Last week I delivered this talk twice at the American Academy of Family Physicians Scientific Assembly in Washington DC, and I also presented it to third-year medical students at The Commonwealth Medical College of Pennsylvania. It is fully transcribed here. Every medical student and physician needs this information. Please share widely. You may save a life.  Dr. Wible: Welcome to Physician Suicide 101: Secrets, Lies & Solutions.
Dr. Wible: Welcome to Physician Suicide 101: Secrets, Lies & Solutions.
 I’m a family physician born into a family of physicians. My parents warned me not to pursue medicine. So I went to medical school. Ten years later, I’m unhappy with the direction of my profession (and I’m not the only one). Then I get this crazy idea: what if I ask for help? Not from the profession that wounded me. Just from random people on the street. So I hold a town meeting and ask patients to help me—design an ideal medical clinic. I promise do whatever they want as long as it’s basically legal. That’s going out on a limb.
I’m a family physician born into a family of physicians. My parents warned me not to pursue medicine. So I went to medical school. Ten years later, I’m unhappy with the direction of my profession (and I’m not the only one). Then I get this crazy idea: what if I ask for help? Not from the profession that wounded me. Just from random people on the street. So I hold a town meeting and ask patients to help me—design an ideal medical clinic. I promise do whatever they want as long as it’s basically legal. That’s going out on a limb.
I’m a go-out-on-a-limb kind of doctor. In med school I protest the dog labs and I’m sent to the office of the Dean—who diagnoses me with “Bambi Syndrome.” In residency I’m caught giving patients recipes for kale salad. I’m sent to the office, reprimanded for not getting approval from the patient education committee. I’m 46 and I’m still handing out unapproved kale salad recipes—now I’m taking on physician suicide. My therapist calls me the “Dr. Kevorkian of Medical Taboos.” Before my wedding, my dad actually made my husband promise to keep me out of jail. “Always pushing the limits,” Mom says, “always going out on a limb.” Today I invite you to join me.
Here are the official learning objectives. Bottom line—I need you to take action. I don’t care what you do as long as you do something.
Why do we do what we do? To save lives. Why did you go to medical school? Seriously. Why spend your 20s studying while all your friends are at parties? To make a difference—to save lives. Why are you here? To get CME? See the Smithsonian? Rediscover your joy, your calling? What is your calling? Why are you a family doc? They recruited me for pediatrics, but I kept asking why? Why this kid’s got asthma? Why the parents smoke? Why they live next to an incinerator? I’m a family doc because I can’t stop asking WHY? So why are you here? You had 20 choices, why attend this talk? Maybe you lost a colleague to suicide, a friend in med school. Maybe you are struggling now. Maybe (like me) you just want to know why our colleagues die by suicide at twice the rate of their patients. And you want to save lives.
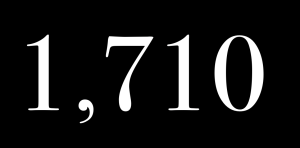
The fact is each year we lose over 400 doctors to suicide—that’s like an entire medical school gone. I lost both men I dated in med school to suicide. In my town, in just over a year, we lost 3 doctors to suicide. One doc in town lost 7 colleagues to suicide! (In what other profession, can you lose 7 colleagues to suicide?!) This year over 1 million Americans will lose their doctors to suicide. Why? To know why someone has died, we perform an autopsy. With suicides, we perform a psychological autopsy:
Today—for the first time—I share my results from 4 psychological autopsies:
This is Vincent. He’s 2. He framed this photo to give his parents at his med school graduation. An adored first grandchild, a joyful little prankster who made everyone laugh. His Aunt Edna told me in catholic grammar school Vincent has his feet up on the chair in front of him. Sister Agnes comes by and tells him to put his feet down. He replies, “I have to keep my legs up!” She asks why. He says, “I have varicose veins.”
Here’s Vincent at high school prom. An athlete and artist, compassionate, sensitive, gregarious, yet private. A compulsive perfectionist. Always a good kid. Never any addictions. Just a straight forward normal good guy, according to his mom.
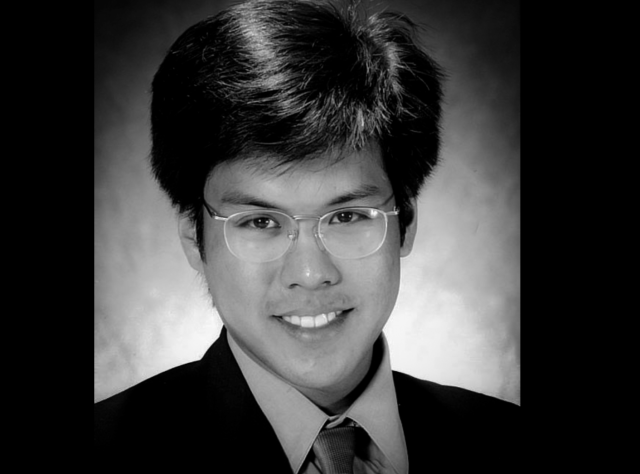
Here’s Vincent’s med school graduation photo—just 25 years old and 2 months after starting a prestigious surgical residency in New York City, he dies by suicide. Why? Look at his eyes. Notice the difference between his childhood photos and his medical school graduation picture. He looked happy and healthy before med school. What happened during Vincent’s medical training? I interviewed several of Vincent’s family members to find out.
His mom says he became disappointed, disillusioned. He lived near the hospital, but drove an extra 45 minutes home at every chance he had just to sleep in his own bedroom. He lost a lot of weight and his jokes and laughs were gone. His family was concerned, but they thought it was the adjustment to a demanding profession.
Vincent told stories of how surgeons publicly humiliated interns. How he and his partner fell asleep leaning against walls in the hospital while waiting for their patient’s turn for a scan. He spoke of his doubts about saving this one guy who jumped out of a building when caught raping a young girl who was also being treated in an adjacent room. He spoke of the sisters—victims of a car accident—brought to the ER, stunned him for a moment because they looked like his mom and aunt who often travel together without seat belts. Vincent took a belt and hung himself in his closet. The note he left:
* * *
This is Greg at 3.
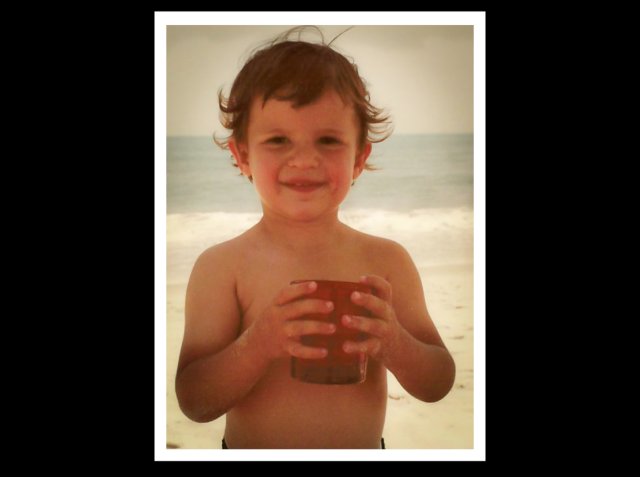
Outgoing, curious and clever. He always got along great with adults. At 5, he goes on this family trip to visit his great aunt—a nun at a convent. A French professor, she asks Greg to give her a word he would like to hear in French. He says, “Guacamole.”

Greg as a child with his mom.

Greg graduating from med school. A pianist, painter, poet, a real Renaissance man much beloved by his patients. Greg sent this e-mail to his parents, both physicians, one year before he died
Subject: Piece of My Mind Read this if you have time. It resonated with me especially well this morning. I like these two paragraphs: I love practicing medicine. Unequivocally. Yet it sometimes seems as much a burden as a privilege. We begin our careers in the anatomy room, a ghoulish lab in which many ‘civilians’ would faint. We cut our teeth in bloody operating rooms and intensive care units from which few people leave intact. We spend our lives bearing witness to the sufferings and diseases of troubled souls. We are well paid, intellectually stimulated, and, if we are lucky, trusted and maybe even loved by our patients. Yet on certain days, when our patients do not do well, the trade-off seems untenable. How are we to protect ourselves from the emotional hazards of the practice of medicine? How are we to stand with our patients through the very worst while avoiding depression, significant stress reactions, and even substance abuse or addiction? Love, Greg
Greg was the only one in his family who struggled with anxiety, depression, and alcohol. After an outpatient program his third year of med school, he was sober until his second year of residency. A brilliant clinician, never impaired at work, but a Physicians Health Program (PHP) mandated a 90-day treatment facility 300 miles away, where Greg felt marginalized, belittled and was 3 months behind in completing residency. He felt if he were a banker or lawyer he wouldn’t have this forced upon him. He hid his depression and substance abuse and carried a lot of shame. Just 24 hours before his death (he had relapsed), he met with his psychiatrist who arranged admission at a local rehab facility. Greg notified the PHP who held the keys to his license. They disagreed with his psychiatrist’s safety plan. Greg felt humiliated, cornered, and killed himself. His mom wrote this letter to the editor of The New York Times in response to a physician suicide article last month. You may recall the article about the two young doctors—interns who jumped to their deaths in late August from their Manhattan hospitals. Greg’s mother writes:
An unacknowledged predicament for physicians who identify their struggle with substance abuse and/or depression is that they are often placed under the supervision of their State Medical Board’s Physicians Health Program. My son, Greg, was being monitored by such a program. He took his own life at age 29, one week before he was to enter an esteemed oncology fellowship. His final phone calls were to the PHP notifying them of his use of alcohol while on vacation, a disclosure he had previously described as a ‘career killer.’ These programs, which often offer no psychiatric oversight, serve as both treating and policing agencies, a serious conflict of interest. Threatened loss of licensure deters vulnerable physicians from seeking help, and may even trigger a suicidal crisis. Medical Boards have the duty to safeguard the public, but the assumption that mental illness equals medical incompetence is an archaic notion. Medical Boards must stop participating in the stigmatization of mental illness. We cannot afford to lose another physician to shame.
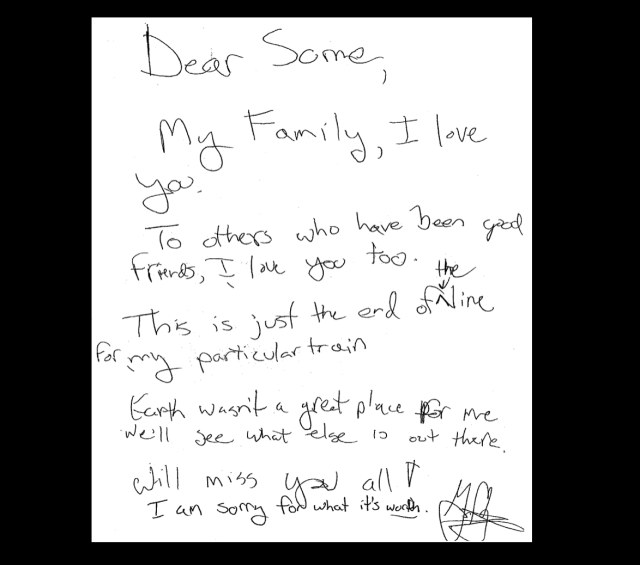
I read 12 pages of online condolences. This anonymous entry stands out: “Thank you for being nice to even the unpopular kids in high school. May your soul rest in eternal peace.” Greg looked out for the underdogs, but what happens when doctors are considered underdogs? Who looks out for us? Do we get the care we need? Greg didn’t. Greg transected his bilateral radial and dorsalis pedis arteries with a scalpel in the bathtub, candles lit, music playing, some wine, vodka, surrounded by family photos. Greg’s note:
* * *
This is Kaitlyn and her mom.

A sweet, good girl. Kaitlyn never gave her parents any problems, though she cried when she lost at Monopoly. From the time she started preschool, she never needed any help with her homework or anything. At 3 years old, she had to get glasses. Her parents took her to the big medical center where the doctor asked lots of questions. He’d look at the parents for answers, but Kaitlyn answered them all. The doctor was amazed.

This is Kaitlyn in high school. A deep thinker, an artist, a poet. I met her extended family in North Carolina. They claim, “Kaitlyn was one of the happiest people on this Earth.”

Here’s Kaitlyn in med school. Just 23 years old and beginning her third year. An introvert with social anxiety, Kaitlyn always had a few close friends, but none in med school. Everyone was busy studying and “people just went their own way,” she told her mom. She was desperately lonely. Her perfectionism worsened. She went on a strict diet, started running marathons, and lost a lot of weight. She ran like 10-12 miles before class everyday and still excelled in med school, acing her Step One exam. Unfortunately she didn’t live to celebrate her results because she completed her suicide—a helium overdose—like a well-planned school project. She left a 2-page suicide note in which she claimed lifelong depression, but hid it to protect her family and herself.
As an aside, I believe that Kaitlyn suffered less from depression and more from “feeling different and isolated” due to her high intellect. She was raised in the poorest county in North Carolina was the smartest person around. Maybe she had hoped that when she entered medical school she would finally be with her tribe—a social circle of more like-minded intellectuals. But medical school rarely creates an environment for students to develop intimate friendships with one another. These young sensitive and brilliant people are left to fend for themselves in survival mode with an overwhelming amount of material to master in a short time with little emotional support. I can guarantee that many medical students cry themselves to sleep at night in their pillows. That’s what I did nearly every night my first year of medical school. I cried so much that one morning my eyelids were sealed shut. I couldn’t see anything when I woke up. I had to feel my way to the bathroom. Is this they way a civilized society trains its healers? Kaitlyn’s mother published her daughter’s suicide letter in a book she wrote about Kaitlyn. An excerpt:
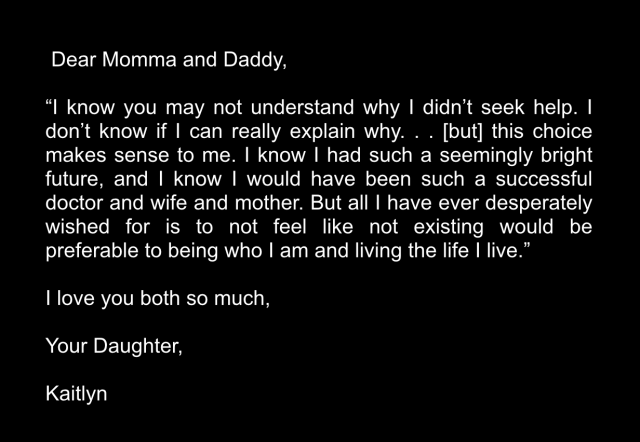
Kaitlyn’s grieving mother—unable to recover from her daughter’s death—died by helium overdose one year later. I attended her funeral last month.
* * *

Here we have a spunky, happy 2-year-old girl who stood up to adults negotiating her way out of a bedtime, a bath time, and persuading her dad to get Slurpees and candy bars for dinner. Life was good until her first year of medical school.

Just a few months into med school she develops major depression due to what she calls “barbaric and inhumane medical training.” Years later, fed up with assembly-line medicine, she’s suicidal. The only difference between these cases is she survived and she’s on stage speaking today for the other 3 who can’t.

* * *
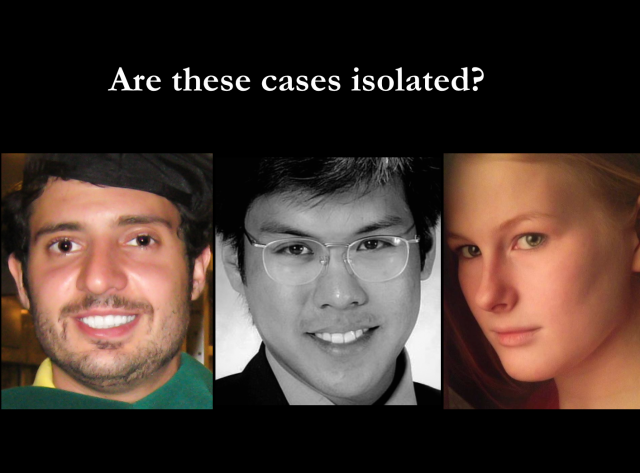
Our cases are not isolated. All brilliant, sensitive people who felt alone in a highly competitive and inhumane environment. All sleep deprived working or studying over 80 hours week. All hid their depression and appeared highly functional until their suicides and all left notes because we’re trained to do and we’re so darn responsible!
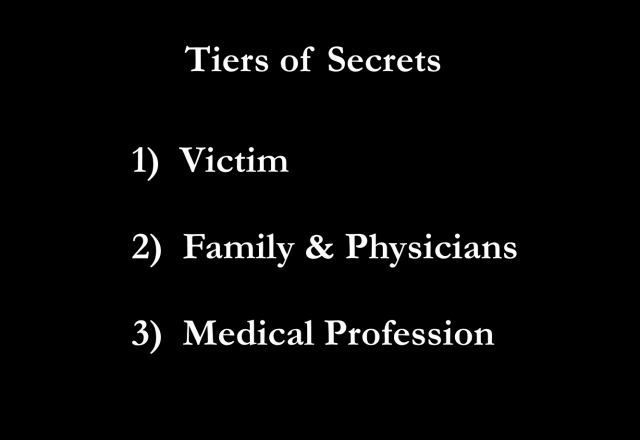
The secrets start with victims who are ashamed. Families remain silent to safeguard their reputations. Physicians hide suicides from patients who never find out why they can’t get a follow-up appointment with their doctor who left the clinic so suddenly. Physician suicide is medicine’s darkest secret and our code of silence is maintained by layers of lies.
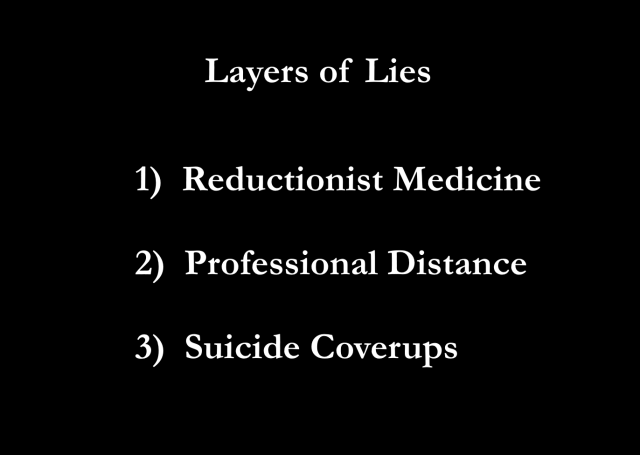
Reductionism is the opposite of holism. Reductionism leads to body-mind-spirit disintegration. While reductionist medicine has led to scientific advances, it’s fatally flawed. It separates us from our hearts and souls which is what gives our lives meaning and keeps up wanting to live here on Earth. Professional distance is far from protective. Vulnerability is strength. When we’re authentic with our patients and ourselves, we build resilience and connections with other people here on Earth. And the suicide coverups . . . 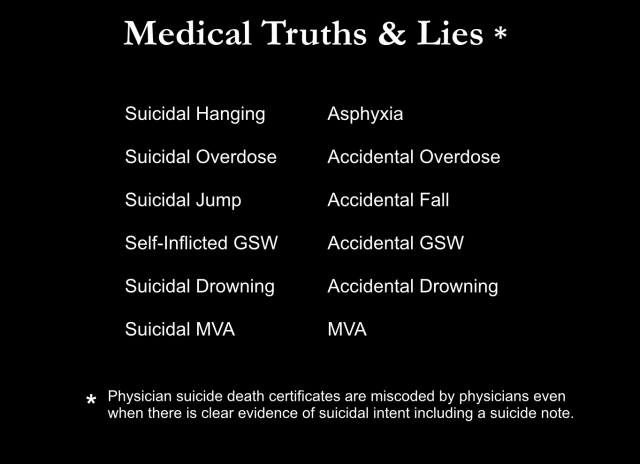
It’s a medical game of truths and lies. Death certificates are miscoded even when there’s a suicide note! A suicidal hanging becomes asphyxia, a suicidal overdose is suddenly an accidental overdose, a self-inflicted gunshot wound is officially an accidental gunshot wound, a suicidal motor vehicle accident is just another motor vehicle accident.
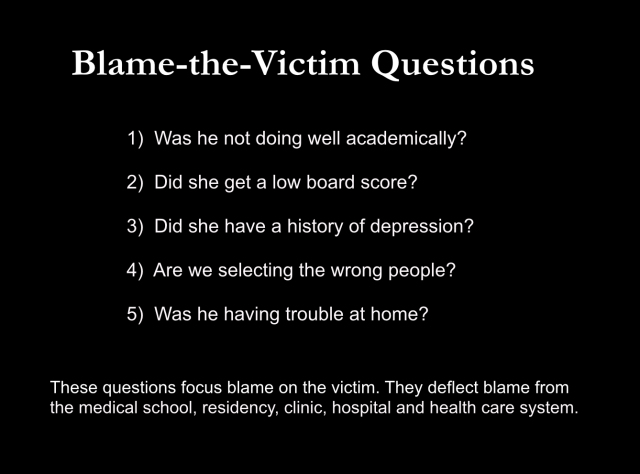
Meanwhile those in the know whisper blame-the-victim questions: Was he not doing well academically? Did she got a low board score? Are we selecting the wrong people for medical school? These questions focus blame on the victim, not the health care system.
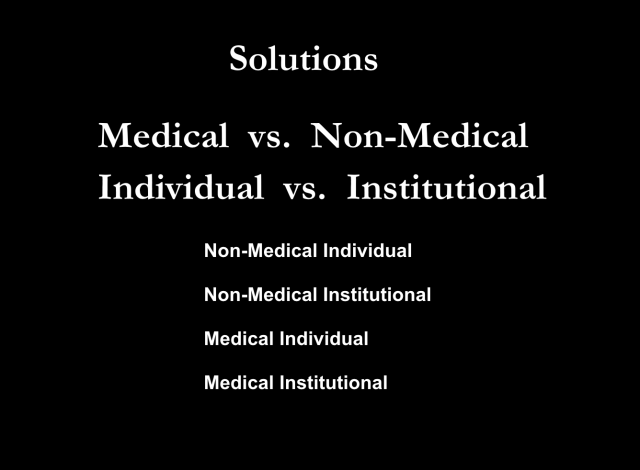
So what are the solutions? Solutions come from individuals or institutions inside or outside of medicine.
Non-medical individuals—the general population of non-physicians. Except for Greg’s parents who are aware of the occupational hazards of medicine, families had no idea their child was at high risk of suicide until the police called to tell them their child was dead. Compelled to act, Vincent’s mom starts a foundation that sponsors an annual lecture on mental health for residents at Vincent’s school. Kaitlyn’s mom writes her heart out online in a blog and on social media sites. She supports struggling medical students online. Ultimately she publishes a book examining suicides in the exceptionally gifted like her daughter. She asks all 171 medical schools in the United States if they would like a copy. Thirty got a copy. Should we rely on grieving mothers—suffering in isolation as were their children—to solve this?
Non-medical institutions like the media could instantly stop the secrecy and alert the public about the high risk of suicide in medical students and physicians. Because sending your child to medical school or a surgery residency is not like sending your kid to law school or to cashier at Walmart. It’s more like sending your kid to Iraq or Afghanistan and it requires a completely different level of vigilance. I spent two hours on the phone with Kaitlyn’s dad the other week. A sweet, sweet man. Not the kind of guy who would ever blame anyone else for his problems. I asked, “If Kaitlyn worked at Walmart, would she and your wife still be alive?” He says, “Yes. Medical school has cost me half my family.”
Medical individuals—that’s me and you questioning these deaths, and Greg’s mom seeking audits of PHPs for fraud and abuse.
Lastly medical institutions. Kaitlyn’s school started a fund in her name for donations to their wellness center so that presumably Kaitlyn’s classmates could seek the help that she didn’t. Vincent’s yearly lectures continue. But what else can we do?
Let’s compare how we handle physician suicide with say. . . umm . . . human rabies. Since the 1900s, annual human rabies deaths in the US have gone from 100 to just 2 per year. How did we do this? Not by grieving mothers launching “rabies awareness campaigns.” Not by donations to a wellness program. Not by a yearly lecture series. And not by miscoding rabies deaths as the flu!
Here’s how we did it: medical institutions took this on methodically using science—primary, secondary and tertiary prevention strategies.
We spend over $300 million annually to prevent human rabies. The cost per human life saved ranges from $10,000 to $100 million. What do we spend on medical student and physician suicide prevention?
Since eradicating the terrestrial canine rabies variant in the US, 90% of the 2 deaths per year are transmitted from wildlife—mostly bats then raccoons. If we can deliver over 6 million oral rabies vaccine baits yearly to raccoons (and I’m talking about guys dropping these from low-flying planes over the Appalachian Mountains and dudes running through dark urban alleys), we’ve gotta be able to do something for med students. Right? We’re way easier to find than raccoons. We’re already in the hospital!
Right now while I’m standing here on stage we are actively tracking rabies in raccoons, bats, skunks, foxes, cats, dogs, cattle—even mongooses in Puerto Rico, but we’re not tracking the numbers of suicides in medical students and doctors. Do you ever get the feeling you might be less important than a Puerto Rican mongoose?
Here’s what scares Kaitlyn’s dad. Now I want to preface this with something else I learned about Kaitlyn’s mom who also suffered from depression. I asked Kaitlyn’s dad when his wife developed depression. Get ready for this. He told me it was after she completed nursing school in her 30s when she worked in a nursing home with a high census in which she was witnessing unsafe conditions for patients—and staff. She was normal before nursing school. Okay. Normal. Like medical students who start med school with their mental health on par with their peers. Then something happens during medical training to doctors—and nurses.
This is what really scares Kaitlyn’s dad. He tells me, “I got one child left. She’s in nursing school. I hope she’ll beat the odds. I can’t handle another.” This man has a real risk of losing more people in his family than we lose in a year to rabies! What are we doing? For him? For medical students? For us? Here’s what we should be doing:
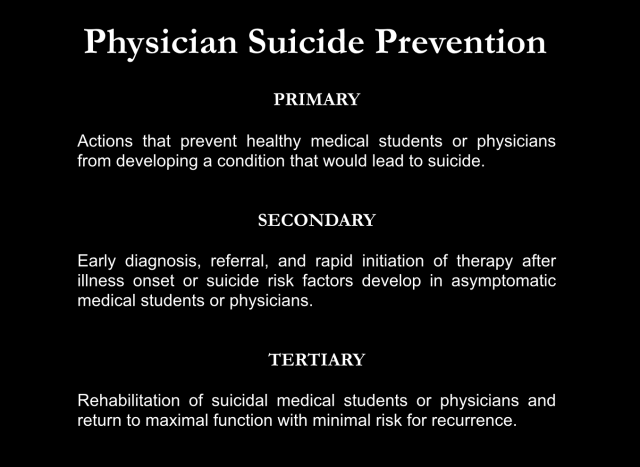
First: prevent healthy medical students and doctors from getting conditions that lead to suicide. Second: Early diagnosis, referral and therapy. Third: help suicidal medical students and doctors rehab.
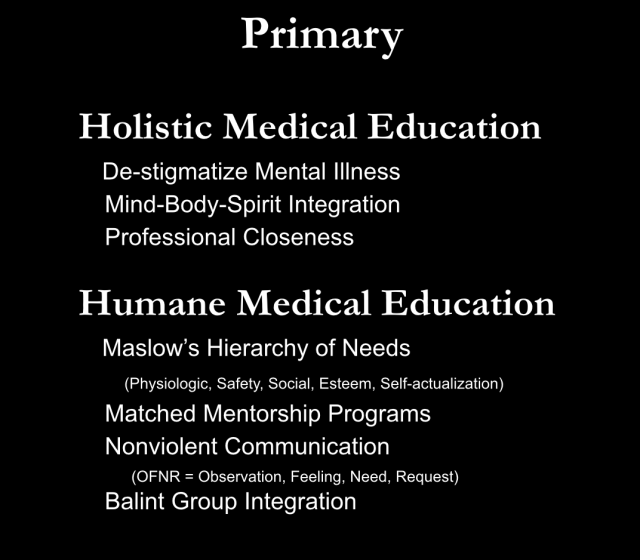
Let’s start with a holistic and humane medical education that de-stigmatizes mental illness.
The goal: help medical students be the self-actualized doctors described in their personal statements for which they were accepted into medical school in the first place. We know how to grow happy and healthy people. This is not some sort of secret. Follow Maslow’s Hierarchy of Needs. Begin by meeting physiologic needs with adequate sleep, time to eat and bathroom breaks. Simple. Basic. Ya know? Meet safety needs with a safe workplace without bullying or abuse. Social needs can be met by allowing students to feel part of a community with time for intimate friendships. And finally, self esteem needs. Medical students should feel honored and respected for their contributions and level of mastery in medicine. Not belittled. Not shamed. Not pimped. Not hazed. This is 2014.
Meet social needs with Matched Mentorship Programs. Use match.com technology to match first year medical students with second years—and physicians within their specialty of interest. Match Day should be the first week of medical school. Don’t wait until fourth year for Match Day. These people need friends. Now. We should not allow medical students like Kaitlyn to die from extreme loneliness. Meet safety and self-esteem needs using nonviolent communication (NVC) which is based on the premise that every behavior is an attempt to meet a need. We can try to change others’ behaviors by using shame and blame or we can listen and educate compassionately. If you hear a doctor raise his voice at Vincent, would you pass by unsure of what to say? Meet the conflict with confidence using NVC using a simple 4-sentence sequence—a stated observation, feeling, need, and request.
Observation: I heard you speaking loudly to Vincent. Feeling: I feel concerned, because . . . Need: I need everyone be respected in this hospital. Request: Would you be willing to lower your volume and speak with more consideration for Vincent’s feelings?
Meet social and self-esteem needs with Balint groups. These are small group clinical case presentations that focus on the patient-physician relationship and enhance our ability to care for patients. Balint groups are usually led by a doctor with some experience in facilitating these groups and/or a psychologist/counselor. These groups are easy to start. If you want some training, I’d recommend the American Balint Society. Has anyone here ever done a Balint group? (Lots of family docs raise their hands in the room).
If Vincent could have attended a Balint group, he might have shared, “This week I saw a 30-year-old male who presented with injuries after jumping from a 3-story window after raping a young girl. I was tachycardic and I had trouble maintaining eye contact . . .” Vincent would have the chance to share feelings and get feedback in a safe environment. Offer Balint groups at lunchtime and meet physiologic needs too since students do need to eat! Ya know, give them a Subway sandwich or something to share.
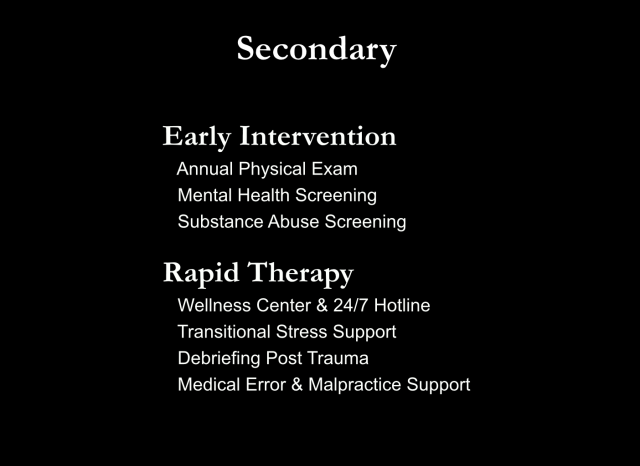
Early intervention begins with a yearly physical. In Kaitlyn’s second-year physical her doctor might have said, “I see you lost 20 pounds since first year and you’re getting up at 5:00 am to run 10 miles before class. How are things going for you?”
Every medical school needs a 24/7 helpline staffed by medical students. We learn to do blood pressures, ear and throat exams on each other, let’s learn emotional support too and give first and second years the real-world experience of being on call—for each other. Build in support for transitions from second to third year, traumatic cases, and medical errors. We’re all going to make an error and we should not have to feel like a failed perfectionist who can never be a good doctor. Again, medical students and physicians should not be left to cry themselves to sleep in their pillows alone at night with no support. That’s inhumane.
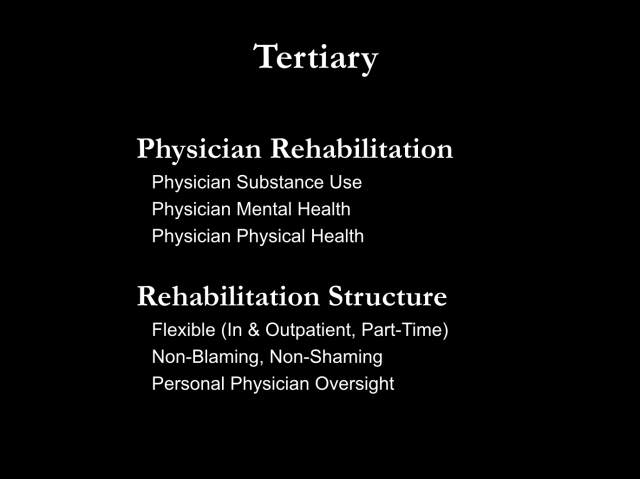
We need physician-specific rehab for substance use, physical, and mental health issues that are unique to physicians and medical students. Even medical students and residents with physical ailments feel ostracized from the group. The message usually goes something like this: “Let us know when you’re off the ventilator so we can put you back on the call schedule.” What kind of support is that? Rehab should be flexible, in town, with part-time work options. You know what kept Greg from drinking? His work. He loved working. Why send this excellent doctor 300 miles away? Greg shouldn’t leave town for inpatient rehab if local, output rehab is effective. And rehab should be non-shaming. When Greg called his mom (a psychiatrist) for help, his PHP therapist said, “Oh, you had to call your mommy?” What kind of treatment is that? We need personal physician oversight so our vulnerable colleagues are not abused and traumatized when they need help.

Would they be alive today? YES. Their deaths were 100% preventable. Every day we don’t take action, we lose another Kaitlyn, Vincent, or Greg. So what will you do?
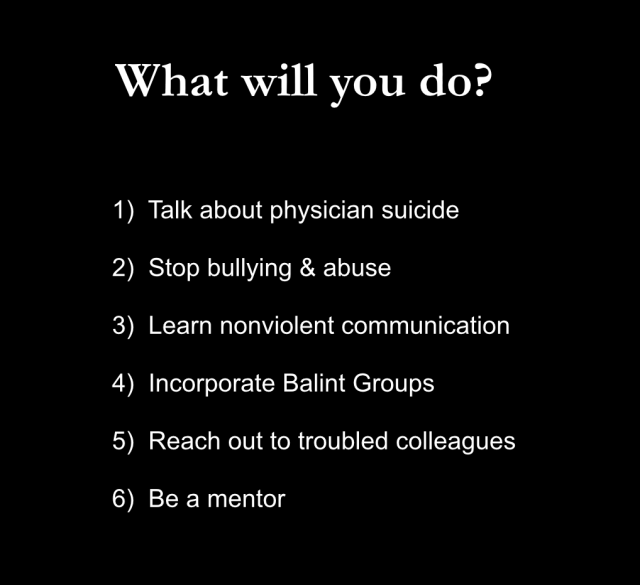
1) Will you talk about physician suicide? If you lose a peer, will you hold an M&M conference or perform a psychological autopsy? A group of cyberspace docs recently asked me, “What gives you the right to perform a psychological autopsy? To go through these victims’ autopsies and suicide notes?” Well, these families reached out to me. I didn’t go looking for this. I didn’t even know I was doing psychological autopsies until I discovered the term in a suicide article. FYI: families with suicided children are eager for someone to take a sincere interest in their kids’ deaths. Would you be willing to honor their children? And prevent future deaths among your peers? Another gang of cyberspace docs wanted to know what kind of training I have that allows me to do these psychological autopsies. Do I have some sort of certificate that gives me the right to do this? I have no training. But my mom’s a psychiatrist. My dad’s a pathologist. Maybe that means I’m a natural at psychological autopsies. What training do you really need? Just take an interest in your dead colleagues. The only question you really need to ask is “WHY?”

2) Will you stop the bullying and abuse? We can all reach out to faculty who use shame-and-blame teaching, call attention to the violence, and offer alternatives. We do not need fear-based teaching to learn how to be healers.
3) Will you learn nonviolent communication? Vincent was inserted into violent crime scenes. Why speak violently to one another? NVC can reduce the trauma of our traumatic jobs. Let’s learn and then teach NVC. It’s easy. I learned in an hour online. Plus my ex-husband’s last girlfriend teaches it and I hired her for a private lesson. Takes about an hour—or at max two. Every medical school, hospital, and clinic should teach their students, physicians, staff—even administrators and CEOs how to speak with kindness and compassion.
4) Will you start a Balint group? All medical students and physicians would benefit from a weekly lunchtime case conference, a structured release valve for the trauma they have witnessed. Vincent and his peers could have processed their feelings and eaten. I teach a biannual physician retreat in which physicians often (spontaneously and without prompting) start crying about cases from years ago. One doc in her late 50s broke down about a miscarriage she witnessed over 20 years ago. She was just so happy that she could finally cry about it! She hadn’t been able to cry in years. Really? We’re just supposed to just shove all this down day after day, week after week, year after year with no release valve? You can’t tell your spouse. Cases are confidential. Plus you’ll wear out your spouse. There’s a reason most people don’t go into medicine. They can’t handle this stuff. We can IF we have a way to process our feelings in real time before we start plotting our suicides. Please (I’m begging you) start a Balint group in your clinic or hospital. You could save lives.

5) Will you reach out to troubled colleagues? Doctors like Greg won’t just come up to you and say, “I’m suicidal.” But he might say, “I had a rough day.” (That’s doctorspeak for I NEED HELP!) When docs e-mail me their troubles, I call them back immediately. Sometimes 30 seconds after they hit the “send” button on their computers. They’re shocked. I respond,” When you’re on call, you call patients immediately. Right? Why don’t we do that for each other?”
6) Will you be a mentor? At the time of Kaitlyn’s death she was dating a man in Michigan who was a 99% match on OkCupid. Kaitlyn needed a matched mentor in her own town—at her own school. Someone to watch over her. Could that have been you?
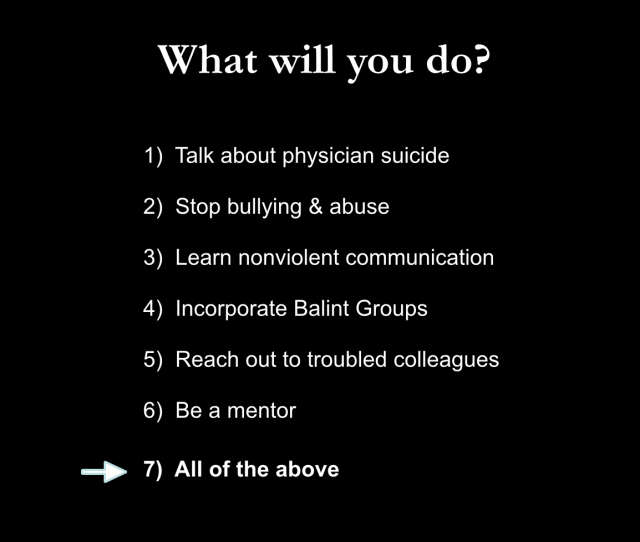
There’s so much we can do. I don’t care what you do as long as we do something. So will you go out on a limb to save a doctor? To save the people who dedicate their lives to saving others? And if you are suffering, will you seek help? Standing at the town meeting, I went out on limb. I didn’t just tell folks I was an unhappy doctor. I told my entire town I was depressed and suicidal. I begged strangers to help me design an ideal clinic. And define an ideal doctor. I had lost my way. They told me an ideal doctor has a big heart and a great love for people and service. And an ideal clinic is a sanctuary, a safe place, a place of wisdom where we can learn to live harmlessly, listen with empathy and observe without judgement. It’s a place where a revolution starts where we rediscover our priorities with relaxed appointments, smiley-face balloons and fun flannel gowns—a lady at the town meeting even volunteered to make them for me. Then a bearded guy in the back of the room raised his hand and asked a question I’ll never forget, “Is it possible to find a doctor who’s happy?” I collected 100 pages of written testimony, adopted 90% feedback and we opened one month later. That was 10 years ago. I’m happy now. All because I asked for help.
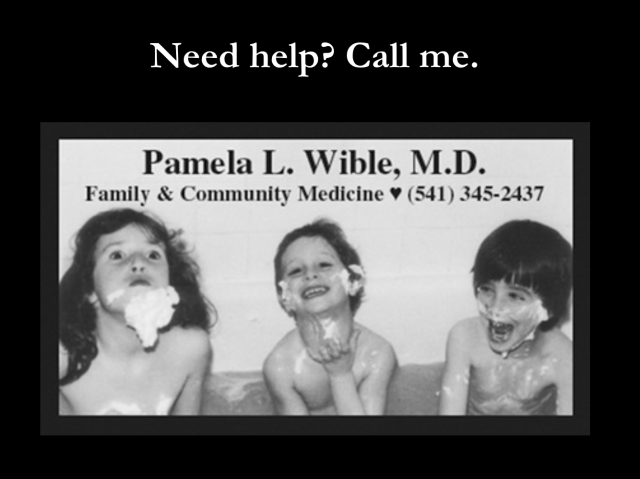 Pamela Wible, M.D., pioneered the first ideal clinic designed entirely by patients—the original “Patient Centered Medical Home.” She was once a suicidal doctor and now dedicates her life to helping medical students and doctors who are disgusted with, depressed by, and feeling suicidal about their once-beloved careers in medicine. There is hope! Come to the next physician retreat (premeds & med students welcomed). Learn more about the ideal medical care movement in Dr. Wible’s TEDx talk.
Pamela Wible, M.D., pioneered the first ideal clinic designed entirely by patients—the original “Patient Centered Medical Home.” She was once a suicidal doctor and now dedicates her life to helping medical students and doctors who are disgusted with, depressed by, and feeling suicidal about their once-beloved careers in medicine. There is hope! Come to the next physician retreat (premeds & med students welcomed). Learn more about the ideal medical care movement in Dr. Wible’s TEDx talk.












To value ones own life we need to grow spiritually from a machine called doctor to an awareness which feels great enabling others to benefit from ones own life.
Nobody is looking for a zombie robot doctor. This is too often what modern medicine delivers to patients.
In Greg’s handwritten letter we see upward slant in the beginning as if to say that everything is okay as he relates to family and friends. But at the very end his demeanor has taken a depressionistic overture as the handwriting begins to slope downward. But the biggest indicator of all is how he has X’d out his name in his signature. That is not a final act but can be recognized months in advance and is a warning sign that someone needs to intercede.
Have never even thought of using handwriting analysis as an early (or late) predictor of suicide.
Greetings, I am currently working on resource brochures for first year medical students in our recently established medical school. I am gathering information to include in the suicide prevention pamphlet at the moment and would like to know if there is anything in particular that you would recommend. Thank you
Please send me what you create and I will help you hone it. I’m also happy to speak to you. I have LOTS of ideas! Use my contact link in nav bar to writ me.
What a great idea to work with!
OMG just came back to this while checking out one of your emails. Can’t believe it’s been close to two years since this post. I added a section on handwriting analysis as it applies to suicidal tendencies.
I didn’t read it all tonight, but so much that I laughed and cried too. I decided to pursue nursing after meeting you. You inspired me, and continue to. But now I am thinking of learning a new trade. why not?
Thank you for mentioning the dysfunctional and unqualified state PHPs under the FSPHP. Many are afraid to for fear of being targeted themselves. After all this is the group that set up the scaffold, widened the scale of the hunt and decides the fates of individual doctors who cross their paths. PHPs have been granted unrestrained managerial prerogative and absolute power over all of doctors. They decide not only who to monitor but how that monitoring proceeds in every last detail. Our fates, literally, lie in the hands of this group. No more physicians should die by this system of institutional injustice, bullying and pseudoscience. The conflicts-of-interest are abhorrent and would be incomprehensible in any other venue including any other branch of medicine. It’s all opaque, secret, and hidden. It has to be or we wouldn’t allow it. Isn’t it time we take charge? And the solution is fairly simple. Oversight, regulation, and auditing by OUTSIDE groups. That is how it’s done everywhere else. Why do these guys get a pass? Accountability is a rule not an exception. But those OUTSIDE the system must speak up. Those already WITHIN the system are marginalized, dehumanized and deligitamized. The accusation of substance abusr or a behavioral issue is used to disregard the claims of that person. The PHP “silences” them in this way. And there is no one to complain to. Feeling helpless, hopeless and entrapped many are taking their own lives. We need emergent ombudsman for outside oversight at a state level then transparency, oversight, regulation and accountability. This is critical to save both doctors lives and the very future of our profession
Well said, Michael!
Thanks Chip- how are ya? Give me a ring sometine
Love that I am reconnecting old friends through my suicide lecture. Yay!
Unfortunately,I have to agree with everything you have said.
Really a great article. I had never heard of the suicide rate in med school until my daughter started at TCMC last year.
Thank you so much for sharing this. Even though my beloved son wasn’t in the medical field, I’m always constantely looking for why. I also lost my mother to suicide when I was just 15 years old. My son’s 2 year anniversary is Nov. 26th and I was fb friends with Kailyns mom… I so miss her. If I’m being honest, I’ve struggled so hard within the past almost 2 years after losing my beloved son. It gives me hope that someone with your ability is trying to get something done. We have an epidemic that most don’t care to discuss or be a part of solving.
And yes, I do think we are more important than animal studies as well. Thank you so much for giving me hope.
I’m so sorry for your loss. Thanks for sharing your story. Be brave, be hopeful, be strong…
Michelle
I am really very sorry for your losses. I am not a physician, I am a psychologist and executive coach, and live in Mexico City. I’d like to share that upon reading Pamela’s article, my thoughts linger towards one word: perspective. There is such a huge world of possibilities out there… And a myriad of options and opportunities for re-designing our life, over and over again, throughout our lifetime. We can always choose again. Everything…. Yes, everything. The rules by which we accept to govern our life and our activities, is included. We have a huge world out there, with endless possibilities and needs to be met. Outside of US borders too.
I highly recommend the book Lifelaunch, by Frederic hudson and Pamela Mc Lean.
Best wishes to you.
It sounds so simple to say “change everything.” People who go to medical school are carrying high expectations of themselves as well as their families’ high expectations. A depressed physician seeing the career as a “dead” end (the stress, the suffering you see, the over-regulation you have to handle, the lack of support to be anything other than what you are, the lack of help from your peers, the risk of losing patients from time off, the income necessary to maintain lifestyle, etc.) would shrug off that suggestion. After 7-12 years of training after college often with debt, it is not easy to start over. Dr. Wible’s concept of changing the medicine is probably more palatable.
Thank you for surviving and doing this; I started med school in 1978, I finished in 1989, while I formed a family, I had many crisis and difficulties, from med school 1st year, I said i would never go back to the cadaver labs, 25 years later and with a specialty and doing what I like, last night I woke up thinking of a patient or two… 5 am, could not go back to sleep, what if I get it wrong? Suddenly it seemed like an unsurmountable mountain… yesterday a 27 y.o. woman died after a short illness, I was not her doctor, only hear the story, it was enough…
We do get it wrong sometimes. And we make mistakes. Hopefully there are many more saves than losses. We do not make the illness happen (usually). Patients often ask “why me?” when they get sick. Why anybody? To expect to be perfect is to expect to be more than human. Your note is classic doctor anxiety.
The life of my friend, the late Rhonda Sellers Elkins, has finally come full circle with this tour de force article addressing the largely-ignored problem of suicide in our medical schools and among stressed-out workers in the medical profession. A tireless advocate for bringing greater knowledge or awareness to the concealed threat of depression that claimed her 23 year-old talented daughter in medical school, Rhonda would be so very pleased that Dr. Pamela Wible, M.D. has carried on with her mission to prevent suicide among those who struggle to keep others alive.
Dr. Wible, thank you so much for your tireless crusade to educate educators, mothers, fathers, brothers, sisters and all about physician suicide prevention. Rhonda Sellers Elkins was my beautiful sister, whom I miss very much. She just could not go on in life with the guilt of not being able to see the lifelong depression that her daughter, Kaitlyn suffered. Unfortunately, with Kaitlyn’s depression, she chose the profession that was probably the worst she could have chosen.
Everyone needs to know what goes on in med school and you, Dr. Wible are truly making a difference. I say thank you.
Thank you Gail and (as you probably have figured out by now) I will continue to honor the memory of these brilliant and talented people who died far too soon of wounds inflicted by (or at least worsened by) the health care system and its inhumane training and working conditions. There is a way to train healers without harming them. The people who choose helping professions should be honored and supported emotionally. Not left to fend on their own. We all come to medicine with pre-existing wounds. But the career should build resilience and strength in our healers, not destabilize them. We can do so much better.
Wow. Just, wow. I had no idea. And I thought I knew a lot about suicide and mental illness, having been the leader of a local NAMI group for three years, after my daughter’s major depression and suicide attempts in high school.
As a nation we are just beginning to seriously address the problem of suicides in the military, and learning a great deal about the effects of stress, mental illness, and the difficult transitions these very young people are going through. Maybe some of the research there could benefit this effort. And maybe some of these excellent suggestions could be adapted for use within the military.
We were able to get my daughter help and healing; she was still at home when life got overwhelming for her. Unfortunately I can’t say the same for my cousin’ daughter, a soldier, Seargent Jessica Jackson Barnett, who died by her own hand on August 15, 2014, at 21 years of age, leaving behind a devastated new husband and grieving family.
Keep up this important work. The only credential you need is a heart.
That is so true.
The only credential you need is a heart.
i am not a doctor, but i grew up in russia. yes, america has more money, better healthcare/etc.
but americans are such cold assholes to each other. russia, people-wise, was much better and warmer. its a robotic, cold, competing, calculated society that drives a lot of people up the wall, into depression with its stress. if you arent a doctor/lawyer/you are a failure. images of millionaires/billionaires are everywhere in american media.
it literally all makes u go crazy.
“Our scientific power has outrun our spiritual power. We have guided missiles and misguided men.” ~ Martin Luther King, Jr.
I love this quote; I will use it in a paper I am writing on the topic of dignity, for my masters in bioethics.
Pamela, I love your work! In all my years as a psychiatrist, I have never known any physician to take on this topic publicly and with such personal transparency. In psychiatry, we are taught an extensive array of risk factors for suicide; I think it enables us to avoid taking on patients at risk as it reduces our potential liability…sad reality.
This guy is spot on. It is terribly isolating here. Maybe people with large families do better, I don’t know. I am married from outside my culture and I can’t tell you how amazing it is having his family around me despite how emotional they seem to me. In fact, I am even thinking about relocating to a developing nation just so my kids (and myself ) can have a normal social/emotional/spiritual life with extended family. Our culture is so individualistic to an extreme that I think it goes against our nature (but good for capitalism and the economy). I would not have realized this unless exposed to something different. I think being too educated can also be very isolating and that is where being close to family really helps. I can’t help but think if these medical students you speak about had their families around them- perhaps things would not have resulted in the same manner. I am not saying it is anyone’s fault. We are trained from a very early age to be independent. It is what for generations we are taught is expected from us and normal. My sympathies to these people’s families.
Thank you Dr. Wible for the work you do! I had never read such a profoundly disturbing yet necessary and thoughtful expose on physician suicide. I am a family medicine physician whom has suffered from depression myself, particularly starting during my first year of residency and intermittently throughout my career. The demands of assembly-line medicine can take it’s toll. My heart goes out to the family and friends of those you have profiled and the countless others not mentioned. As physicians we have a duty to reach out to others suffering so and to stand up for change in a profession that seems to have turned a blind eye to it’s own.
First they came for the Socialists, and I did not speak out—
Because I was not a Socialist.
Then they came for the Trade Unionists, and I did not speak out—
Because I was not a Trade Unionist.
Then they came for the Jews, and I did not speak out—
Because I was not a Jew.
Then they came for me—and there was no one left to speak for me.”
~ Martin Niemoeller
If doctors and medical students do not start standing up for each other and ending this cycle of abuse, “health care” will continue to decline. We are of little use to our patients if we are plotting our own suicides during their visits. Enough is enough.
A society will soon fall when its healers are harming themselves.
Pam, I’d like to do some deep research and possibly publish a paper with you on this topic. Are you already working on something or would you be interested? I’d love to get into the statistics and data that is out there and prove to the world that what you are saying is without a doubt true. We could start with death certificates of doctors who have died under questionable circumstances. Let me know what you think. -Tracy
Love to! And I am working on something now. More data needed.
Pamela and to Tracy Kritz,
I can attest to one Dr. Frank Ruiz, Tucson. He was my one of my Doctor’s who performed my cancer operation year’s ago. I believe the paper say’s cop assisted suicide. I hadn’t seen him in year’s but we found out while looking for him to evaluate me, and rule out any return of cancer. His current patient’s were shocked. None had a clue. What a burden to have to carry the weight of your patient’s, and also to live in solitude with depression. I think the whole mental health system needs re-evaluated. There is no therapy in the traditional standard’s. It’s another pill mill, and a diagnostic web of stigmatizm’s. My mother had to live most of her life in and out of institution’s after being heavily sedated, and titled. The real life struggle behind it all was that she had lost all of her children to a man who knew how to get away with the most heinous crime’s against humanity. Him and his new wife made sure that she was only ever understood as “mental”. After his passing my Mom was finally able to have conversations without fear. We even discussed the issue with institutions, and how she felt safer there at times. It was only recently when I discovered just what we both had survived. I lost a sister at age 16. When my mom had said my Dad did it. I assumed like most it was her mental illness speaking. I had no clue my Mom was right. Sad thing is that the stigma of mental illness act’s as a cover for so many underlying causes. Often those causes are thing’s which society would prefer stayed hidden. I’m very saddened by reading the oppression that medical student’s, and Doctor’s face. Nobody really know’s what it’s like to wear those coats. I guess we see Dr.’s like Giant’s. We seem to forget they are human too. I’m very grateful to know the truth. So much in this article is helping me to understand what happened here in Tucson with so many Dr’s. who were basically ran out of town. One was so openly bullied that his torment’s made news in social media. It was outrageous., and yet he was so loved by his patient’s who went to bat for him. An online petition was written to address the board of regeant’s, ect. Him and other’ well-loved Dr.’s which faced similar issues. It’ seems Tucson doesnt like innovation, and/or Dr.s who love their patient’s. I’m glad you escaped Pamela. I’m so proud your following your heart, and doing what you can to inspire other’s to do what they can as well. Much love to the both of you. I just know your contagious spirit is infecting many!
Pamela,
I am still stunned and, dare I say, grief-stricken, hours after reading your extraordinary presentation and call to action on physician suicide. Your courageous self-honesty and your ability to cut through the mesmerizing psychobabble of monotone clinical presentations on suicide are awesome, and so refreshing.
While the boot camp mentality of earlier eras of medical training was brutal, there was at least some thread of community, and pride in identification as a physician. Now, with corporatization of healthcare, nearly complete loss of the doctor-patient relationship, and punishing forces coming from all sides (litigation; payers; government; patients turned demanding consumers; even our own medical boards and PHPs), both the sense of community and the very identity of being a physician have all but vaporized. No more collegial grand rounds or M&M conferences; no “journal club.”** Just a relentless stack of administrative tasks and regulatory demands on top of a loaded schedule and ever briefer and more cursory patient visits (“one complaint only”) where physicians devote more eye contact to a computer screen than to the patient.
(** This just occurred to me – I bet the reason why pharmaceutical reps were so popular was that they brought a sense of esteem and reconnection with one’s identity back to the doc. And along with that, an opportunity for good dialog. I had many great chats with my reps about the state of healthcare, the stresses of being a physician …. A few were like therapists, with the added perk – bearing lunch!)
And yet, as you so plainly remind, the nearly universal reason why we each went into medical school in the first place – to use our minds and skills to help people and relieve suffering, to do good in the world and leave it a better place – has not changed. That idealism still lives. And people continue to suffer awful trauma and acquire complex and life-threatening illnesses, and sometimes die in our helpless presence.
And in this ever more pseudo-connected but terribly lonely society of ours, our patients come to us, they honor us as their minister of mind and body, and seek real connection, genuine compassion. But we are pulled away, that connection increasingly made impossible – shorter visits, “reimbursements;” the EMR, emergencies, bureaucratic tasks (one of which ironically is attending to ‘patient satisfaction surveys’ ! ….). And with the loss of that defining doctor-patient relationship, we lose our sense of purpose, of meaning, our very identity.
But even more tragically, while that existential crisis permeates more malignantly, while that which sustains our very identity as physicians crumbles, each of us is also feeling terrible isolation and emptiness and aloneness, aware of the lack of a coherent community, with few if any real and genuinely compassionate supports to turn to.
Your thrusting this crisis into our awareness, in all of its tenderness and rawness, has been so needed. It’s truly heartening to have hope that our profession might, just might, be able to re-humanize itself, to restore heart and soul to its being. I believe your suggestions are right on target and ought to be a focus not only for each of us individually, but also of a dedicated task force at every healthcare institution and training program.
And in response to your call to action, I promise that I will strive to bring that dialog that you’ve so bravely begun front and center in all the spheres of my professional life.
With deepest admiration and heartfelt appreciation.
Ok Kernan ~ Now you’re making me cry. Good tears. Cleansing. Our profession needs a collective grief ritual and a spiritual cleansing. I plan to visit each and every medical school in the US over the next few years and help revamp our medical education system. We must start by not inflicting this pain on the next generation of healers while those of us already wounded help one another heal. There is no greater call for the healer than to heal each other. What good are we to our patients if we can not help one another?
Wise words from readers as well as from Pamela. At age 81, long retired from child and family psychiatry, I now am a patient of several doctors. Takes getting used to! As an effort to help health professionals under stress, I wrote Intravenous Hope, Stat! We Need to Help Stressed or Suicidal Doctors, Nurses, Psychologists, Therapists And Their Relatives. The website above has some information about the book.
Don’t keep your problems to yourselves, whatever your role!
Bill Taylor
Thank you for this profound article. Though I did not know that the Suicidal rate was so high, we too lost the youngest member of our medical class, A. CARR, for whom we as a class have given a Scholarship named for him, but that is not enough. He was21 years of age, the youngest member of the class, sensitive, honest and as you have said “would have made an excellent Clinician. I have often thought “Was there not just one person that he could have called?” “Is there not one ray of hope, one line of trust that he could have had with any of us to prevent this?” You have analyzed the reasons well. Let us pray that there will be many persons who will listen, who will respond.
I’m a GP (family doctor) in the UK – it’s not just in the US that these problems are occurring. I’m currently off sick with anxiety/depression – this is my 3rd episode and I’m only 31. The first time started in medical school and I recall a particularly unpleasant ‘teaching session’ where I was ripped apart in front of a patient and my peers. My best friend stood next to me whispering ‘it’s ok, it’s ok’ in a bid to stop me breaking down then and there. We moved to the next patient for one of my peers to be cross-examined, when this patient looked at me and offered me a tissue because she could see the tears in my eyes.
The second crisis happened less than 2 years after medical school although I’m surprised I lasted that long. The gruelling on calls instilled such fear in me that I would get diarrhoea before each set of night shifts and at one point I actually considered making myself ill eg. breaking a leg, in a bid to get out of work. It was not helped that I felt responsible and blamed for the death of a patient and received no support.
Currently I just don’t think I continue with medicine – the job is wearing me down so much that I can’t seem to notice the positives anymore. It’s not helped that in the UK, GPs are currently being blamed for every problem in the NHS by politicians and the media; we’re told we’re lazy and overpaid and should do more for less money etc. Patients have become self-entitled and abusive/aggressive thinking that they know how to manage their illnesses better than us (we’re just here to hand over the prescriptions they demand).
I don’t know how things can improve to be honest.
Things will improve when we finally embrace the idea that health care is about promoting health and caring for one another. It is not about public humiliation, abuse, hazing, and media bashing doctors—the people who have devoted their lives to helping others.
This requires a cultural shift.
Human evolution requires these culture shifts at intervals. We once thought it was okay to own black people as slaves until we finally understood that they are HUMAN with feelings just like white people. We thought it was okay not to allow women to vote or own property until we realized en masse that women are HUMAN just like men.
Now comes the civil rights movement in medicine. Yes doctors are HUMAN too. We have feelings. We should not be abused. The sad part is that doctors are too often indoctrinated into a life of abuse by other doctors! We need to stop abusing each other if we are to evolve. Shine the light on the abusers. Stand up for your rights as a human being if you are being abused. If you are afraid to do this as an individual, then have a petition signed by all your colleagues or classmates. But DO something.
Here is a talk that I gave to medical students describing how to stand up against the abuse: https://www.idealmedicalcare.org/blog/how-to-graduate-medical-school-without-killing-yourself/
(the same can be applied to workplace abuse)
The call to action is for doctors to be REAL healers. You can not be a victim and a healer at the same time.
What use are you to your patients if you are a victim? You are perpetuating a cycle of abuse and teaching them that it is okay to live a life of silent desperation. They can see that we are not well. The solution to our sick health care system (in UK, US) is not more legislation, more bureaucracy, more media bashing, more patients on your schedule. The solution is for every doctor to look in the mirror and see the reality of their situation. And then repeat after me: “I will not be abused.”
Yes. Breaking out of this cycle of abuse is much like breaking out of an abusive marriage. Hard to believe there would be a prince charming for you when your husband is beating the crap out of you. But guess what? There is. You deserve to be the doctor you described in your personal statement when you entered medical school. Your patients are waiting for the real you. Look in the mirror. Claim your birthright. Be the doctor you had always imagined.
And if anyone needs help, check out this physician retreat link on website.
Or please call me. Seriously. 541-345-2437
Thank you Pamela…
I want to help. What can I do to start? I’m in my child psychiatry fellowship now.
How about a meeting of like minds to brainstorm?
-SP
Please share with residency directors and medical school faculty. Share this lecture widely. Also do the “all the above” in the penultimate slide. Get in touch with me if you want to do more. I have a plan. 🙂
Dear Pamela,
Thank you for an excellent perspective! You’ve so clearly articulated our pain from Vincent’s death. We sincerely believe that your advocacy will continue to promote medical suicide awareness and eventually save physicians’ lives. Please let us know what we can do to help.
Edna
Thank you for your courage to share Vincent’s life with the world. He is healing more people than you can ever imagine now.
What could the rest of us, non-medical folks (aka “patients”) do to support you in these efforts, to help you accomplish your stated goals? Your article is extremely enlightening, doing much to explain why I get the responses from docs I have had in the past. If docs had the time, and emotional support they need, and we’re professionally encouraged and supported to process their emotions, to learn to be better listeners/communicators with a more highly educated emotional intelligence, we would all have better doctors. Effective healing requires love and compassion, but docs need permission and the means to make this possible. I would very much relish the opportunity to support your efforts. You not only identify the too long overlooked problem, but you actually have a game plan! Now you need grass-roots support of patients. Tell us how we can help our docs, and your cause, please!
MOST important thing you can do is to keep talking about physician suicide (to friends, family, write an op-ed in your local paper), let your docs know that you know that they may be suffering and that you care. Just random acts of kindness go a really LONG way.
My articles on doc suicide are all archived on my website here: https://www.idealmedicalcare.org/category/physician-suicide-2/
And finally, please forward this Physician Suicide 101 to everyone you know. Especially doctors & nurses. Free audiobook under “books” tab on nav bar.
After doing all that if you still want more to do, contact me by e-mail off my website: https://www.idealmedicalcare.org
I truly enjoyed your perspective. I began medical school as a survivor of 4 tours of conflict in as an enlisted man in VietNam, so I knew what suffering, pain, and devastation people inflict upon each other.
It shocked me that a classmate took his own life. It was more shocking that the local PD at first tried to blame another classmate, his roommate, for homicide, and the Dean kept him out of classes for a few days. It took the war veterans in school to turn the dean!!
But despite the grueling demands: I find that nothing you talk about insofar as the time demands of training is any reason for a trainee to have that weakness of personality.
The interpersonal dynamics of ‘bullying’ that takes place, ever since ‘the team’ became more important than the legacy of the mentor, is the troubling factor, to me. I was strong willed enough to ‘tell-off’ any senior doc who pulled that on me, and still am: what will they do ? shoot me? Happened already! The demands on our time remains throughout our lives; but how we pace it it up to us! A great teacher and mentor wants their students to emulate them, to stand on their shoulders, and to improve upon what they have imparted.
When fatigue sets in, mature adults walk out, with apologies. Immaturity includes not recognizing this in yourself. In my opinion, the children who get into medical school who do not have the maturity to deal with the total time commitment, need to break it off, just break it off, and do something else for a few years. Then return to their dream, re-energized. What is wrong with a leave of absence? It is far better than continuing to deal with the maelstrom of emotions under stress.
But, I agree, we cannot accept the bullying. The attitude of bullies in the field of medical education is what you have elocuted so well. We have done poorly at re-educating or eradicating them.
Thank you for taking on this subject. I’ll admit I have been so close to suicide so many times. I’m fortunate to have a partner who sees the warning signs and reaches out. Others suffer in silence. It amazes me how cruel the medical education system is toward physicians in training. The cruelty is perpetuated by the residents who undermine patient care by treating each other so badly. When you feel that nothing you do is good enough, you stop “doing” and that includes caring for patients.
I had the honor of working with medical students. Yes, it is an honor, laying the foundation for how future physicians care for their patients. I had the reputation for being a kind and patient teacher, always available for questions or concerns. I reinforced the notion that, as medical students, there is no such thing as a stupid question. It is truly amazing to see how productive people become when they have positive reinforcement, positive feedback and the sense that what they do, even as a medical student, makes a difference.
All too often, they become victims of the ridiculous competetive nature of residents or, worse, the scapegoats of residents who lack the integrity to own up to their mistakes. They get thrown under the bus while a fellow resident is driving that bus.
I aam no longer in residency. I was not offered a categorical position in the surgery residency program where I was a prelim. My evaluations were “very good”, my patient care was “exceptional”. Upon speaking with an attending, I was told that because I wasn’t “cut throat” it was believed that I didn’t really want to be a surgeon. It was what I was told next that absolutely stunned me. I was told that I was, quite simply, too nice to be a surgeon. I’m quite certain that complaint did NOT come from the patients I cared for.
There is a tendency to view patients as their disease or procedure and not as a person who is feeling scared, vulnerable and wants to know that the person caring for them is invested in their wellbeing. The tragedy comes from viewing patients as “something” rather than “someone”. Those of us who see patients as human beings are ridiculed, reprimanded and, in some cases, told to get out of the medical field.
How did this profession, designed to assist others, get so far off track? When did it become ok to treat patients and each other with such disrespect and a general lack of empathy?
What do we do when the disillusionment strips us of the desire to practice medicine?
Some of us have overwhelming debt from medical school with no way to repay and no visible prospects to practice in a career field where you can be ostracized and left with what amounts to a worthless degree. The entire medical education system needs an overhaul. There needs to be a guarantee of graduate medical education upon graduation from medical school. Increase the number of residency programs to meet the number of medical school graduates. This “survivor” mentality of competition does nothing to train great doctors. It floods the system with narcissistic, self serving physicians who care more about themselves than the patients that turn to them in their time of greatest need.
There must also be a change in graduate medical education itself. The tradition of humiliating residents and medical students must stop. I do believe that with a leveling of the playing field, eliminating cut throat competition for residency positions, we would see a change in the stucture and function of the medical profession. We would see a return to patient focused care. Isn’t that why we all chose this career in the first place?
Thank you so much for calling attention to this crucial issue in medical school training. During my medical school/residency training I have been writing a blog “A journey through medical school & residency” in an effort to give my family and friends an insight into the grueling nature of the training process. Although no one in my school committed suicide, many became depressed and this pattern continues even now in my residency. I am in my last year of residency training and just this past week we had a discussion with all the residents in the program, one attending, and 2 psychologists, about the stress and trauma associated with our training. We are trying to come up with a better system of support for the resident, and not wait for a resident to ask for help. I myself am still carrying the grief associated with multiple bad patient outcomes (including one where my senior resident told me I killed our patient, and another where my attending told me to not apologize or talk to a family about a bad outcome). I like the idea of the Balint group and I’m going to suggest this as a model for our program. Thanks again for all your hard work Dr Wible!
Dr. Wible- I am so happy to have just found this. I am a physician who nearly died due to a suicide attempt during my second year of residency. I have desperately been wanting to help in outreach in the area of physician suicide. After several years not working as a physician, I started again 18 months ago. This is just my very short story. Please let me know if there is anything I can do to help. I, too, know of mental illness issues ending the lives of medical students I was acquainted with. Thank you so much for helping in this area. As you know, your work is terribly needed.
Thank you so much for having the courage to write this article. Our profession is unforgiving and inhumane. This includes not just PHPs, but other regulatory bodies such as the NRMP who have zero regard for physicians as individuals. We need to start treating each other the way we are expected to treat our patients– with respect, compassion and consideration. I can’t count the number of colleagues in med school and residency who had to take a leave of absence or drop out altogether– and the level of judgment from peers and superiors alike.
I remember in residency, an extracurricular group meeting led by a social worker who kicked off the meeting with an “emotional check-in.” Everyone in the room was stunned into silence because our feelings, thoughts, reactions are never EVER taken into account. We are so conditioned to focus on others that we forget how to care for ourselves.
We need to change the culture.
I find this true for nurses as well. I struggled with nursing school as I was a middle aged newly divorced mother going back to school to make a difference. The year after school was probably the worst in almost my life. I was fired from two jobs, and have worked at about 5 others within that first year. Nurses will eat their own and they were mean and spiteful. Of course, this is a general statement, there were some good nurses, but mostly they would make you feel stupid, not help, and even lie about you. If I were told how hard the first year would have been, I not sure I would have done it. As a group we are understaffed being expected to do more work with less resources. Nurses job hop a lot because they are burned out. Now I am finally doing a job I have ways wanted to do. But I am on salary, therefore the long hours, up to 14 hours in a day, is not compensated. I work on average, 55-60 hours a week. I take call one day a week and every 5th weekend. I had always wanted to do hospice, now with the schedule and limited resources the government provides, I am very disheartened. I will be in debt for the rest of myice to a profession that I don’t even know if I will be ae to work in within 5 years.
Dr. Wible, this is so profound and struck a nerve with me. I was dismissed from my medical school in the beginning of my fourth year because I had a medical condition that didn’t help the school’s ‘technical standards.’ I suffered abuse my entire third year from residents and attendings telling me that I wasn’t fit to be in medicine, that if I knew what was good for me I would just drop out. My school told me that being sick was akin to being unprofessional, and that I should give up my dreams of wanting to become a physician. They pulled me into their administrative office several times to harass me, and eventually told me that I was dismissed. I couldn’t think, I couldn’t breathe. If I hadn’t called my parents immediately and spoken to them, I don’t know what I would have done because only the worst was running through my head at that time. Medical schools NEED to be more attuned to their students’ needs and psyches before treating them like slaves or robots with no regard for human emotion.
Now patients can start to understand why they might be treated in a less-than-humane way. Look at how medicine treats its own. Deplorable. I am so sorry you had to be subjected to this. Who knew that choosing a helping profession could lead to a lifetime of abuse? I am happy to help you if you still feel called to be a healer—or even if you just need personal healing from your trauma.
This point about patients is so critical. I feel I have a unique point of view as an ex-pharma rep in psychiatry, friends with many residents and attendings, as well as married to an MD.
Many people feel dismissed and mistreated by psychiatrists, in particular, and are under the impression that the physicians themselves have no problems and never take the drugs that they RX. I know that is not the case, though I was not aware of these shocking statistics.
If this was known, I strongly believe the doctor-patient relationship could be much better, less *challenging*, and possibly supportive in both directions. I appreciated the earlier comment from the physician who valued his time talking to a rep.
There is a paucity of research and information about how to safely wean off of antidepressants, in particular, with many people experiencing horrendous physical and neurological effects for months and years later. There are now researchers using the data from online patient groups to study this and I can’t help but wonder if some physicians may be pushed over the edge by these withdrawal reactions on top of all that they are going through. Just a thought.
I realize this is an old thread, but I wanted to leave a comment.
It’s so uplifting to see this discussion. I think institutions are beginning to change. After leaving residency I decided I would practice medicine the way that feels natural to me. At times I feel as though I’m being watched and critiqued (no one has ever said anything to me but I think it’s the training in residency that still lingers, the need to see as many patients as possible; to be robotic and to the point rather than getting to know the patient). I still remain true to myself and my upbringing including the importance of prevention and I spend time with my patients to get to know them. This is what has kept me happy. My first day of my clinical rotations in medical school I felt depressed briefly but I quickly picked myself up. I felt sad after seeing a 5-month fetus after an elective abortion; I was responsible for bringing the tiny little boy to the pathology lab. It’s these moments that some of us are not able to shake. I will now do my best to keep my eyes and ears open for my fellow colleagues who are in distress. Thank you!
Thank you. I am a night shift ICU nurse. I see untold suffering so often that I forget that the new interns and residents are just cycling through the ICU. You have given me an opportunity to help them, I can help stop the bullying when I see fellows and attendings belittling residents and interns.
Thank you so much Julia! Theses young docs may have invisible emotional wounds far worse than the ICU patients’ physical wounds. Sometimes all they need is a nurse to give them a hug and a little container of apple juice. Interns may be starved for positive emotional contact and suffering from hypoglycemia. I was working with a blood sugar of 24 in school if you can believe that. It’s the simple gestures that can save lives.
I have been an RN for 38 years. You are the FIRST physician I have ever encountered who knew what Maslows Hierarchy of Need is. We learn it in Nursing, but no one ever seems to get that it applies to all of our lives all the time.
I love this presentation and you are right about Medical and Nursing schools driving us to depression. My disenchantment and burn out stopped when I quit depersonalizing my patients and started making what I did personal and relevant to them and me.
Excellent move Kate. I felt better when I started practicing professional CLOSENESS. Yes, I do laugh and cry with my patients. Yes, I hug and kiss my patients. Be human. It’s still legal. http://www.huffingtonpost.com/pamela-wible-md/why-i-kiss-my-patients_b_5399281.html
This was tough to read. I actually tried to put together a clinic like yours, but this June I was fed up and had no support, and I am fairly sure there’s no way I can work in western medicine. I hadn’t had a paycheck in 3 years and still had to justify my low fees (which felt like my worth). I have struggled with all of the above besides thankfully substance abuse since I was 8 or so, and yes, med school and residency nearly broke me, but they didn’t. Despite hazing in the NICU, despite my mother passing and not telling my attendings (so my poor performance was belittled and harshly corrected- made me a much better doctor in the end though), etc etc… At this point I’ve tried everything I can think of, but am at the end of the rope in many ways and thinking all I can really handle is working at a coffee shop or something. Maybe. Maybe moving somewhere where I already know people instead of being so alone where I was before. But I miss helping people and I was a good doctor. And had a great combination of skills I’ve never seen anywhere else. Not that it mattered much then. Is there anything out there for someone who refuses to market herself (again) and wishes to spend an hour with each patient and only work part time? Because I couldn’t figure it out on my own, and it can’t really face starting completely over completely alone. Thanks for any direction you can think of.
Andrea you MUST come to my next retreat and teleseminar. Starts in February. No excuses. I can give you a scholarship if you need. This is a total lifesaver. YES! You can practice medicine the way you feel called to practice. YES! You an make a living practicing medicine the right way. I would be honored to show you how to create your ideal medical clinic.
Thank you, it looks lovely, I’m sure it’s great for people wanting to start again. Also, I have a course (in Ashland, funny enough) I must attend in May already. I am just not going to be able to start my own clinic again, I’d need to find some other way to practice if at all. I really do appreciate the thought!
I lead these workshops twice yearly. Teleseminar & retreats are for anyone wanting to heal from the trauma of our training. Not all attendees open ideal clinics. I have premedical students, hospital-based radiologists, and others who attend. Maybe fall 2015 will work better. Regardless, keep in touch! xoxox Pamela
Please remember that it is not your fault that you did not succeed in practice, it is currently a “bubble” of consolidation.
I too have a solo practice and went through not taking a paycheck for 3 years, but was fortunate to have been known in my area over the last 25 years, and that there is a “niche” where some solo FPs like me can make it work.
A salaried job, at least for a while, may be all you can do, Urgicare-like.
Don’t give up, but pay the bills….
I am sorry you had to close up.
Dr Matlev in Western PA
Madhu spoke like an Isha meditator!
Perfect- absolutely true
Unfortunately, we are suffering from this as well in the veterinary profession. I am sure many of the underlying causes are the same. The rigors of veterinary school mirror that of medical school to some degree (although we typically begin practice after only 4-6 years after starting veterinary school in contrast to most medical students).
Suicide has become rampant in our profession in the past 10-15 years and is becoming more alarming every day. Thank you for shedding light on this as it may pave the way for doctors/veterinarians struggling with depression/anxiety to seek help earlier and prevent more suicides.
Yes. Some simple interventions in both veterinary and human medicine would be lifesaving. Happy to help vet schools humanize their educational system.
Wow… what a thoughtful article from a very compassionate lady… I salute you Pamela. I wish we could apply these principles to all areas of life…. in business, with our families, doctors to patients, and patients to doctors. Unfortunately just recently I’ve observed that the medical profession is often so stressed that they don’t have the time to really listen to their patients… and of course there are also those doctors who go the extra mile, but then maybe don’t have the support that they need.
Compassion and caring is what makes life worthwhile. I have a couple of friends here in the UK who have had their late teen children commit suicide. I think all suicides are tragic, but the second one I heard about was so tragic… the 17 year old girl knew she was having problems and went to her GP only 2 weeks before she hung herself. The GP with very little training relied on a “tick box” checklist to assess this girls state of mind… even though the girl said she was only there because she was feeling a little better than she normally felt. Her parents and family were devastated, and I have no idea how the GP felt but I doubt it was good. The parents and family have started a charitable foundation to raise money to fund training & to campaign for nurses with mental health awareness and knowledge in all GP practices in the UK.
What can we do in society and in our communities to create a world an environment to which people want to belong, rather than one they wish to leave.
Thanks again Pamela for all that you are doing. 🙂
“What can we do in society and in our communities to create a world an environment to which people want to belong, rather than one they wish to leave.”
1) Honor people for their soul’s purpose—their reason for being born. Stop homogenizing everyone to fit some industrialized mold of high productivity life.
2) Be compassionate and loving.
3) Rinse.
4) Repeat.
also this can apply to lawyers and emergency help professionals And military and a few more, I am certain politicians…….:) Thx for getting this out. It needs to be faced and dealt with…:)
I wish I had known you when I lived in Eugene! The October issue of Mindful Magazine has a couple of articles about doctor burnout, suicide, and prescription drug abuse. The author includes this staggering statistic: “Death by suicide in male physicians is 70% higher than among men in other professions, and up to 400% higher among female physicians than women in other professions.”
Thank you for your passion and commitment to this important issue!
The current Physician Health Programs represent a culture of psychopathy. If you look at corporate psychopathy this was the perfect storm.
We need to start recognizing this – many of those who are in leadership positions have histories of egregious crimes but reinvented themselves as “addiction Medicine” doctors. Many have a history of manipulative.behaviors. They present a menace to the profession.
I knew Greg in high school and college and looked up to him because I also went to medical school a few years behind him. One thing this article doesn’t mention is his brilliance. Greg was by far the smartest person I have ever met. His presence was electric and inspiring. This is the view of pretty much everyone who met him. I can only imagine how his spirit would have guided even the most terminal cancer patients through their illness.
There is clearly something wrong with a system that doesn’t nurture revolutionary minds.
Yes. I agree 100%. I have had many long talks and e-mails with Greg’s mom. His brilliance was not only noted by family members, but by everyone who was lucky enough to cross paths with this man. RIP Greg. On his 32nd birthday this Thursday (11/13/14) this blog will be reposted as the only highlighted story of the day on KevinMD and will be showcased on MedScape. Happy birthday sweet soul. We miss you.
I did mention: “All brilliant, sensitive people who felt alone in a highly competitive and inhumane environment.”
Wonderful article, Dr. Wible. Sorry if I sounded critical. What I was trying to say is that its almost impossible to describe Greg’s particular kind of intelligence and the world is worse off without him and his brain.
I know Richard. The loss of his brilliance is immense. And his compassion was in the same category as his brilliance.
Glad you are doing this. Much needed. But not just with doctors. And it is good you are focusing on what can help. But as you and some of the comments suggest the underlying causes and effects are many.
It is late and will return when I can write a more coherent comment, but since my health is precarious, I want to post several ideas for now while I can.
From childhood in the segregated South, I have been appalled at how difficult it is for people to prevent rather than react to difficulties. As an activist and psychotherapist I learned a bit about this difficulty, and now years later than I should have, I think I see one of the more neglected causes of our human disability when faced with traumas.
I now think there is an evolutionary design flaw if I can use that phrase, where as small dependent children we have an instinctual need for approval, which prior to about 7 years old, drives us to feel desperately responsible for traumas and since most are beyond our capability to solve, we are ultimately dependent on those who care for us for any resolution. So we seek relief and when we get it, we call this experience being loved. Now here is the flaw, what happens when the young child feeling responsibility (we call this shame and or guilt) is denied relief? For now, let me just say, the child does the only thing they can do with the painful shame they feel, they bury it.
We know how complaining children are often told to be quiet, and ignored. I call what happens not only toxic shame, which is a condition that all therapists have seen, but also a term not yet in the DSMV, “Childhood Post Traumatic Shame” or CPTS.
My theory is that this condition undiagnosed and virtually unknown and rarely treated therefore, affects millions of children, and through their diminished capacity to love or function well, it affects their families and communities.
One last observation, I think those who suicide and suffer from PTSD are more likely to have had this condition (CPTS) untreated and unrecognized in their childhood.
Pamela, thank you for outing a horrible situation. I have worked over 25 years in a university with a large academic medical and got to watch initially as I saw young human beings entering their 3rd year of med school (after all, they are totally sequestered year one and two, only to emerge into patient care settings after much of their humanity has been trained out of them) have to learn the hard way (using by being publically shamed in some forum) that emotions are not acceptible, only logic and “you can’t be wrong”. We know human being fail, so the basic premise of physician training makes them non-human.
Most of the last two decades, I have had the honor of of directing the Employee Assistance Program for the university. We attend new resident orientation each year and try to press home the message that we are there 24/7, we are confidential so their peers and attendings need not know and we are free of charge. We do get some takers and see all the symptoms you describe over and over. But we also don’t see everyone who needs us and those have ended their careers in ways similar to the doctors you describe in this post.
We also have experienced physicians referred formally to us, sometimes because they are the attackers, sometimes because they were victims of attack and responded without following the unwritten rule of not going public. We need to unwrite this rule. We need to make anyone going into a medical career (doctor, nurse, pharmacist, even technical and support positions) know that there is a risk, but also that to address this risk there is SUPPORT! But before we can do that, we need to build the support into the system and it is clearly not there right now.
Thanks for pointing it out. Knowing is the first step towards actual change.
Before we can solve a problem, we need public awareness.
Hi Dr. Wible,
I often wonder how many of these persons realized that medicine was not what they had expected or hoped it would be. Also, I wonder how many went into medicine for the wrong reasons. I know I did.
I never liked medicine. I still don’t like it. Perhaps, I even hate it. I had only entered medical school because my family expected it of me, as I had been groomed to do so from a very young age. I have met others along the way, too, who had similar upbringings. I knew, by my 2nd year of medical school (actually by sophomore year of college, but only came to the full realization here), that I would never find self-fulfillment in medicine. I wanted to drop out, but had no potential means of repaying my loans and, immaturely, couldn’t withstand the pressure from family. Some of my close friends had told me the same thinking. I began to feel trapped, hopeless. I often thought about killing myself, mainly by hanging for some reason.
One day, it all came to a head at school, and, long story short, I had a complete meltdown in the administrative office. They stuck me in the corner and watched me until the dean came to meet with me. He treated me with such kindness and genuine concern. They suggested I take a year leave-of-absence, but I feared how it would appear on my CV and affect my placement into residency. Instead, I continued to attend school and started seeing a psychiatrist and psychologist, which did help my state of mind.
I had another “relapse” during internship. My training program did not foster a nurturing environment. If you violated duty hours, you were blamed for being incompetent and inefficient, and other such foolishness abounded. I feared that the rest of my life would be like this and considered ending it at times because I didn’t feel like living that way indefinitely. Again, I had a meltdown in front of a superior. Fortunately, it was the right one, as they took me into a private setting and spoke at length with me, setting me up with the wellness center.
Since then, I have not really had such severe episodes. I still don’t enjoy what I do or find fulfillment in it. I am only 30 years old and just feel like I am running out the clock until I die by whatever means the universe has in store for me.
I don’t know if my story helps at all, but I feel there are more people like myself in the field than truly recognized, and I wonder if there are others who felt they were just finally doing things on their own terms.
Wow. In the 1930s, my dad and his brother were sent out to the front porch while their parents had a meeting inside the house. When they brought the boys back in, my dad was told he would be the doctor and his brother would be the lawyer. Jewish family in Philadelphia. Probably not the only family that assigned their kids’ professions. Happens in more subtly too. Not a good way to launch a career in medicine.
On another note, love to have you at the next retreat. If I can’t help you find a way to enjoy medicine, we’ll figure out an enjoyable exit strategy (not suicide). Let me know. Please do not live a life of silent desperation.
I interviewed both my parents about WHY they really chose medicine as a career. BOTH went into medicine for parental approval and love. Probably a more common reason that any of us want to publicly acknowledge.
I have been a residency program director for over 25 years. And I always prided myself on having been very close to the residents and indeed, they brought me their personal as well as professional concerns. Usually, it was enough for me to listen. One of my great rewards has been continued contact with “my” residents for the rest of their lives. I am regularly thrilled when they send me photos of their growing family. Word of my mentoring also reached the medical students and so, unofficially, I usually had several students each year whom I regularly meet with. One such student was obviously brilliant, hard working and dedicated. But somehow, he kept failing his tests. I pressed him a little to understand what was happening, and finally he confessed that he hated medicine and didn’t want to become a doctor. So why not drop out, I asked. Because his parents were dead set on having a son who was a doctor. He added that I didn’t understand his culture (first generation Chinese) and how, to use his words, “impossible” it was to discuss with them what he wanted in life. Eventually, I met with them. They were a lovely couple and, with their son’s permission, I spoke of his dreams and fears. They surprised him with their understanding and eventually (months later) gave their blessing to his leaving medical school to embark in another career. It was a happy ending that might have instead ended in tragedy. Sometimes, children of loving and dedicated parents are wrapped up in their image of success. They so fear letting their parents down, that they become trapped and unable to express themselves with vulnerability. As this young man repeatedly told me: “The pressure was unbearable.”
very poignant and resonating lecture. I am a medical oncologist and recently I met with a patient with newly diagnosed metastatic lung cancer and he was saying that his neighbor who is a physician had been helping him through all of his tests, scans etc. but that his neighbor commited suicide 3 days ago. The patient said isn’t that shocking a doctor commiting suicide. I told him no it’s not it happens all the time. He teared up and said I guess if I had to deal with cases like mine day in and day out I might be suicidal too. It was just such a hard comment for me to process but true on some levels too. I hope I can sustain my career and my sanity it seems like such a hard task.
So very sad to lose another doctor. We can heal as a profession. We each can reach out to one another.
No need to be isolated in the suffering. We can build support systems into our workplaces and medical
training programs. Some of out suffering is self-inflicted. I’m writing a book now on solutions.
You are welcome at my retreats if you ever need a dose of love and inspiration. See video:
https://www.youtube.com/watch?v=_tPFSgaL5ZM
Love to meet you one day . . . soon!
Dear Dr. Wible,
I thank you very much for your excellent article (Physician Suicide 101: Secrets, Lies & Solutions). There is something which you have previously published on KevinMD – I liked it, too; and I believe that I responded to it. Thank you again. A brief bit of self reference: I am a semi-retired Licensed Clinical Psychologist, who lives in Illinois.
However, what I feel a need to say here is that I am sending a copy of your entire article to each of our three adult children. I will also attach a small summary of some of your concluding observations and recomendations. Each of our ‘kids’ is an adult now. Each of them have selected health care professions for themselves. The oldest (and fiancee) began practice as anesthesiologists this past summer. The second oldest is in her third year of medical school. Our youngest Our youngest completed a 3 year Masters program in school counseling – it is a field which most states have all but eliminated from their requirements for all but high schools. Alas!
Reading your text brought tears to my eyes. Not only did I meet the persons and families which of whom you wrote; but I also revisited a psychological autopsy of a friend, David, who committed suicide while we were in graduate school together.
There were many places in your manuscript which caused me to wish that I could respond to it (in greater detail than I am doing here). That tells me that you are both a very good writer, and that you possess the ability to write soas to convey dialogue in your material. That is not so common a trait in writers as many imagine. I intend to share your materials with a friend who has written a fine book about this latter subject.
Thank you again. And know that I am passing along what your experienced and wrote about, not just to ‘protect’ our much loved adult children, but also to remind them to also be alert to this risk to their friends and colleagues. I have had both PCP’s and varied specialists as clients during my career. As I see it, you have illuminated exactly the perils of their professional and personal lives exceptionally well.
Keep up the good work. I hope that it will help save some worthy lives.
Dick Stanton
Thank you Dick ~ I am writing a manual now that can be used by health care providers and the public to save medical students and physicians from suicide. Also, once we have healthy health care workers we will be in a better position to actually help our own patients with mental health issues. A win-win for all.
I had the privilege of viewing Dr. Wible’s “TED” talk. I was very impressed. Even though I have never contemplated suicide, I have been very disappointed and frustrated with my choice to pursue medicine as a career. So much so, that I decided to pursue a “Preventive Medicine” residency. I chose to study “Sports and Exercise Preventive Medicine”. This program was offered at only one place in the US. The prestigious “University of California, San Diego”, and “San Diego State University” offered this program. After completing this two-year residency upon completion of an “Internal Medicine” internship at the National Naval Medicine Center in Bethesda, Maryland, I felt that my training was superb and truly resonated with my beliefs. However, given the uniqueness of my training, the Navy was never able to properly utilize my skill-sets, so I basically languished as the “bastard-child” in a primary-care delivery system dominated by Family Practitioner’s, which I was not. Also, I was ostracized by the Preventive Medicine community because I was not trained to perform the usual duties of a Prev-Med Officer in the military. Anyhow, my point is that my last twelve years in the Navy, I was mis-utilized! This predicament, and my disdain for “downstream bio reductionist” medicine motivated me to pursue “Naturopathic Medicine” and “Functional Medicine” studies and board-certification. I am much, much more happy now with this “change-of-course”.
This is a well written article. The issue of physican suicide need to be addressed. Mental illness and substance abuse are issues which truly need to be addressed because these are underlying issues. I only wish I had known all of this in 1997 when I first started medical school.
This is actually personal for me. I am 38 years old. I was diagnosed with depression almost two years ago after I swallowed a bottle of extra strength Tylenol after having an altercation with my spouse. I survived because my family intervened and called 911. I realized that my symptoms probably started in medical school. I started med school in 1997 and finished in 2001. I started to feel sad and become more withdrawn. I did my surgical residency which was no walk in the park either. My first marriage ended and I got a divorce. I remarried while in residency I struggled for the first few years but managed to finish and even matched into a fellowship. I finished and went into practice which was a struggle as well. I separated from my second wife after our altercation. She took off with my daughter. I take responsibility for all of my actions.
I feel that if I was not afraid of the stigma I would have taken my symptoms more seriously and obtained help. Instead I attributed all of my symptoms to feeling sad. I am glad that you are doing this. Because of my experience I am in the process of writing an autobiography of my experience in order to shed light on this experience.
Despite all that I have said, there continues to be stigmatization. From my own experience I have had an overwhelming amount of support but I have had to with the repercussions of having a diagnosis of depression. I also feel that medical school and residency can be brutal and rob humanity from the best of us. I thank you for writing this piece.
Not only is suicide a problem among Doctors, but the general population is committing suicide every 15 minutes. (CDC 2011 figures) . Some numbers on veterans are higher that that.
Are you aware of the Limoge’ wave Transcutaneous Cranial Electrical Stimulation (TCES)? It a wave that you do not feel that produces electro anesthesia . It controls Pain, Stress, Anxiety, and Addiction without drugs or side effects.
Its was used during the Vietnam War to refresh the chopper pilots that picked up the wounded. We pulled out of Vietnam and Dr Limoge’ went back to France and with the two other doctors that help him develop the technology use it to control chronic pain. We have a study (Not to FDA Standards) done in France in ’95 on a number of heroin Addicts that had an 80%+ cure rate.
You have my email address. If you want more information let me know. JBJ
Wow James. That’s great. Feel free to post links to studies here for all to view.
Dear Pamela
I’m so impressed about your article.
I’m a pediatric trainee in Australia, I’m struggling with exams.
I have a beautiful family that keeps me alive.
I don’t know what my luck would be if I were alone.
I did cry a lot reading your page, I’m still crying.
Thanks for thinking of us even if we are far.
I know I will be fine but I’m still crying
Thank you for speaking bravely about physician mental health. I would like to share your comments with my colleagues in the form of a grand rounds. Is there a video recording of the lecture you gave and do you mind it being shared?
There’s no video from AAFP, but there is one from Scranton TCMC where I also presented it that week to medical students. I am trying to get a copy. I do plan to present this in other venues as I am doing a big speaking tour over next 2 years to US medical schools. I would be happy to speak at your event as well.
I am 15 years retired and still reflect on how close I came in my first year of med school.At the start we had a physical exam and my BP was 180/112. After rechecks, an IVP etc no cause found so BP lowered with a Rauwolfia compound.My roommate and the doctor in student health saved me from the subsequent acute depression. I have since lost two college roommates to suicide. I started running to relieve stress and it has probably done more for me “down the road” than any medication or conversation.Being sensitive was a wonderful gift as a physician but I quit because of a malpractice case that dragged on for almost two sleepless years and was settled for a pittance. I would have preferred 6 weeks of jail time. We could have called it vacation time !
Keep up the good work. Hey, where are the male comments ?
Lots of male comments on Medscape: http://www.medscape.com/viewarticle/834434
Here’s one:
Dr. bruce haupt| Physician
Before you kill yourself, call me first. You may need to leave a message and I may need to get back to you.
My associate told me indirectly that he was going to kill himself but I told him that he’d get over it. He said I was wrong and when my secretary can screaming into my office completely out of control crying that Len had just shot himself in the head and that the trauma team at Suburban hospital in Bethesda gave him virtually no chances of survival.
That was in 1980 and I haven’t lost anyone since then.
202-253-7300.
I was asked to share my story.
I was a near loss a few times over for my “chosen” profession. I went to medical school at the prodding of my family. I hated it and had a bout of depression while in the “booking stage” of school that I weathered without treatment. Somehow, I kept passing my classes. I developed test anxiety along the way which only made it worse.
Once on the wards, I found I had some natural ability and hand skills. I set a goal to graduate because no one gets credit in life for part of med school. I dealt with chauvinism and teaching by intimidation/shaming that was how things were done at that time. Graduation felt like a sham–it did not mark pride so much as survival.
I had mild runs of depression on and off in residency, but was still functional and respected. To boot, I did it as a single parent of twins (med school marriage that didn’t make it).
In private practice and dealing with the long hours and family strains, I continued to suffer mild burnout in waves. I continued. A few lawsuits (dropped) further stressed my system. Another lawsuit for a patient I saved ended in a settlement with my attorney saying they should have had a parade for me instead. More chipping away.
I allowed myself to become a salaried physician, and then had all my ability to control my career taken away. I was thrown into hospital and call-group politics. I grew to hate my job more and more. I became anxious about complications and things that could happen on my watch, even though I had a good track record. Call nights became dreaded. I was crying in the call room wanting to go home.
Finally, I asked for leave, though asked for family reasons, not my mental health, for fear of losing my hospital privileges. While on leave, the chair threatened to shut down my practice and did nothing to cover my patients. I sunk into a suicidal place.
I went to Borders Book store to find the book Final Solution to know how many of what pills it would take to kill myself. They don’t teach you that in training. They didn’t have the book, so I stood with tears running down my cheeks in front of the Death and Dying section. A woman approached me and asked if I had lost anyone dear to me. Not being able to admit the truth to her, I said “yes”, and let her hold me while I cried on her shoulder. Only later did I see the irony that I had lost me. I did find the book at the public library, but never went beyond that.
I asked my chair if I could ease back into the schedule, maybe not do night call the first several weeks. I was told I would be fired if I was not back at full function. The anger over that somehow carried me over the next year as I worked on leaving my job.
I went into solo practice on a more limited level. Nearly went bankrupt the first 5 years while paying off the debt. Though I will never see a six figure income again, I can handle my work at my own pace and in my own way. As long as the government and insurance companies don’t spoil it.
Having a modicum of control makes a huge difference. Being told how to keep records, how to and what to prescribe for my patients, how to practice, what I should withhold from patients, what I should manage to teach my patients in limited time, what data I should collect for Medicare, billing and rebilling, more and more privacy rules, more and more regulations, re-boarding, CME, etc. is exhausting. Anyone going into medicine now is crazy.
Judy,
Similar story-15 years now as FP, first 12 as salaried MD, now in private practice 3 years. Single mom of 3 that unexpectedly became 6 after having to take custody of another family member’s children. All the reasons about data collection, insurance and Medicare regulations, etc have piled on so much more. I’ve lost hope it will ever get better or easier. I can’t do this another 15 yrs. I feel guilty because I will have an option to reduce my hours in about a year, but that is still so far away. No options in the meantime to stop this relentless onslaught. It’s just overwhelming.
Thanks for your fine work. It’s nice to see such a serious problem discussed openly. I attended Harvard Medical School, made what the books assured me was a reliable suicide attempt, woke up 36 hours laters. Blind luck. I was offered an antidepressant, time off doing research, and the choice to return or no. Nothing more. Studying was no big deal, that was like asking a fish to swim. Sleep deprivation was devastating, and I have come to see it as completely counterporduct as a educational strategy. It risks countless patients’ lives, and serves only as an advanced form of hazing, more thorough and relentless and of greater duration than any hazing I’ve found elsewhere. Other forms of bullying take on new toxicity when one is so weakened and vulnerable. So I got out. I’m a nurse and a teacher now. People ask me, often, “why” I’m not a doctor. Why? Because I stood up for myself, at long last. No more.
I see it among clergy too, being a survivor of PTSD (Gulf War), US Army Chaplain.
I used to be an avid hunter, but now don’t have a gun in the house! I know my limitations and weaknesses.
Isolation of helping professionals is dreadful. Particularly in rural areas where I’ve ministered for 28 years (I am an ordained Lutheran pastor) and a Licensed Clinical Professional Counselor in the state of Montana.
I am in the process of setting up a non-profit to provide counseling for rural clergy and their spouses it is with LegalZoom right now.
Your insights were very welcome as an Army Chaplain I dealt with the aftermath of suicide and tried my best to prevent it by being close to my enlisted men!
I’m not a doctor, but a patient. I had some medical problems recently and saw lots of specialists and took lots of tests. No one was able to fully explain or understand what the problem was, and I saw a lot of frustration on the part of practitioners in various medical fields. They wanted to help, but didn’t have an answer. At one point I told my primary that I wasn’t expecting her to be a miracle worker and that there were a lot of things that were simply not known to medical science. She seemed really grateful to hear that and said she wished more of her patients had that attitude.
I was really shocked to read your article and had no idea the physician suicide rate was so high. Is there something I, as a patient and compassionate human being, can do to help?
You can check my blog under the category “Health” for more information about what was going on and who I was seeing.
In any event, thank you for posting this. I will follow your posts for sure.
Best, BostonMargy
Things patients can do are simple. Just like what you did. Offer appreciation. Let your doctor be human. Say, “I’m not expecting you to be a miracle worker. There’s lots of things that are simply not known to medical science.” That is all wonderful.
Other ideas: Compassion and empathy work wonders. More than once, a doctor has disclosed that a kind gesture by a patient has made life worth living again. So give your doctor a card, a flower, a hug. The life you save may one day save you.
Thank you for tackling this important problem. Mental health among healthcare providers is often overlooked or, worse yet, ridiculed. Keep up the good work. David Holcombe
Physician suicide is one of the things that can help connect with patients more than anything. We are human, just like our patients. We have needs; we have every right to break out of an abusive system. So many people come to us and have this notion we are perfect – that can actually HARM the trust between people. If we are perfect, then it can be done; if it can be done, then how inferior must someone be that they can’t achieve it? By being more and more open about what we as doctors experience helps everyone understand we’re all just trying to make something new for ourselves.
I found Dr.Wible’s article interesting and unnerving. I am a recently retired internist/geriatrician. I retired after both physical medical issues and some mental/stress problems brought me unwelcome interest by phs. Your article is especially concerning as my 22 year old daughter is a first year DO student. I have long enjoyed medicine and all my patients. However,administrative/.corporate world was soul destructive. So,here I am. I have found that there is life after medical practice(I am 61)!
Hi I totally agree with you and I have had issues with the Board and some terrible BCBS insurance panels but I am hanging there as I am hoping some day doctors can make a change and I truly love my work and my wonderful patients.
How can we get together to make lasting changes? please contact me.
What an amazing story and no one outside of the medical industry really knows about it–at least not anything more than a car crash announced on TV. I run a blog with the title “cluelessdoctors” that is actually a criticism of the establishment, big pharma, recently the FDA, and also some doctors who really appear clueless but I never understood why. I now do.
I have a question: Why is there such pressure on doctors to finish this amazing amount of learning in such a short time? I find this interesting because one of the reasons I chose not to be an MD is precisely the pressures and the internship of ungodly hours. I did not think I could do it and I think I am right. I turned into a PhD instead and decided to leave that rat-race also for those who care to kill themselves for tenure or the Nobel Prize. I am not interested in either. I am trying to overturn the system that created these monsters and the drugs that kill us.
I can see from your stories that I am barking at the right tree but from a distorted angle. I took on the case of patients who get misdiagnosed left and right and killed by the wrong treatments–unfortunately my mother was one of them who got killed after I diagnosed her with serotonin syndrome (in a hospital where I was not a doctor or scientist) and the medical director of the hospital in care of my mother said “serotonin what?” and the psych said “she cannot have serotonin syndrome because it is so rare.” So as you see, as a professional quite cognizant with the field of medicine (I am in neuroscience researching the hormones of decision-making) I see what you see from a completely different angle.
I see that the good doctors left and the bad ones remained–and this is what I was told by many of the MDs I have asked. Is that really what is happening? I do not see that in your story but perhaps it is politically incorrect to discuss your colleagues like that in public but I need to know.
I would like to join you in your fight. I was a professor in lecture halls for hundreds so I can give public speeches with no effort. I really want to participate in your effort of getting things right. I am 61–like the writer above me most amazingly–and my life started after academia–the same way as Beth’s after her medical practice. I don’t think the similarity is a coincidence! If your time allows, please contact me so we can chat and discuss what I may be able to help you with and how I may join hands with you.
Hugs,
Angela
Hi,
I was aware of the issue but not the extent of it.
Honestly I do not go to Allopathic Doctors because the whole system is tragically flawed and this problem written about is merely the tip of the iceberg.
Allopathy has become a money making machine that seems to be spurned on higher up the food chain than the actual MDs.
I have relatives and a number of MD friends from various specialties, but I have no interest in what they know, because I know that it is just a puppy mill for the folks who make drugs. Sad but true.
I have one alternative training specialty and am working on another (for knowledge mainly as we are very healthy). I also have a number of medical devices that have been banned by the medical mafia and trashed over the web (in North America) by the shills employed by said companies. These devices all work as advertised and the brilliant PPL who designed them have been driven into poverty and disgrace by the medical mafia.
I feel for you PPL who were lured in by the promise of fame and fortune. I know this doesn’t help, but you PPL need to reform your profession badly.
Alan
Thanks Alan but we are not lured into this for “fame and fortune.” We went to medical school to help people. Plain and simple.
I hear you Pamela and truly feel for your plight.
I am a pro pilot (retired) and I know lots of PPL who became one because they heard about the glory days of Pan Am and once they got in and found out the pay, they left.
A sweet relative of mine and my Alternative (as they are now referred to, sadly) Doctor’s child are in school to become an MD. I think it is a dream to be a well paid, well respected person doing a lot of good reducing suffering, and maybe they will be OK. I do not believe they simply want a Benz, as they really are kind.
The reason why med school is so brutal as explained by a Dr of Internal Medicine friend is that there is a silent rule, that less Drs means higher pay. It’s a rule that is as old as unions, guilds, and so forth.
Back prior to 1910, before the Rockefeller’s financed/instigated Flexner Report was issued, going to med school was basically a one to two year affair. There was in excess of 150 schools in the US. Then it was winnowed down by the Rockefellas and their crooked friends to around I believe 19 schools that taught Allopathy and taught the Holy Grail of ‘surprise surprise’ drug usage and slice ‘n dice. Did it change the quality of care in the US??? Prove your answer scientifically, not with just an opinion. Stats are fun.
Now it’s a many year effort in which you pay for lots of knowledge that has nothing to do with medicine. Fun to know, but useless. It is simply a way to reduce the Doctor rollcall and make Drs scared of being booted out if they don’t push drugs.
My friend explained to me with sadness how very bright PPL he was in school with, got washed out after they got tested @ O-dark thirty (middle of the night after working straight for days) with an oral exam. Too bad so sad. This is nuts!
Pilots long ago stopped pulling 24 hour duty days. It’s illegal now. My friend and his wife (both specialists) told me they worked many days straight. I was/am horrified. There is no need for this. Lots of bright PPL are accepted in the schools.
This is pure and simple squeezing the Doctor supply tube to keep up salaries.
I doubt that you have anything to do with the root of this madness but you and your colleagues can and should at least tear down this nonsense.
I used to rail at one author, Nenah Sylver PhD who suggested that this was a male plan* created by males, but now I am softening and starting to see that she probably has a point… Because… all of the rascals at the top of this pyramid are indeed males with a smattering of females who have seen the gold.
*not really a plan, as in ‘someone sat down and created it’ but really a house of cards that just keeps getting taller.
I am not trashing Doctors BTW. I have too many friends and relatives who ply those waters and thank heavens they do, because even though I never go to their offices, one day I might get hit by a car.
I wish you luck in rescuing your calling.
Thanks Alan. Pray for us all. Our health depends on having real doctors in our time of need. The women in medicine are often a masculinized version of their former selves. I believe in a humane approach to health care and training. How can we effectively work in health care if we are dehumanized?
I have lost 2 physician colleagues from suicide and I am grief stricken that they committed suicide. I would like to speak with you in regard to a project I would like to put together for physician’s health.
Please contact me on the email above.
Thank you so much for your wonderful blog
Chantal
Thank you so much for the truths you speak for so many. Many times in my years of medicine I have said to trusted friends and to several therapists, “something happened to me in med school”. I was happy, secure, and mostly unafraid until the age of thirty. Until med school. I do not know what happened precisely, but I do recall in vivid detail that on the first (orientation) day of med school the MD who was our anatomy professor, and therefore largely controlled our lives for the next many months, stood before an auditorium filled with 125 eager, nervous, idealistic would-be healers and said these words:
“If you decide to commit suicide, do it right so you do not become just a burden to society”.
He then described in anatomical detail how to commit suicide. I could not possibly make this up. I have often wondered how many auditoriums full of new students heard those words from him.
I am sure someone stood in front of us and told us what a wonderful and rewarding profession we had chosen. I do not remember those words. But I do remember how to successfully commit suicide. With a gun.
One month later, on the eve of our first monthly round of six exams in one day, I had my first full-blown panic attack. I had no idea what was happening. I thought of course that I was losing my mind. I took a leave of absence and made up excuses. I returned, and completely untreated but with maladaptive compulsive behavior completed med school, survived the public “pimp sessions”, and all the rest. No one ever suggested that the process was brutal, or the responsibility frightening, and no one offered us help. I have maintained contact with only one colleague from med school, so I do not know how the others fared. Through the many years of training and through what would appear to the observer a successful career in a surgical subspecialty and now into retirement, I have carried the anxiety, and the depression, and the fear. Perhaps entirely unrelated to those first days in med school, but still something happened to me, and probably to many of us, that changed us forever. I still remember how to successfully commit suicide because someone who had power over me at a vulnerable time described the details. And we wonder why…
Thank you Pamela! This webpage is awesome btw. Very easy to navigate and learn from. Hugs and blessings.
Most of my friends are not physicians. When they ask me why most physicians are assholes and I am not, I describe to them my medical education. I compare it to army boot camp. They tear you down as a human being and build you up as a “doctor”. I just refused to lose my humanity. Unfortunately, many of us who do do end up damaged from the experience. Thanks for this insightful page. When I taught medical students and residents I refused to bully and belittle them. I think they learned much more that way.
I’m just a fellow human being that feels your pain. I’ve lived a hard life and try to keep my head above water by leaning on my faith. Just simple prayers for help through my days makes an amazing difference with my endurance. I think my forgiveness to others and myself helps me to understand the meaning of life. The people who have chosen to save the world and it’s inhabitants of every sort, tend to take the many disappointments the hardest and end up in a puddle. What you need to know is that you can make a difference in you own small way, but you need to recoup so you can keep on. I know that I’m counting on you. Thank you for the enlightenment. I guess we are all just human.
Hi Pamela – I think you should pitch an episode on this topic to Grey’s Anatomy. Maybe you could get a cameo as the retreat facilitator!
As a longtime Nurse, I have seen the bullying…you find it in every area of medicine and among all medical professions. For Nurses the saying is, “Nurses eat their young”. I never understood why the people who stand up to care for others treat each other with such brutality. I can’t tell you how many times I have stood up to a “medical bully”, in defense of myself or of a less seasoned colleague. I am not the most popular among the people I work with because, most know I will call them out on their bullshit. Some of the meanest people I have ever encountered hide under the cloak of being the ‘healer’.
As a Mom, reading this has left me completely heartbroken. I will not encourage my children to pursue a career in medicine and because of this article I will watch them like a hawk if they decide for themselves to go into medicine.
I am not surprised at the outcomes of medical practitioners. I was a nurse for years and went back to school to be a Physician Assistant. There is so much abuse handed out in training. At the time I was in school, we still had some 36 hr. shifts. It was difficult. At least at the University that I attended they had a buddy program. All of the first year students were given a third year student to help show us around and be a mentor. The problem was that before we even started our first classes, my mentor committed suicide. She was in her car on her way home still close to the hospital when she stopped at a red light then picked up a gun and shot herself in the head. The person behind her was a physician at the hospital. These things are not that unusual. It’s a sad state of affairs.
Dr. Wible, very interesting information, I agree that it’s time to break the silence. Thank you.
Thank you for an amazing insightful read, my daughter is struggling in 3 rd year of medicine and horizontal violence is alive and well
As an outsider I am not surprised at the high rate of suicide among doctors, particularly in training. They are all sleep deprived. This alone must increase the risk. Everything is more manageable for the well rested. Add all the stresses and it looks like an emotional time bomb.
Nurses and paramedics experience crushing career disappointment also. Lots of hidden substance abuse and depression. Medicine used to involve helping people. Now it is a business transaction.
Thanks to Krista for sharing this thought stirring article. I need to reach out to my friends in the medical field more… And, study more on applying these approaches to other areas…
HI Pamela!
Thanks for sharing this aritcle.
When my ex-husband was in medical school his lab partner and friend (good buddy and mentor type) drove out into a field one day and shot himself in the head. We found out about it on Halloween Eve….my husband started to laugh the strangest hiccuping sound I ever heard come out of his mouth. He never laughed any other way after that, he seldom ever laughed after that. He too struggled with depression and suicidality, as well as alcoholism and sexual addiction/multiple affairs. We were married 21 years and then he divorced me for someone 10 years younger. He is estranged from his daughters, weighs close to 400 lbs, and I seldom see him. When I do, I get an overwhelming feeling of sadness for the slow suicide that is his life, for the beautiful man who is missing in action forever. He was a musician, a poet, a gifted singer, writer and gardener….none of which he does anymore.
I hate medicine. It cost him his true life, it cost me and his daughters our family, it is the source of unending grief for me when I let it be….but I have worked hard to heal and have found ways to deal with my own mental health issues, ways to stay in recovery.
My daughters are adults now, and are doing well, although some aspects of life are still a struggle. We can communicate about feelings, dreams, hopes, fears….and they have a step-dad now who they love immensely, who loves them unconditionally….and he’s not a doctor.
I went on to earn a PH.D. in Human Studies and I research resiliency. I work in a mental health role. I write….
….and some days I still weep for the incredible losses the terrible Mistress of Medicine inflicts, and for the beautiful dream that disappeared.
Thank you for “listening”.
Best wishes to you in the very important work you are doing.
Annie
PS…you may share my story if you think it will help someone….
Now you have me in tears . . . again. The pain never really goes away. I will email you.
How sad. I have goosebumps all over my scalp from reading this. I’m so sorry for your loss. Thanks for sharing your story.
Thank you for writing and sharing this knowledge. I have worked with young and older physicians for 45 years and I am an RN. I recently had a family crisis re subject of suicidal ideation and am processing what to do and how to help my young loved one who was in college and taking stressful science classes.
As an alternative therapist (Alchemical Hypnotherapist and Trainer), I’ve been noticing how many of my clients were shamed, belittled, disbelieved, etc. by their previous therapists, and I coined a term I call “therapist abuse”. I’m so glad to hear you speaking about that subject.
And I’m thrilled to hear you mention body/mind/spirit integration as I see how the therapeutic medical world is forced to shy away from adding the concept of spirit (IF they are even emotionally intelligent enough to understand the body/mind connection. At least it is becoming more accepted and even taught in some schools.
Thank you so much for “coming out” and shedding light on this subject I had no idea about.
Therapist = The Rapist. Just another interesting play on words.
Please include other types of doctors. Veterinarians commit suicide at a rate unsurpassed by other medical professionals. Please help us, too. We share a lot of the same causes of depression, stress, and suicide.
Agree. Veterinarians, dentists also high risk.
I left practice. To heal myself
. Twenty five years later, I am whole again. Curious how I did it? My YouTube channel is liambsden ???? part of ending aging n death, Happy new year
Thank you Dr. Pamela for shedding a bright and focused light on the deliberating issue of suicide among aspiring medical doctors, doctors and nurses alike. It is deeply saddening to read the accounts of Vincent, Greg, Kaitlyn and yourself in this ordeal.
I am grateful for your cause and the awareness being raised on such a delicate, soulish condition. My thoughts and prayers for the family, friends and all sufferers — that healing, comfort and restoration come about through this, and other voices uniting to support and end physician suicide!
Many thanks for your sincere dedication — and heart! 🙂
Thank you Brendaline. Silence will not save us. We must speak the truth and here comes the documentary –> https://www.idealmedicalcare.org/blog/emmy-award-winning-filmmaker-takes-on-med-student-suicide-view-movie-trailer/
Hi Pamela, I’m a physician who graduated in 2010. We lost one from our med school class a few years ago but I’m unsure of the reasons. He graduated top of the class and was finishing up a very prestigious residency. I can’t assume to know the reason for him taking his life; if it was stress from being a doctor or something else. I can say that med school and residency were some of the most depressing times of my life. I truly felt like my med school didn’t care at all about the students. I wanted to quit my first year, but my family put so much pressure on me and convinced me to stay in a malignant situation. I was so depressed, didn’t seek counseling because I felt I had no time to take care of myself. There were several moments when I overdosed on sleeping pills because I didn’t want to wake up. By the grace of God I’m still here. Intern year was a complete nightmare and I had to deal with a few toxic attendings. Again I was doing my body a total disservice by not seeking help and over using benzos. I have never found any joy in this profession, even as an attending now. I’m not nearly as bad as I was in med school and residency but I still struggle with depression relating to this grueling profession. I no longer take benzos. Anyway, just wanted to share my story. You can publish this if it will help others. Thank you for shedding light on this. ~ Sara (just got this email from Sara)
Dr. Wible, Several years ago before I went to medical school. I had a good friend who was in his residency. He tried to commit suicide 3 times before he ultimately succeeded. Nobody would listen to him or take him seriously. At the time I worked at a psych facility where he was a patient which was the same hospital he was a resident at. When he was put on a 72 hour hold he was out in 24 hours per hospital admin because nobody took him seriously. He begged me not to go to medical school. He told me “going to medical school is like digging a grave. And the people standing over the top keep telling you to keep digging because it will get better. Only it doesn’t and you’ve dug too deep to climb out and it’s too late.” His 4 year-old daughter found him dead in their garage via exhaust hose in his car. I’ve come to a point where I completely understand where he was coming from. His biggest complaint was that even though he was paid for 80 hours of work as a resident he easily logged 130-140 hours per week more or less. Please share this letter. We need to tell the truth about what is happening in medical training. ~ Scott
Yep. I agree Pamela. Battery nearly dead. If you can get in touch with me I may be able to add some insight into how things might be changed. Drats…gotta go. Sorry.
How about doing this for all people, eh?
No doubt you have heard this but I will say it again.
You leave out the big elephant in the room.
10-15% of individuals who go into medicine, nursing, etc come from bipolar families and themselves have bipolar disease. This disease has 30-40% mortality over a lifetime due to suicide. The effect of this illness on a person gives them the empathy to be a good care provider.
No doubt the stress of training and practicing plays a role but fixing all these stressors would not eliminate the risk- it is inherent. Yes, I know classmates from medical school who have committed suicide-my best friend during those years hung himself after a setback-I have no doubt that he was bipolar. This is not blaming the victim-the risk of suicide in these bipolar Doctors goes with the territory. Source Dr Jamison of John Hopkins; You do a disservice despite all the good you do by not recognizing bipolar disease as having a role in many of these deaths.
We all come into medicine with our own issues no doubt. There is absolutely no excuse to 1) Teach by terror, public intimidation, and use other fear-based teaching methods 2) Allow sleep deprivation in medicine when it is outlawed in the airline industry, trucking, etc. 3) Omit the high risk of mental health issues from medical school websites and brochures. Obviously if I were depressed before medical school and I was alerted that a medical career would destabilize me, I would have the option of choosing another career. Kind of hard to switch once you have 300K debt, 7+ years of training, and suicidal thoughts.
My wife and I have lost two children to suicide. I am a retired physician. Our remaining three children have all struggled. Thank you for what you have done and are doing. This is an exceptional article.
Third-year med student writes me: “This morning I was on call and walked in to see the residents names on the white board with tally marks underneath their names. When I asked what it was for they told me that they started counting the number of times they considered killing themselves.”
This is a very opening article to many of us going through med school. Through my own experience, I have seen many of my colleagues and classmates going through similar experiences. Thankfully, we haven’t lost anyone, but there has been mental trauma through the years.
Even though our class is small and we stayed strong together, some have changed and others are going through many difficulties and stresses that are preventing from sleeping at night. Though I wish to help, that would compromise my well-being as well.
Clearly, awareness will be increased from my side; and I hope that after being doctors and life saviors, we are also humans with a ton of stress under us.
Of all the factors that make Med students and even attendings vulnerable, I think isolation is the worst. I actually think that the dreaded changing over of patients is a great opportunity to reduce isolation but the powers that be, look at it as lower patient care ( or perhaps a threat to the bottom line). Isolation is an abusers first weapon. Ruthless Hunger Games style competition is a great way to accomplish that. Then add sleep deprivation and nutrition deprivation and you have a brain washing playbook.
I see it as a consent problem since patients are not informed their doctor has been up so long and we know that study after study shows that the public would ask for another doctor most of the time. I think that is a failure of informed consent.
Hi,
I am a GP from NZ. I was trained in NZ and our system in NZ is much more friendly as it starts from high school graduate year to internship. A lot of us met our lifelong friends there at age of 18. There is no need to compete for specialist spots until you graduate and it is 6 years of happy life to make good mates (to me anyway) and most of us help each other while studying. There was freshman’s camp to meet new friends, we have study group and we join the social club in uni also, most of my best friends are in our study group and we formed our own hiking group later. In our first year of internship we also have buddy that we can call for help when we become the training intern (first year practicing in hospital). Yet I know 2 students that took their life in my 6 years of training, one in our year and one in the year after us- it can just be the stress of studying too much compounded with previous depression/ mental health issues. May be the issue is that the US university is too focused on academy and not a place for fun and development, where you meet your lifelong friends and fulfill your dream of being a doctor (as social buffers are very important, and it is hard to make close friends in a 4 year intense postgrads setting in US).
The other fundamental issue in the US medical system involves too much litigation that stress everyone out, from the teachers to the students and everyone starts to watch out for their own ass than practice medicine. In NZ there is a central governing system to prevent suing the medical professional. We may not make as much money here but we are happier in general is my impression as most the doctors I know from NZ are very happy indeed. Well you meet some unhappy one now and then but most are happy in my memory.
What you are doing is great, keep going, Pamela!
I still talk to my study group mate from med school about all sorts of issues, they are like my Balint group.
Judy that is FABULOUS!!! We should develop something similar here. So impressed!
no litigation?…so what recourse does the patient-public have when medical malpractice happens, or someone dies from a vaccine?…
So tragic and so sad that we throw such gifted people into the health care meat grinder. You are amazing and thank you for what you do. I am a nursing student and it’s bad here, too. You have to be *perfect* because nurses never make mistakes, not can they get sick, tired, or god-forbid–have a bad day! I lost my boyfriend, a brilliant Ph.D. Chemistry professor, to suicide in 2014. I found him dead due to a gunshot wound to the dead. I forge on with the goal of becoming a mental health nursing professional. I hope to help end this abuse and madness.
Hello!! I want to participate in your movement!! We have to do something greater about this!! Why is suicide among medical professionals such a big secret!! Nurses — We have to do something!
Hi, Im a physician from Dominican Republic, and yes we have the same problem , i dont have the exact number , but i can point out 2 cases of brilliant interns that committed suicide while i was in my internal medicine rotation during my last year of medical school. Yes been a doctor is challenging and stressful, but in my opinion its not the job perse that makes you commit suicide .The job is just a trigger not the cause of it , the real reason are underlying personal problems, maybe the person have self-image, self worth issues, think they are not good enough, have been trough drama in their lives among others, but the truth is that we all have problems , we all face difficulties in our lives but not everyone handle it the same way. Medical profession is not for everyone, and within medical profession not every specialty or area of training is for everyone either. Been a doctor, not only require long hours of study, learn about diseases and treatment self discipline, sacrifice and responsibility ,it also requires maturity, selfawereness,and a highly developed emotional intelligence. So my point here is, its important to find a balance between work and our personal lives and instead of blaming our work and our profession for our behavior, lets focus on working in ourselves, in our personal growth and in resolving our personal issues and the baggage we carry on in order to be more able to respond to the stressors and hardships at work and in our lives.
I’m a 3rd year medical student and despite being well aware of the psychological risks of med school beforehand, I went ahead and did it anyway. I tell myself every day that I won’t let the long hours or the mean people change me from being the super bubbly person I’ve always been. And last night a nurse told me “wow you must have just gotten here, you seem wayyyy too happy to have been here for more than 5 minutes. You’re probably the happiest person in the whole hospital.” I had been there for 13 hours and didn’t leave for another 3, but it was a little sad that I was the “happiest person in the hospital” when I literally didn’t do anything except not act like I hated everything and everyone, because that’s the mood people expect you to be in.
I heard your interview on OPB recently and it totally resonated. I personally have known 2 MDs from our hospital who took their own lives, in a relatively small community. I work adjacent to the medical community, in the prehospital emergency care arena. On thing that strikes me is, and I may be way off base here, the therapeutic distance it seems providers of all types must maintain. I am sure that MDs see pts all the time whom they connect with, and yet they have to isolate themselves to a degree, socially. My PMD is a great guy, I’d love to grab a cup of coffee with him, but there is a professional distance to be kept, and I am sure it wears on these human beings upon whom we rely for our health care. I would really like to know what you think about this. My grandfather was an OB back east and he died relatively young….
I thought your interview was awesome, it really made me think. Thank you!
Thanks Dave! Absolutely there is a problem with enforcing professional distance on a human being for 80+ hours week x 30+ years in a career. Connection is what tethers us to the planet. Habituated disconnection is deadly for one’s personal and professional lives.
This is SO very sad to read and has brought tears to my eyes, making it difficult to continue reading.my heart goes out to the families, colleagues & friends.
May I list a couple of points that may possibly be concidered?
Firstly at med school, (I’ve been saying in talks I deliver coming from lived experience) the power of language. It should be stressed how this needs to change /be delivered meaning the patient shares responsibility for their recovery. Eliminating some of this added stress. ( I’ve simplified things but you get the gist) I realise this doesn’t address emergency situations but recurring & secondary.
Students are encouraged to share their emotions/concerns once qualified and not be afraid of how this will inpact on their review.
A programme be in place addressing anxiety/stress etc and this should include their partner too. Often they are living in new areas away from family & friends. This adds extra pressure on the couple – how many as a result of shifts, anxiety felt by the Dr,also have broken relationships? This way they are helped further and where possible preventing the added anxiety of being alone and having heartache.This programme to be a requirement rather than optional therefore no one feels judged.
They may sound very simple things but possibly the foundations, the other important things following on.
Excellent suggestions! Yes, simple solutions are abound and just need to be widely adopted.
Looking for listening of patients designed clinic s. I live in Mpls MN. Any in this area?
DREW DIETL MD is your man! He is AWESOME!!
All residents and health care professionals who have been HARMED by ADA violations and the ABUSE of power from residency programs, licensing boards, and PHPs NEED to know about this new development!
Three US Senators recently wrote to the DOJ, demanding investigations of state medical boards and ADA violations (specifically medical licensing questions about mental health/substance abuse), PHP corruption, residencies and lack of oversight.
In summary, the senators say, “there’s something going on with state medical boards, their ADA violations are harming physicians beyond simply the licensure questions. We are going to get to the bottom of it and the DOJ needs to answer some specific questions ….”
https://www.wyden.senate.gov/imo/media/doc/Congressional%20Letter%20to%20DOJ%20re%20State%20Medical%20Boards%20Violating%20ADA%20with%20Intrusive%20Mental%20Health%20Questions.pdf
This is HUGE!!!!
Those who have been harmed here is your chance to have a voice! I would like to encourage you to first, write a letter detailing the ADA violations you experienced and how they negatively impacted your career and wellbeing, then submit the letter to your own state senators. Let’s increase awareness of resident abuse and help create policy change!
Share this with any colleagues, family members and friends who have experienced or witnessed these injustices.
Hi Dr Wible,
Do you think psych meds or withdrawal from psych meds has played a part in some of these cases? This is a very serious issue that people are not talking about, nor is the medical community. People seem to be in the dark about the dangers of psych medication. I’ve been watching a YouTube channel, Dr Josef, that interviews people that have themselves been damaged by these medications, or their relatives are interviewed because the person that was harmed completed suicide. I have a feeling this is why we lose a lot of veterans to suicide as they are likely given such meds by the VA to treated PTSD, and many of them likely have TBIs, which is another contributing factor.
YES! I know two cases off the top of my head that were benzo withdrawal:
Michelle Fernandez MD
Ben Shaffer MD
Doesn’t help that the medical profession drugs so many students (75% or so) who can’t keep up with the inhuman standards.
75% of med students are on antidepressants or stimulants (or both)