’t work that long because the pets will start to die in the grooming process. They don’t notice the subtle signs of panic in the pets, and then we have dead animals.”
Now, you have to think why are doctors working beyond that length of time. I mean, for every industry, pretty much, 60 hours a week is a max for pilots, 16 hour shifts are the max for pilots (and 9 hours flying time). Air traffic controllers, you need these people to be alert. Would you get on a plane with somebody who had been up for 28 hours? It makes no sense. But in residency new doctors are now forced to work 28-hour shifts.
I mean, this makes absolutely no sense, and makes our new doctors feel unsafe. We should not be doing this. There’s actually a term karoshi. It means physician death by overwork and karojishi is physician suicide by overwork. (I’ve taken these Japanese terms and I’ve adapted them to a physician demographic).
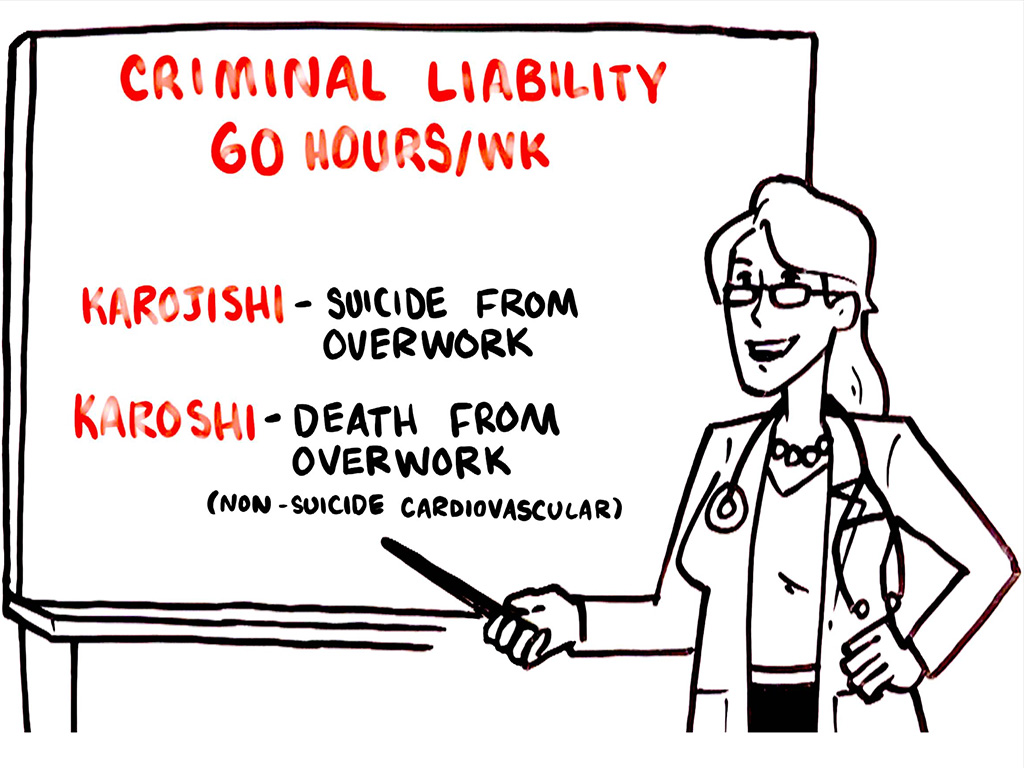
Worker’s comp cases are filed against the employers with financial payout when their employees die of cardiovascular deaths or other non-suicide deaths from overwork. Your family will get a payout in Japan if you have a death of a family member at a company that has worked the employee over 60 hours a week and then that person dies by suicide or stroke, found dead at their computer, heart attacks. Companies are criminally liable. I’m only sharing this because there’s a precedent in most other industries to never allow anyone to work over 60 hours a week. So the question is why are we allowing this to happen to physicians? And of course it doesn’t play out well for medical mistakes for patients.
Another one is sleep deprivation. That sort of goes hand-in-hand, if you’re working 80 hours a week, or 100 hours a week, you could die in a lot of different ways. You could also injure your patients, right?
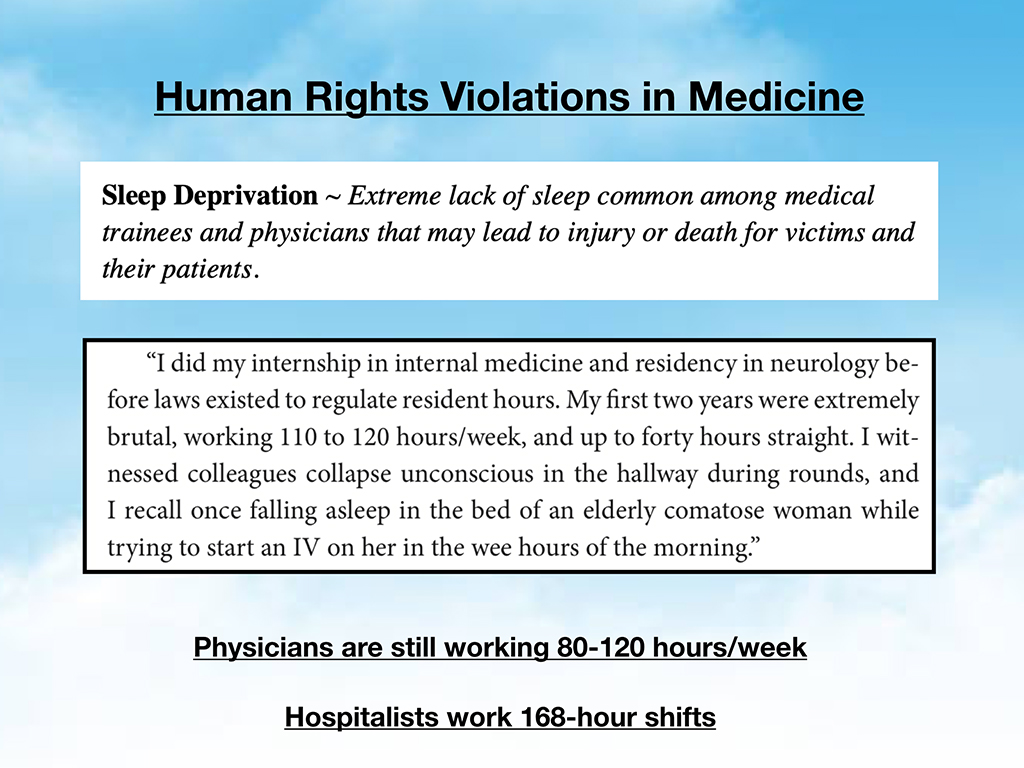
This is an example from a gentleman who said he was doing 120 hours per week, and falling asleep in the hallway. He fell asleep on top of a comatose elderly woman while trying to start her IV.

I mean, I think we all know this shouldn’t be happening in our hospitals, yet these sorts of scenes play out, where people are falling asleep in weird places under gurneys, in closets, patient beds. People are tired. Physicians are still working 80 to some of them 120 hours a week (even with ACGME work-hour “caps.”)
We think because of the work-hour caps, things are better, but with the acuity of the cases now they never get to sleep. It’s not as relaxing as when you had a baby in the 1970s and stayed for a week and learned how to breastfeed in the hospital. Now the beds are turning over every 12 hours. People have to be with it and the amount of technology and labs that come in. I mean back when my dad finished med school in 1948, all they could do was give people brewer’s yeast and hope for the best. I have his admit notes from the 1940s. There wasn’t much we could do for people. We had a lot more time to discuss cases.
Anyway, but now, it’s overwhelming, right? So, I still have residents who call me now today, having worked 100, 120 hours a week, even with this cap because it’s not enforced. It looks good on paper. I talk to a lot of hospitalists who work seven days on, seven days off, well, that’s 168 hour shift/week. That’s all the number of hours in a week, if you work in a rural hospital. Like this one doctor told me, “I mean, you will actually, maybe not get any sleep for many days in a row. The cafeteria is only open limited hours. So, you’re not eating.” I don’t know if anyone’s ever felt this way. If anyone ever felt like you might fall asleep while in residency while caring for a patient. The problem is here, that when a doctor’s physiologic needs are not met, they’re not functioning well, but the result of the system unfortunately is to blame the doctor.
This is a cartoon that shows how a doctor feels to be blamed for moving slow amid the fact that their basic physiologic needs are not being met. This is a real story of a hospitalist, who developed a seizure, and this was on one of these 168-hour weeks. The administration actually saw him have a seizure in front of them, and they sent him right back to work in the ICU. These are true, horrifying stories.

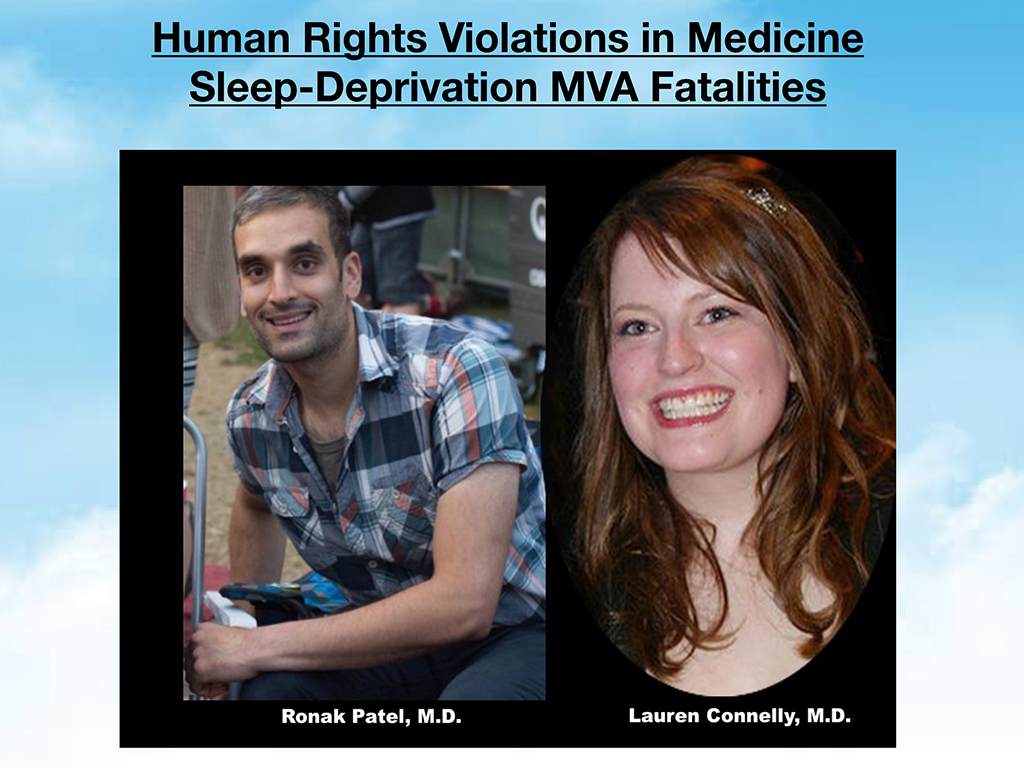
Sleep deprivation can also lead to injury or death of physician victims from car accidents. When you’re up for more than 24 hours, it’s the equivalent of having a blood alcohol level that would put you in sort of the DUI range. If we’re really concerned about impairment among physicians, probably the number one way that physicians are impaired is due to sleep deprivation, not substance abuse, not even mental health issues, but just sleep deprivation, acute sleep deprivation. And these are just some examples.
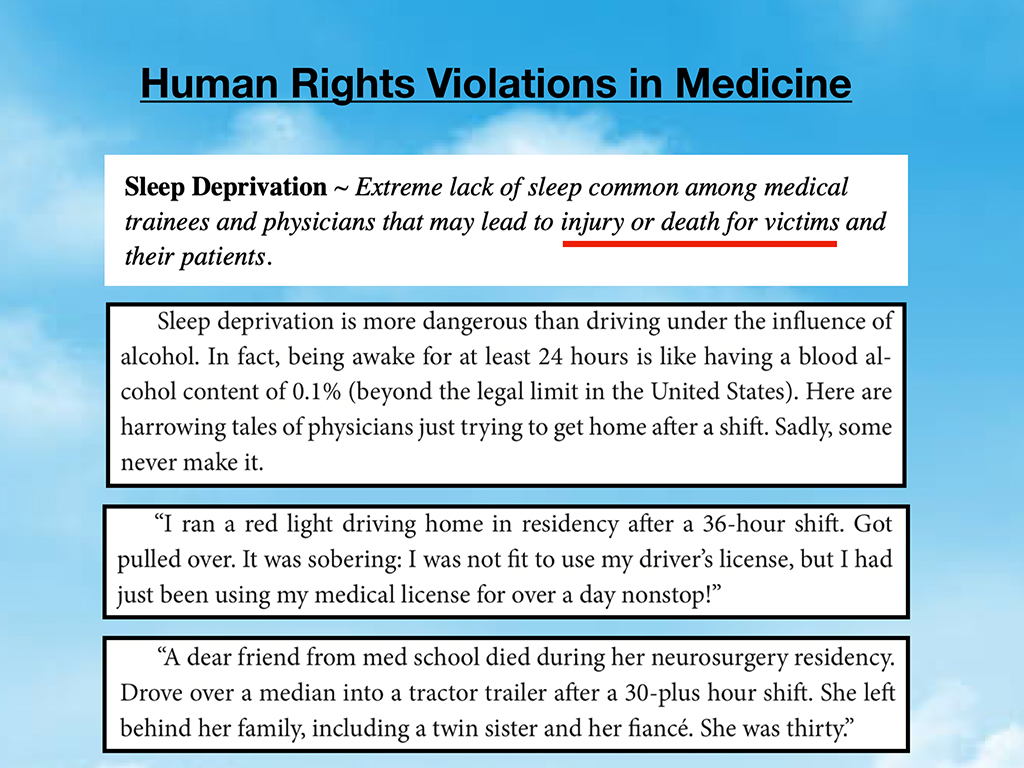
They’re all very sad. But a dear friend from med school died during her neurosurgery residency. Drove over a median, into a tractor-trailer after 30-plus hour shift, and left behind her family, including a twin sister, and her fiance. She was 30. These are actual physicians that have died by motor vehicle accidents after not being able to make it home after 30-plus hour shifts. This is another hazard on our highways that can end up killing innocent people in other cars. We’ve got to put a stop to this.
As a health care profession, we should never allow people to leave the hospital unsafe to drive, yet just running the ICU like 30 minutes before, it makes no sense. But then the reaction, unfortunately, I think because we all need to have more of a collaborative approach to dealing with this, and really dealing with it an institutional level. But the knee-jerk reaction of the ACGME and other organizations is, “Well, if they’re not sleeping, send them to a sleep lecture. They’ve got to learn the importance of sleep.”
So, I’m just telling you when the residents call me crying, they tell me they feel like they’d really like to go home and sleep after 24 hours, but now they’re being forced to go to an importance of sleep lecture. And the older doctors are calling them “weak snowflakes.” This is how they feel.
I didn’t know how else to share it other than a cartoon. But that’s kind of a little bit of insanity of what’s going on when you force people who aren’t having their rights respected to have more wellness to-do activities (that they would naturally do if they had free time, but unfortunately, they don’t).
And food and water deprivation again, I don’t have to lecture you on the importance of eating and drinking, so that you don’t die. But people have nearly died during medical training from acute renal failure. You leave these students in a situation where they’re stealing leftover food from patient trays in the hallway. They’re trying to get the crackers and apple juice from the nurse’s station that are really for patients. And it’s a sad state of affairs.
I thought of some ED docs that have told me lately they’re not even allowed to have water bottles at their desks. But they don’t have time for a break. How are they not going to get dehydrated? Some of us have medical issues, have diabetes, when we start residency. You can end up in diabetic ketoacidosis and require hospitalization just from lack of access to food and water at reasonable intervals that people need to live.
A friend of mine lost 42 pounds in her first five months of her emergency medicine residency. And she’s not the only one, I hear all the time from people, “I’m 130 pounds, and kind of a small frame, but I’m now down to 110, because I haven’t had time to eat and we’ve been so busy.” When you do the caloric expenditure calculations day-by-day for residents, I don’t think that’s a good time to be intermittently fasting or losing that kind of weight. This is just the truth of what people go through.
And then they feel like they’re called unprofessional. Here’s a surgeon who has collapsed from dehydration and hypoglycemia. These are all true stories.

Then there’s of course discrimination that people sustain in all organizations. But in medicine, on top of the sleep deprivation, the overwork, the lack of access to food and water, to then be called a racist. My friend who is residency now, I mean, guys come in with confederate T-shirts on, and call her the N word. And she’s just supposed to power right through that. And if she raises any attention to it, they’ll say “Well, your skin is too thin.” It’s a doctor’s job to take all this toxicity coming your way. You feel like you’re in a hostile environment on top of the sleep deprivation.

Try not to get too depressed here because I do have some very simple solutions at the end. But, I think in order to solve this. We sort of have to identify the precise problem and have language to discuss the problem. These are just some examples of discrimination that people have faced. Breaches of their “confidential” medical records is another issue. If you get medical care at your own institution, your supervisors and peers are often in the EMR looking at your records. There are frequent confidentiality breaches. Your program director sending you to an in-house psychiatrist and then reading all your records. This is a HIPAA violation. The number of calls from people who have experienced this is astounding.
Just one example are physicians with mental health issues afraid to get mental health care. They drive hundreds of miles out of town and pay cash and they make sure they’re going to somebody who is using paper charts that in no way will ever breach their confidentiality. I mean, can you imagine if getting a colonoscopy involved sneaking out of town, using a fake name, and paying cash and paper charts. What a huge obstacle to people who they feel unsafe, either because there’s a lack of access to anything at their institution, or what’s available to them they perceive as unsafe so they’re willing to make this dramatic move or (more likely) not get care which is very sad. So I think we all want physicians to feel safe to get care locally with people that they can trust, where their confidentiality won’t be breached. There are examples here of physicians being fired because they needed a wheelchair after hip surgery.
Bullying, hazing, and intimidation, I don’t think I have to go through the definitions of these. But people experience this in the first few years of medical school, this might have something to do with why they’re not feeling as well as their peers two years later. Unfortunately, I have several examples of people just being bullied to the point where they’re having panic attacks at home and they’re scared to go to work or school the next day.
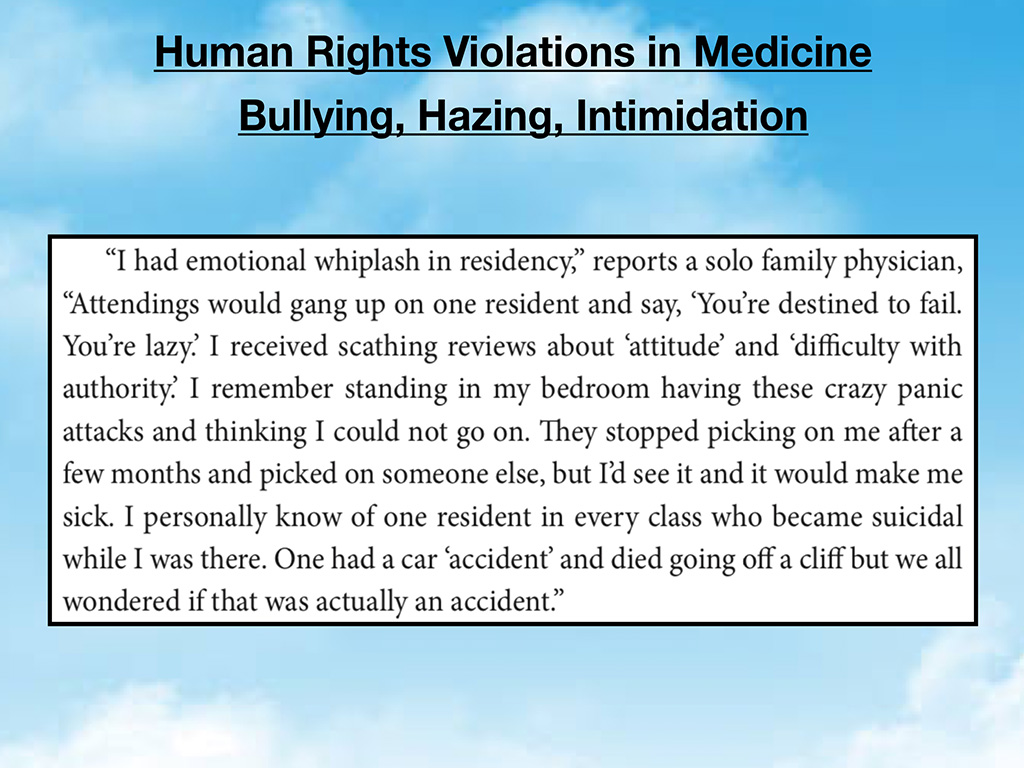
The whole pimping thing. Do we really need to continue that? Such malignant levels of pimping? I think when people are afraid, they’re not going to retain the information. They’re just going to remember being terrorized by that attending.
I think we can do this in a better way. These are just from the last year, people have told me, “The incoming class at my medical school is just told by our assistant dean of academic affairs on their first day of orientation that he was there to crush their souls.” How is this helpful? This is a medical student that wrote me, “I’m in a medical school where the president of the school has told students to kill themselves, jump off the top of the building, and he also personally attacks students based on weight.” It’s a school not too far from here. I get calls on this school all the time. I get calls from a mother who told me she’s concerned that her medical student child will actually follow the instructions. Her medical student child is depressed and attends this school, and he is told these things.
I would think any of this was sort of outrageous. It’s just that I hear so many, different people calling from all different area codes with the same sort of story. Then it makes me realize that these aren’t so rare. While these seem to be a little bit off the bell curve, they are not totally isolated. Again the combination of these violations on top of everything else. I mean this last one is very extreme. Bully professors remain in power positions and continue to torment surviving students even in the aftermath of losing their friends to suicide. One female physician reports, “After one of our residents killed himself, two of my professors sought me out to gloat that their abuse had resulted in his death. They were proud of it.” I mean, it’s hard to wrap your head around this, but this actually happens.
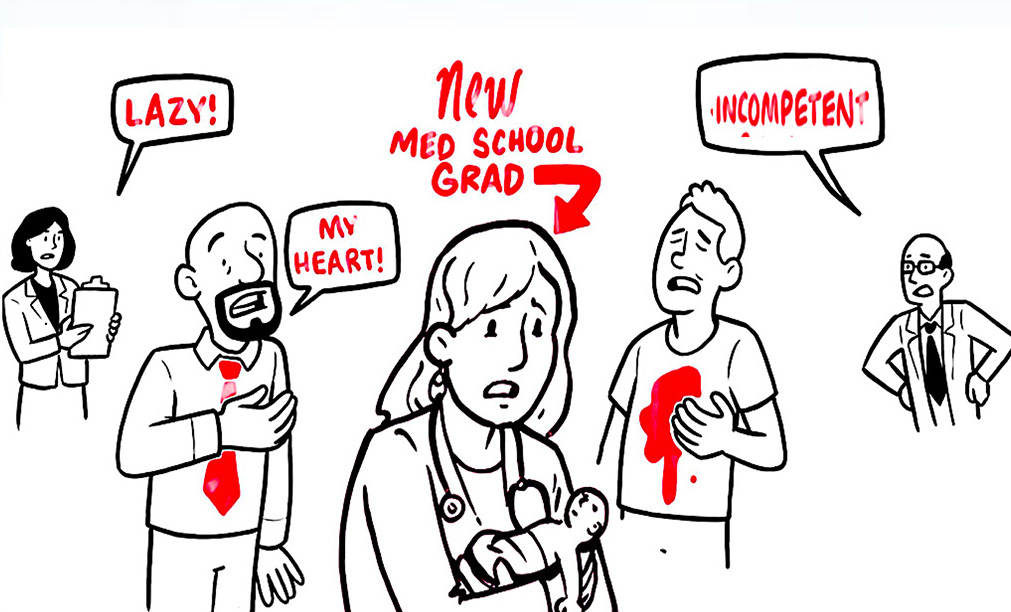
You leave a new medical student grad, this is a new intern in the cartoon above. They’re going to start July 1st, this is the feeling that they have. This is why they’re scared to start their intern year. It’s not just “Can I take care of these patients? Am I going to do a good job?” It’s, “Can I do this on a 28-hour shift while I’m being told I’m incompetent, or lazy, and not moving fast enough?” And there are people coming in with heart attacks and strokes. An impossible situation for someone to feel well.
IMGs (International Medical Graduates) experiences even more human rights violations than American resident physicians and are at risk of being deported if they protest unsafe working conditions. See this brief interview with an IMG who reveals the plight of abused foreign doctors.
And maternal deprivation. There’s only a few more I’ll share, and then we’ll go into solutions. But, obviously, as Dr. Tate Shanafelt shared earlier, I think in his main talk, but definitely in the breakout session is that it’s very hard for women under age 40, in medical training, during their fertile years to handle all of this and procreate and be there for their kids. So, you have a situation in which women are having miscarriages. Read examples below:
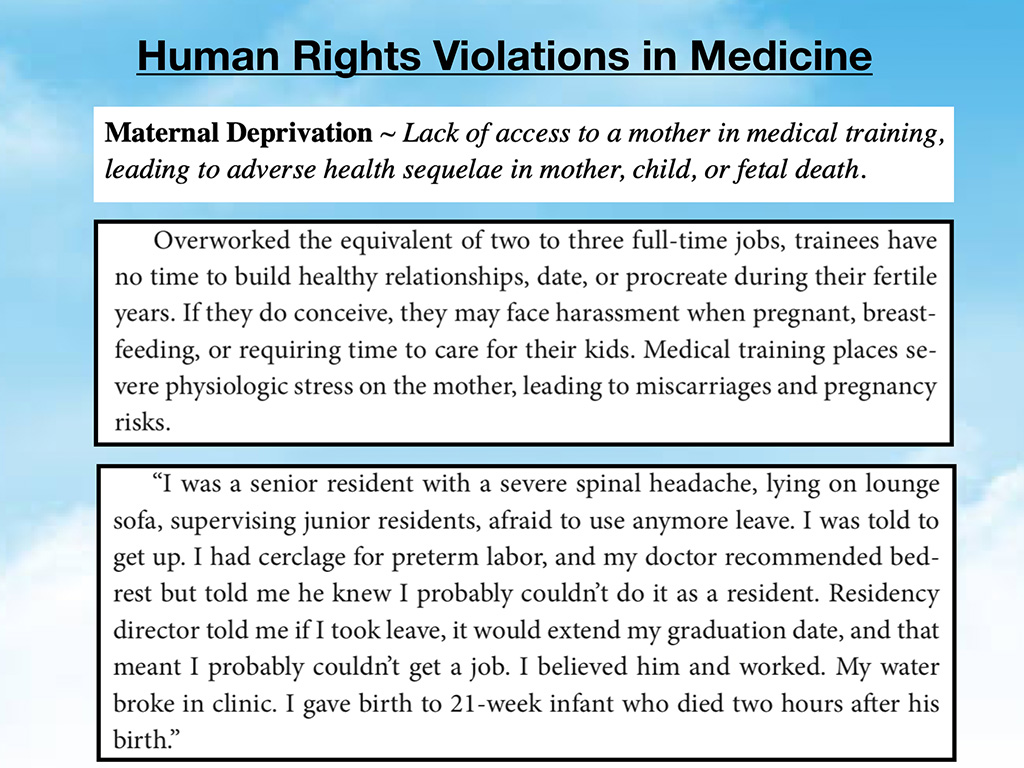
We’re putting women in an untenable situation where they can’t procreate during their fertile years in a way that’s safe, where they can’t take care of their children. If you become a female neurosurgeon, you don’t really get out of that till you’re after your mid-30s. And then you are quickly trying to go on dates. The number of women who call me to disclose, “I just froze my eggs. I’m hoping to date one day. I’m 36. Is it normal to have panic attacks?” It’s very sad.
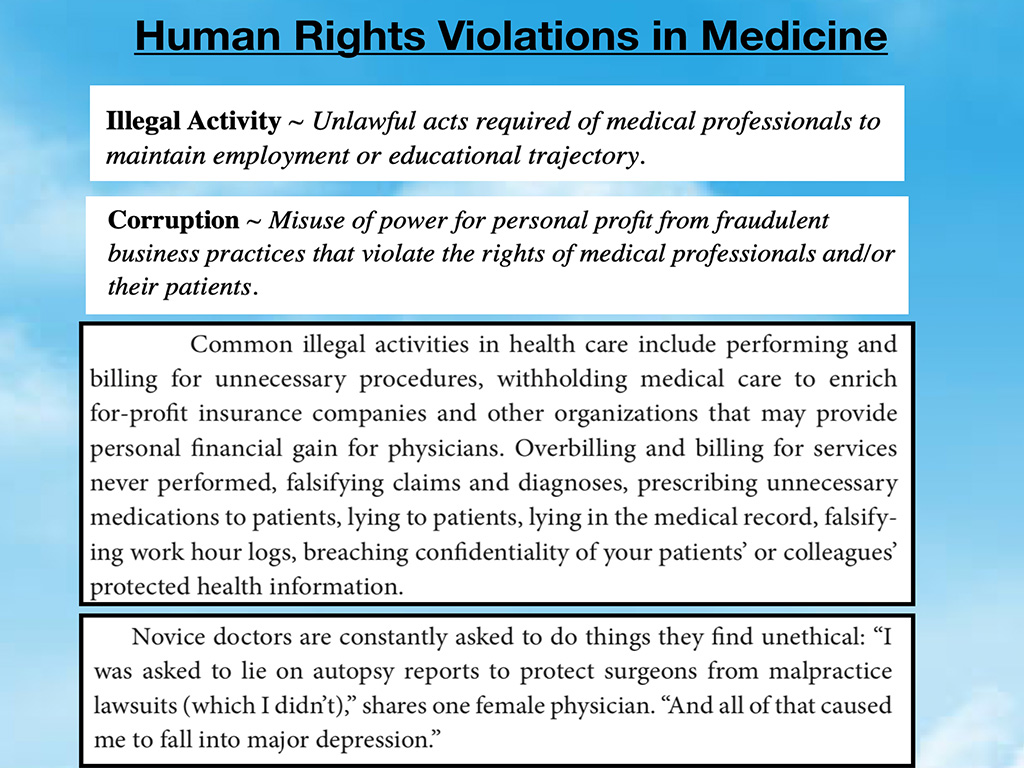
In addition, there’s a lot of illegal activity and corruption in our hospitals. I’m sure not one person in this room can tell me that they haven’t seen some upcoding, fraudulent claims here and there. There are things that happen that are frankly illegal. In many of the jobs I was in, we’d have lectures demanding that we “code at the highest level. It’s a 99214, not a 99213.” Physicians are doing things without the patient fully understanding and getting consent. There are these things that happen that are truly in the “moral injury” category when people feel they’re in a situation where they can’t practice in alignment with their values.
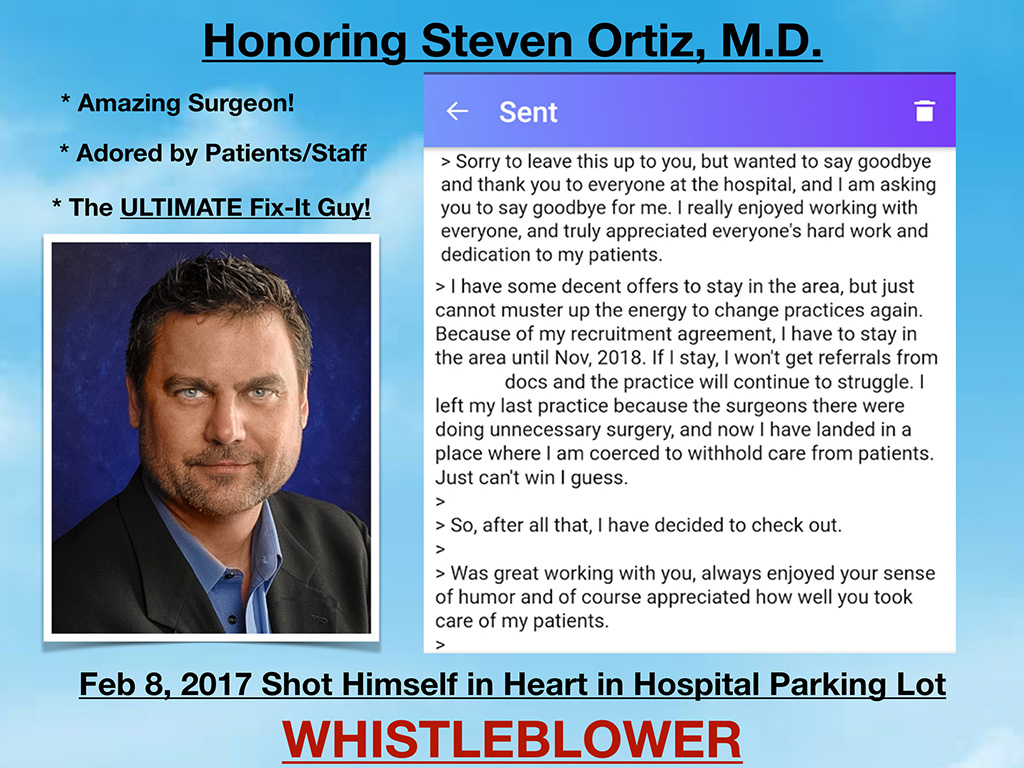
I want to share an example of one man who was faced with illegal activity and corruption at his hospital. A cool orthopedic surgeon, I mean, this is the guy you would totally want as your ortho doc. I mean, he would fly home early from vacations to take care of patients if they fell ill. His hospital parking lot had large potholes that weren’t getting fixed, and he couldn’t have his patients bouncing up and down in potholes. So he actually went in one day and fixed them all, early before surgery. An orthopedic surgeon fixing all the potholes in the parking lot. Coolest, guy ever. Unfortunately, this was the last text he sent to his nurse before he shot himself in the hospital parking lot as a whistleblower due to the corruption in his hospital. He did not see a way out, and apparently the quick end of the story here is he was in Florida practicing at a hospital where they were encouraged to do more procedures than necessary on patients to increase the amount of revenue coming in which he didn’t feel comfortable with.
He changed jobs. Then he was at another hospital where they owned 51% of an insurance company, and they were supposed to not do procedures on patients, so that they could retain the premiums and not spend a lot of money on patients. So he was coerced to withhold care in one place and over deliver care in another. This guy is like a guy of extremely high ethics. He tried to work this out. He tried to meet with the hospital board of directors. Everyone is like “Well, just go with the flow. This is how it is.” And he couldn’t. So we lost an amazing orthopedic surgeon as a result.
I didn’t even know what gaslighting was. This is kind of interesting again, because this is the perception of current medical students and residents (and practicing physicians). They feel there’s some sort of psychological manipulation leading them to question their own sanity, especially when they are mandated into forced wellness lectures
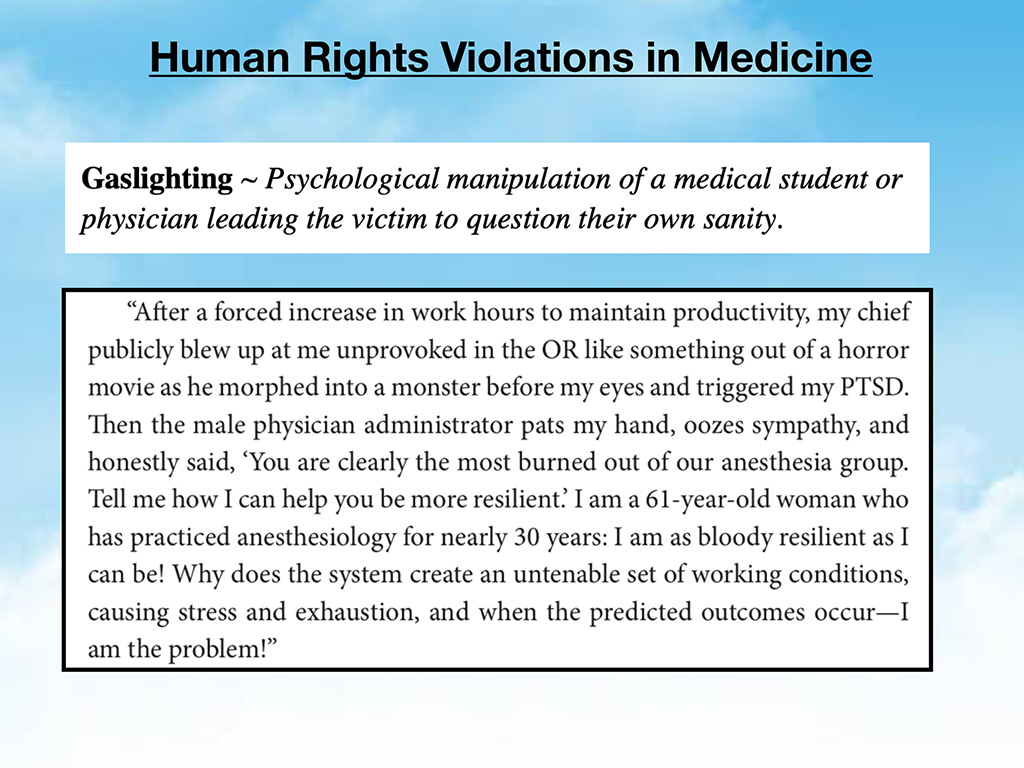
And again there is nothing wrong with the term burnout or resilience in and of itself. But when they are used to blame victims who feel like they’re basic needs aren’t being met. They interpret this as gaslighting. That’s how they interpret it because they start to wonder,”Wait a minute. Is there something wrong with me? Maybe I do have burnout. Maybe I do not have enough resilience. I mean I’ve been a valedictorian, overachiever my whole life, and suddenly I’m not functioning, maybe it is me.” And so what happens is these people feel sort of unfortunately by the way that we’re using this terminology, people feel assaulted by these terms, like it’s their fault. A few more examples:
So, I think it’s really important that we address this in a way where the victims, the current medical students, and physicians feel empowered, and supported, and not further victimized by the way these terms are used, and I’m sorry I have to go a little fast here at the end. But this would be a picture of how they feel. They feel that they have a lot to do, they better quick hurry up and do yoga, keep a gratitude journal, meditate, and yet this does not address their core issues of not getting sleep, food, being in an unsafe, hostile environments where they’re not able to deliver the care that they had imagined they would deliver to their patients.

This is just a picture of a surgeon who needs to go to the bathroom and he’s told he lacks resilience. I’m embellishing this a bit to make a point. But this is how people sometimes hear these words, like there’s something wrong with them.

From the thousands of hours of calls I’ve had with suicidal doctors this is how a physician feels in a pictorial form, like it’s their fault, like they did something wrong. And they are just having essentially a normal reaction to unsafe working conditions and an inability to get the support or mental health care that they need. They have developed occupationally induced mental health problems that they did not have before medical school.
They feel thwarted in their ability to actually go get mental health care without being worried that it will end up on their transcript, worried that they won’t get into residency or maybe the medical board would find out and then they’d lose everything they ever worked for in their whole life. And so that’s why they sneak out of town, pay cash, and get care elsewhere.
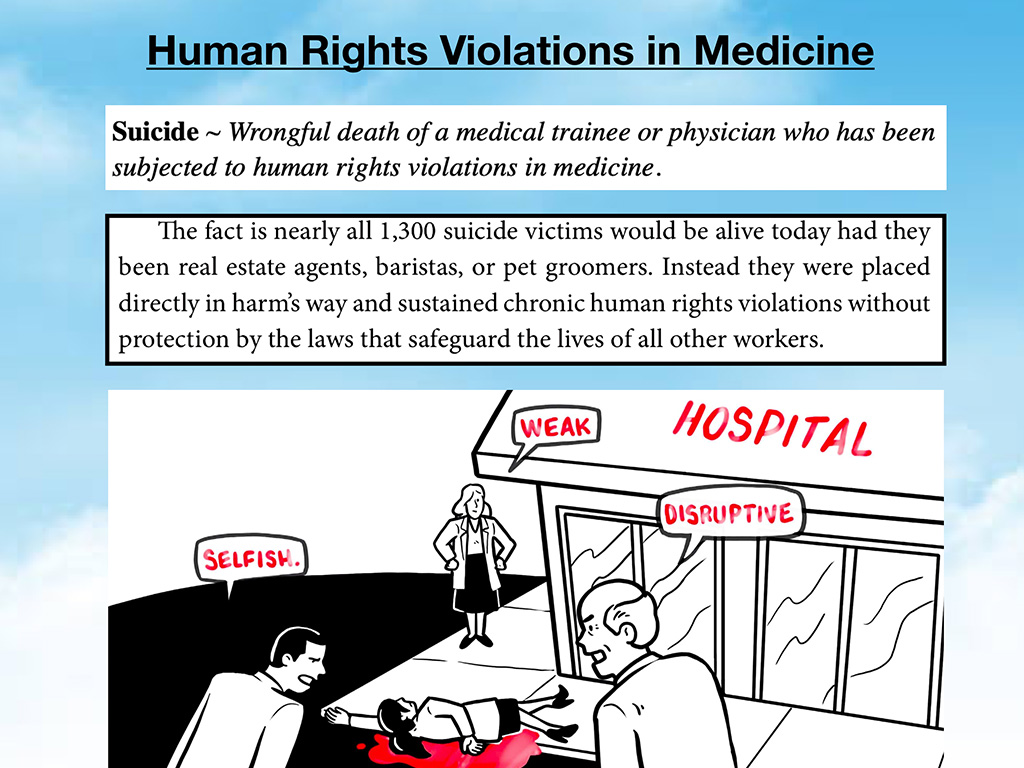
The end result of all of this is that you have people that succumb to suicide. I believe if these people were in safe working conditions at PetSmart or as pilots, I think most of these 1,300 people on my registry would be alive. Unfortunately, they were left in harm’s way in our own medical institutions. Unbelievably tragic.
I interviewed a physician who became psychotic from sleep deprivation on 40+ hour shifts. She’s a very good friend of mine, in residency. She said the worst part about it is you can’t trust your mind, you can’t trust your own body, and then you feel like people don’t trust you. And then you’re in a psych ward. But you were normal when you could sleep. She was placed in unsafe working conditions and developed a known physiologic response to extreme sleep deprivation and then was mandated into a PHP (where she did well) and is now a successful physician in private practice. Why did we allow her to be placed in such unsafe working conditions in the first place? All of this could have been avoided with labor laws that protect doctors and patients from such hazardous working conditions.
You know what I mean? Sleep deprivation causes you to lose a grip on reality, and yourself. And as a result you could end up dying by suicide. And I think the worst thing that happens after your suicide is you’re defamed, and demeaned as weak, as collateral damage, just part of medical training, you weren’t strong enough. What a terrible way to treat other people! Yet this is what I have witnessed again and again.
Now the solutions. There are lots of solutions being put forward, but I think some of these solutions are simplistic and don’t necessarily address the core issues that are creating such distress among doctors.

None of these solutions are bad ideas. I just don’t know that they can fix the human rights violations. Above is a picture of military docs with adult coloring books. They had to color for a resilience day. Now I love coloring. I am such a fanatic about art projects; however, this sort of thing with military doctors that were in this coloring event, they didn’t necessarily feel like this was helping. They still had patients lined up. They still had a ton of charts piled up. Now they had 30 minutes of coloring to do. This is just kind of what’s going on.
Yoga, I’m not really good at yoga. Though many of my physician friends are actually cross-trained as yoga therapists. And so there is absolutely a role for yoga in healing, however it doesn’t really solve the human rights violation aspects of our medical training and practice. Swing dancing. Gratitude journals which I keep, but I don’t think it’s a solution. I mean, these are just some of the solutions that are put forward. Individually, they can help some. But the point that I’m trying to make is they don’t solve the human rights violations.
But the next three solutions do. They’re very simple. Number one is we need to remove the mental health questions from state licensing applications. Twelve states have already done this: Connecticut, Hawaii, Indiana, Kentucky, Maine, Maryland, Massachusetts, Michigan, Nevada, New Jersey, New York, and Pennsylvania. Pennsylvania does not ask mental health questions and has no generic impairment question; however, Pennsylvania does ask about the use of legal and illegal drugs that may lead to impairment. “Do you currently engage in or have you ever engaged in the intemperate or habitual use or abuse of narcotics, hallucinogens, or other drugs or substances that may impair judgement or coordination?”
[Please note I’ve updated the above paragraph since the keynote and have a research paper coming out on the above topic of state boards mental health questions this summer.]
These mental health questions on job applications are illegal. They’re against the American with Disabilities Act. They are preventing our physicians from feeling safe enough to get the mental health care they need. This is an actual portion of many mental health questions on the current Alaska medical state licensing application. Across every state, they’re all different. But twelve states have been very progressive in just removing the question.
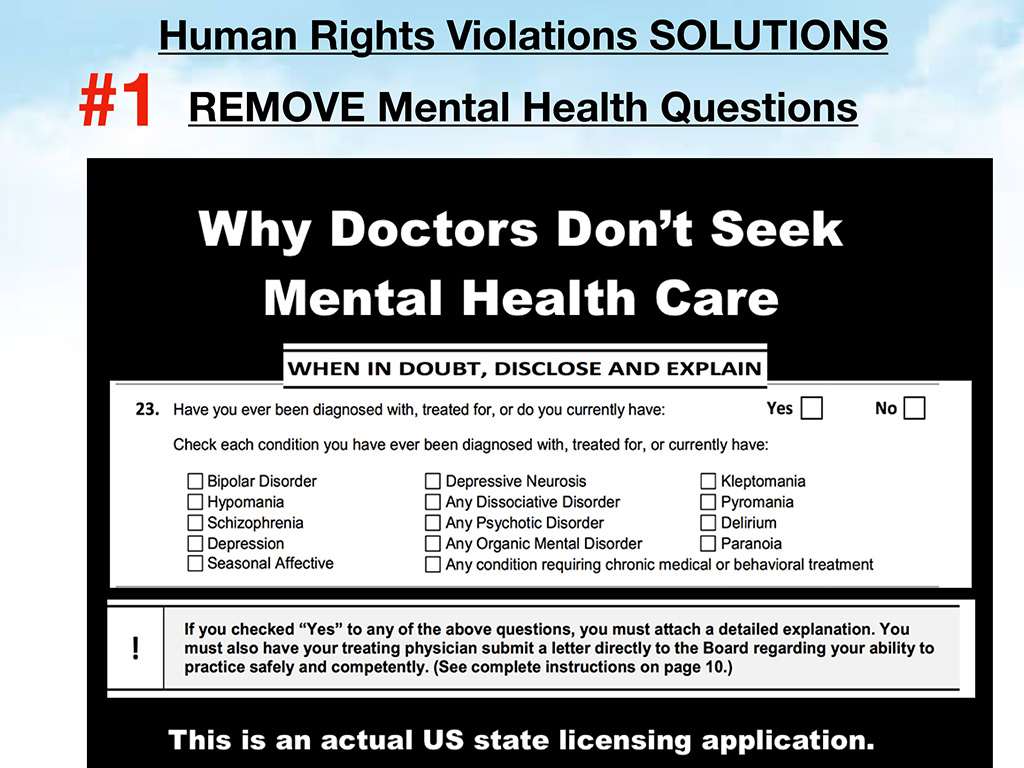
Underneath the mental health question, what we all want to know is, “Are you impaired?” That’s really the question we’re asking. It’s just that we’ve shoved it together with mental health, and other things in a way that makes people feel like they are criminals to be receiving mental health care. Removing that question would do a lot to help us, because first of all, it’s an illegal question and shouldn’t be on there. And by the way, mental health questions are asked not only by state medical boards, but they are also on applications for insurance contracting and hospital privileges. We need to remove these from every job application that has anything to do with doctors, they should not be answering such invasive questions about their mental health.

Certainly find out if they’re impaired, but not invade their privacy because mental illness does not equal impairment. It’s ill advised because the number of physicians that tell me they lie on these forms anyway. They’re just lying. So, you’re just going to push everyone underground (like literally) or they’re going to run to another town with paper records and cash. We’re going to create more ill physicians because the physicians who really need mental health care probably are not the ones driving 200 miles out of town and paying cash. They’re staying in town and they’re sort of deteriorating in front of our eyes while pretending to be “happy.”
Remove the question completely, which is my number one suggestion. That couldn’t be too hard. I mean, we can come together as a group and just say “Before the end of 2019, we’re nixing all these illegal questions off all these applications.” We can do that, and that could be sort of an easy move that would require some consensus. Follow the lead of these twelve progressive states. Or we could replace it with a better impairment-related question.
Number two: We also need labor law compliance. Every other industry follows these laws. This is physiologically what human beings require so they are not impaired at work. We require maximum 16-hour shifts. After that you are becoming impaired. And over 24 hours it’s as if you’re a drunk driver. That’s how impaired you are. Nobody should be working more than 60 hours a week, and that includes charting in your bed at night, almost falling asleep on your laptop. Plus every eight hours we should have a 30-minute break.

If we could do this in medicine, we would actually solve a lot of the distress among doctors and prevent these suicides, prevent the mental health issues. Number three: We do need non-punitive mental health care. These are some things we could start in hospitals; peer support, debriefing after traumatic cases, keeping everything local. Like I said in the last skill that goes for a physician is their work ethic. If you can keep them attached to their job, their benefits, and their salary, they’ll be able to actually pay for mental health care. If you make them go out of town for six months, or three months, they lose their job, they lose their benefits. They lose the only thing that keeps them stable, which is seeing patients, which brings them joy. You sort of further destabilize them. And we need suicide prevention and postvention. I would request that we stop blaming doctors for normal reactions to human rights violations.
The last slide here is we can improve physician health programs so that people feel truly safe to go there, with more than just substance abuse issues. I hear from people all the time, I wouldn’t have known this, but people tell me that they have postpartum depression, or anxiety, but now they’re in a PHP where they’re mandated into a 12-step program with random urine drug screens (but they don’t use drugs!). So, I think we need a personalized approach where physicians can actually get the care that they need for their particular issues—PTSD or substance abuse or whatever it is, in a place where they feel like their records are kept confidential, and they receive HIPAA-protection.
This is a free audiobook you can download on my website if you want to learn more about what goes on in the minds of suicidal doctors. I’m happy to answer any questions people have at any time today. And I appreciate your attention. Thank you so much.
This keynote was created based on the book, Human Rights Violations in Medicine: A-to-Z Action Guide now available on Amazon (#1 new release is Medical Law and Medical Ethics). Questions? Contact Dr. Wible here.












I had a friend, Kenneth Gladieux. He was a doctor–a psychiatrist. I knew him before he even went to medical school. I knew him through the bluegrass music community. Over the years, we lost touch, but I looked him up. On Google, the first article listed was his obituary.
Do you have Kenneth Gladieux on you list?
He is not on my list (though registry is not comprehensive).
Thank you for all the work you are doing, it’s about time the information you are providing comes out to light ! I look back and I have no idea how I made it through it all. I do remember put downs, humiliations, discriminations, insecurities. Once During my residency and being awake for over 80 hrs I had decided that I was just going to walk away from it all, but the only thing that stopped me was, that I could not find my car in the parking lot.
I think many of us have experience many horrible situations that somehow we have put away in our minds. It’s so sad ?
Trauma amnesia is what I call it David. Docs figure if they ignore the trauma they experienced (because it’s too painful to face) then medical education will somehow improve on its own. Most docs are shocked to realize the stressors are even worse for the younger generation (debtload, a different EMR to learn each rotation, technology advances, increased patient expectations etc . . .) and this is how we pass our trauma to the next generation. Sad.
Dr. Wible, I think we are cut of the same cloth. Had a [physician] meeting tonight and invited were the State leadership. They gave a brief talk about what they do for us commoners in the trenches. They came to advocacy. With beaming energy I got up and said I like that, advocacy : we need that I said on my soapbox, someone in leadership that yoga, massage, diet, building more resiliency is not the answer: The canary in the mine is sick to the extent he or she is not waiting but jumping out of the cage in suicide, not telling his or her children not to go into medicine. Making the cup of hemlock sweeter is not the answer, lessening the damming penalties might be a start, mandates from CMS, when they do not pay you if you do not use EHRs, then not paying you if you don’t get scores from patients, then not paying if you don’t prove what you do is good based on metrics that are faulty. And all for work already rendered. Recall Mr Slavik-‘ I think we lost the doctors.’ Nuts we’re not lost. He was. Keep up the good work Pam. No, don’t use my name. I do think I touched a nerve, of all the remarks, those above drew applause from the audience, and silence from the leadership. We do not need more toolkits and teflon sprays.
Ah you are my hero! Thank you for sharing. Your secret identity is safe with me.
Oh, Dr. Pam … you’ve done a fantastic job of putting all this data together and presenting it. I have always loved your work, but this is a magnum opus and so, so damning of the industry.
I have a sneaking suspicion that the people at the top of the industry (the elites or the 1%) don’t think ordinary people (the 99%) are worthy of receiving good health care, so they sandbag the doctors in training and hamstring the ones in practice so they can’t escape. They still make sure Americans pay more for medical care than any other group in the world.
Thanks for all that you’re doing!!!
Thank you Yvonne! If you enjoyed the keynote, you’ll LOVE the book. Please let me know if/when you read it. I’d love to talk to you afterwards. So much more to share.
“As a group, medical students are accomplished, capable, healthy, driven, and full of humanitarian impulses when they arrive. How then, does one account for the “1000 yard stares” common among medical residents? This book tells us how that happens and makes some basic suggestions about to resist.
The book is the latest publication by Dr. Wible in a series that examines the abuse and de-humanization that has been permitted to arise in undergraduate and graduate medical education. The singular contribution of this book is that it names and catalogs the instruments of abuse in medical training so that trainees have a written source of reality testing during their darkest days.
In a marked departure from other books that touched on these subjects, this text encourages each reader to record observations that they make at their own institutions. I will go on to suggest that much of the content of readers’ notes should be communicated back to Dr. Wible. Future editions of the A-Z Action Guide will be improved by front line reports of housestaff union formations, wage and hour complaints, OSHA violation reports, abusive referrals for psychiatric evaluations at physician health programs, sleep deprivation injuries to housestaff and patients, retaliation by superiors, participation in patient abuses by upcoding encounters and procedures, forced falsification of work hour logs, and so forth. Just imagine what we are about to hear from the Hahnemann housestaff!
This book will only be improved over the years when medical trainee reports of dealing with EEOC, the US Department of Justice, state civil rights commissions, OSHA, NIOSH, state wage and hour enforcement, and the National Labor Relations Board are aggregated and “best practices” can be recommended.
When I trained, students and residents were routinely-criticized for reading (or worse, carrying around) The House of God. That book was thought to be bad for morale and stood in the way of trainees “getting with the program”. In retrospect, those instances of criticism may well have been outtakes from Full Metal Jacket. Human Rights Violations in Medicine gives the reader much more. It presents a guide (admittedly not yet encyclopedic) about what TO DO about the abuse. Readers should use it, share their experiences, and improve this groundbreaking resource for colleague yet to come.” ~ Tom Horiagon MD MOccH
At 50.5 years of observation/experience, I recognize four main fronts when one confronts life changing circumstances, (a) hostile working conditions (ganging up by people above, peers and below one’s job function) result in helplessness, (b) loss of dearly cherished job/relationship, (c) malicious disrespect etc. and (d) blackmail.
The objective of all four is to isolate a victim from those who can and do provide support. The victim is invariably an ethical/conscientious person who may not wish to wallow with peers who relish in sabotage, betrayal and such myopic endeavors or has engaged in an unethical relationship under intoxication or some other form of relieving stress etc..
Taking one’s life viewed as damage control is worth it only in a conventional battle field, a soldier taking the impact of a grenade to save one’s comrades. In all other scenarios, the overriding priority ought to be, I am an ethical person, taking my life is a loss to humanity. In the overall population dynamics, if the number of ethical people reduce, society becomes a mirage viewed in the context of earnestness, honesty, integrity, honor and such other pillars of society that can withstand any tremor.
Some coping strategies:
– When one is in a hostile workplace, increase entropy of relationships (volunteer, visit public library/museum/concert, engage in sports etc.).
– If confronted with a significant loss or malicious disrespect, levitate from the prevailing circumstances and salvage life by analyzing who is to gain by oneself losing life.
– Blackmail is the toughest challenge, my strategy is to be truthful (my application for Enlistment to the U.S. National Guard and U.S. Citizenship present the bear truth).
The key learning from my life, the challenge to hold the high-ground of intellectual honesty comes in the form of sabotage, betrayal from sources with and without direct conflict/confrontation (mobbing – non-transparent group solidarity to perpetuate fear) seeking every possible way to weaken the victims resolve to hold dear traits like ethics/honesty. Not allowing oneself to be manipulated to be untruthful, unethical may pecuniary wise be challenging, but attaining kinship with one’s conscience is difficult to match (John Adams quote “when my conscience claps…let the world hiss” comes to mind).
In conclusion, it is essential for anyone who is contemplating to take ones own life to think of oneself as an indispensable component/feature of a super-structure which networks living beings. The super-structure desperately needs ethical beings, since such beings do not betray. A loss of such beings weakens the super-structure rendering it vulnerable to a tremor metaphorically and literally speaking. I do not doubt the catastrophic events that have brought ruin to past civilizations fomented by reckless abuse of people and Nature by myopic actions (eg. lifetime of Prophet Moses). From an evolutionary stand-point, life has been down-sized with the notion that smaller beings are more agile and adept to not push oneself to the precipice. Groups of people turn into behemoths attacking the fabric of live-and-let-live may have been the motivation for the movie “Planet of the Apes” by Franklin J. Schaffner, a veteran of the 2nd World War who saw first-hand the carnage embroiled by egocentric power-politics.
Hero. What to think about ending the trauma under circumstance of state endorced repeated legal trauma? How should one think in order to avoid suicide? The children. I must go on for my children. But they have to watch this. They have to live without the proper attention of their mother. The trauma of watching their mother suffer the trauma repeatedly. The gaslighting affects the whole family when the accusation is about mental health. They are going to kill me and I am tweeting instead of doing what I need to do. Im still here but I am not living. I have blind hope in a miracle. Everyday is traumatic.
I think anyone who has sustained trauma within medicine needs a great therapist to help process the abuse and end the cycle.
brutal, yet not the job itself but the inter-personal relationships with authority as the medical profession remains staid and conservative power positions of control. as with the Libby Zion case, the system broke down, and a precious life was lost. sometimes the lies effect the individual negatively, sometimes not and is greeted with a sigh of relief. how to teach those figures of authority to use their non-existent senses to learn something and truly learn to teach. how to make them care.
Univ of New Mexico neurosurgery residents complain to ACGME about how malignant their program is. ACGME does a site visit. ACGME de-accredits the program. This is of particular concern as UNM is really the only consistent neurosurgical resource in the state, so once the attendings start jumping from the sinking ship its going to increase M&M for the entire Southwestern US. Not good.