
“Have you ever been depressed as a physician?” I asked 220 doctors. Ninety percent stated yes. Yet few seek professional help. Here’s what depressed doctors do (when nobody’s looking). Some drink alcohol, exercise obsessively, even steal psychiatric meds. Still more shocking—I discovered that 75% of med students (and new doctors) are now on psychiatric medications.
“I was told by the psychologist at my med school’s campus assistance program, that 75% of the class of 175 people were on antidepressants,” shares psychiatrist Dr. Jaya V. Nair. “He wasn’t joking. How broken is the system, that doctors have to be pushed into illness in order to be trained to do their job?”
“During my internship, I found out that at least 75% of my fellow residents were on SSRIs or other antidepressants, just ‘to get through it’ because it was so horrible.” states Dr. Joel Cooper, “Depression, or a constantly depressed state, is more or less the norm in medical school and throughout one’s residency.”
“When I left my residency, I was alarmed to find out that about 75% of my fellow residents had started antidepressants since their intern year,” says Dr. Jill Fadal.
Seems the epidemic of depressed doctors begins in medical school. I wondered how best to verify this oft-repeated 75% statistic. Just then a student called to tell me what her professor said during orientation: “Look around the room. By the end of your first year, two-thirds of your class will be on antidepressants.”
I’m appalled. Yet she’s grateful. Why? Her school is so progressive. They normalize the need for antidepressants.
I must be out of touch. Do most med students require psych drugs for day-to-day survival? I turned my question over to Facebook: “75% of med students and residents are taking either stimulants or antidepressants or both. True or false?”
“It’s absolutely, horrifyingly, true. It is a symptom of a great sickness in MedEd.”
“Sadly I am guessing true as I prescribed some for my residents every year that I worked in a residency.”
“True, but I’m sure a lot is unprescribed.”
“I would assume definitely true, Ritalin, Adderall, energy drinks, ephedrine. Yep.”
“While working as a nurse at a major Army hospital, I was astounded by the number of medical students on Adderall or Ritalin.”
I’ve been on an antidepressant since being premed—18 years now. Little did I know it would be impossible to wean myself off and that my entire class was using Adderall.”
“True but most take them in secret as there are negative consequences and stigma that come with getting your mental health addressed.”
“Very true. From my practical point of view, I’d put medical students & residents at 100%.”
“I take both Zoloft and Adderall daily.”
“Very much so true—the percentages may actually be higher. I see it in my classes and I’m only a premed student.”
“If coffee counts as a stimulant it’s definitely 100%.”
“The only way I’d say false is to say it’s higher. I’d say a quarter of my class had to take a leave for a mental health break.”
Having received Facebook confirmation that most med students are on psych drugs, I then queried 1800 medical students via email with the same question and encouraged respondents to share personal experiences. To prevent professional retaliation, all quotes are published anonymously (with permission).
“I am one of the many who are currently on BOTH antidepressants (2 types) & a stimulant (amphetamine). I lost my very dear friend (also a classmate) to suicide in my third year of med school. I have been on psych treatment since then.”
“Hi Dr. Wible. The number sounds high, but whether it is right or wrong is anybody’s guess. I can tell you about myself and my girlfriend—we both just started our third year at a DO medical school. I use 100 mg Sertraline to treat panic/anxiety attacks that were very bad when we had practical exams. I am also very depressed, but the Sertraline does nothing for this. I was diagnosed with ADD in 2013, right before taking the MCAT. I have been on and off of amphetamines and Concerta since then. Then there’s the alcohol and marijuana for the end of the day when I just get too tired of thinking. I have been offered various benzos by my family doctor to help treat the anxiety attacks. I haven’t filled that prescription, but do use them (from a friend) occasionally to help sleep, escape life etc. This is coming from someone who never touched alcohol or other drugs/mind-altering substances until I was 25-ish right at the time of taking the MCAT. My now significant other also uses Sertraline, Adderall, and Benzos to treat anxiety/panic attacks and ADD. Coincidence? I doubt it. So my sample size is two, but 100% are taking antidepressants and stimulants.”
“True. I’m on them, and every student I know is on them too. I’m on both; never took them before med school. Same with all of my friends. Eek!”
“I do recall around board study season hearing from half of my classmates about sharing Adderall and getting Rx from doctors they knew. I was even offered it, but never tried. However, my coffee intake has definitely gone up since school to the point having trouble controlling my bladder. I also know of about half of my friends taking antidepressants throughout school. So I would guess at least 50-75% of my class took stimulants and/or antidepressants.”
“I tried two types of antidepressants in medical school, lost more than 200 thousand dollars, and almost ended up homeless from medical school. All [my depression and debt] started in medical school. Yet my passion remains.”
“Hi Pamela, I agree! Students are afraid to speak about it and I know some who have even asked friends/family to get meds under their name so it isn’t on their record. I finally started talking about it with my classmates and found that many of my close friends were taking them and we had individually struggled alone not knowing there were others going through the same thing. Also, if everyone’s doing it and it gives you an edge, then everyone else has to do it.”
“Sounds about right. I never needed antidepressants before medical school. And it definitely made me rely on higher doses of methylphenidate than I’ve needed in the past.”
“I never thought I would take study drugs. But I was near the bottom of the class in my exam results, and then found out that several who were best in our year were taking study drugs. I cut my losses and copied them. Low and behold, my results improved drastically. I don’t like it, but for me it is better than falling behind and doing poorly. All my friends at other med schools use Modafinil and Adderall too. They also use recreational drugs like ecstasy, cocaine and acid when they’re partying. Drug use is very common amongst the med students I know.”
“In my med school class, I’ve heard of people on antidepressants, on sleeping pills, using pot to calm down, and then also on some kind of uppers for test days and days after partying which the partying was to de-stress..but I have no idea if it’s 75%…I don’t know enough of my class well enough to have that info, nor do I think anyone does…there are usually cliques of up to 25 people, but for people to say they know for sure details of 75% of their class would be hard for me to believe but maybe…there is a lot of it, I agree with that.”
“True. As a med student I was on antidepressants. No different now I am intern. Having just finished 12 days straight and >120 hrs. I can understand why people are also using stimulants.”
“True. I only have four friends in medical school that I know well enough to know which meds they take. All are on both. I went to the university psychiatrist in my Texas premed program for depression he asked when I felt better I told him when I took my friends stimulants to study, I expected him to give me a verbal wrist slap instead he gave me a script. I was on a steady dose for years but the first year of med school I kept upping the dose to try and keep up, ended up deciding I needed to stop after one episode of not sleeping for four days and having auditory hallucinations. Failed second year when I quit them cold turkey, didn’t feel like I was keeping up without them so switched to Modafinil which is much mellower than amphetamine but definitely not good for me. Everyone started antidepressants in school even folks without a history of depression. Being completely honest 75% seems a bit high, but I wouldn’t be that surprised if it were true, in my n=5 study it’s 100%.”
“True. But that number may be higher or lower depending on the school and year in med school. I was on an antidepressant in the last month of last semester because all my other coping skills weren’t enough. I’m on summer break and I haven’t needed any medications to be functional and happy. My depression was entirely induced by the stress and frustrations encountered during medical school.”
“I was on an inpatient internal medicine rotation working 12-14 hour days 6 days a week (as a 3rd year med student) and would ‘keep it together’ at the hospital and fall apart on the way home, cry and sleep to cope. It was the first time in my life I felt suicidal, no plans—just wanted to fade away. My husband was afraid to leave me alone. I put myself back on the Lexapro, equalized somewhat and kept pushing on. That all happened around Christmas of last year. In June I finally was able to find a psychiatrist. He put me on a trial of Adderall. I was hesitant due to the abuse potential but decided to give it a try. With the two meds I have less anxiety, way better at prioritizing, and my focus is improved. I’m studying for step 2 currently so time will tell.”
“I take Effexor 150mg QD. In addition to 10mg of amphetamine salts TID. I used to drink 2 quad shot white chocolate mochas from Starbucks a day, but with the stimulant I threw myself into SVT too frequently.”
“I cannot talk about anything beyond what I know of my immediate friend circle but I have in mind about 10 examples of people who started NEW prescriptions for 1) Stimulants for studying and staying awake 2) Antidepressants and/or mood stabilizers and one person who was started on 3) Beta blockers for new onset panic. These are people with new diagnoses since starting school. I know a few others who came in on these medications after having hard times as premeds (or earlier, I don’t know) That’s just those who actually got the prescription…. As I’m sure you know there is unfortunately also a great deal of illegal procurement of prescription medications as well as abuse of illegal drugs. An increase in alcohol abuse is also a major concern. People are self-medicating left and right.”
“Oh, I would not be surprised! I know 10 people from 5 different schools and at least 7 are on either.”
“I am lucky to have a great support structure and have coped quite well so far without needing any medication. I am actually diagnosed with ADHD and have a prescription for two medications which I don’t really use. The pressure to use them every day rather than relying on my own hard-won compensatory skills is certainly there. Interestingly, I am not shy about my diagnosis and talk about it openly to destigmatize it but I have actually cut back on that because if I’m not careful I inevitably get a lot of classmates asking if they can have some of my medication. For a future doctor to brazenly ask for illegal sharing of medicine is worrisome to me but again I do understand the pressure (to stay up just one more hour studying) that drives the behavior.”
“Popping prescription bottle caps and chafing of pills while studying in the library is a fixture of how daunting the pressures of medical school really are. Med school libraries are dungeons where souls came to die. You’re surrounded by absolute dread—the look of despair painted across the faces of your fellow classmates who feel at any second their life could be ruined with one failing grade. Most of my friends were on SSRI’s, Benzodiazepines, and various types of stimulants. I once asked a friend if he had anything to help me go to sleep and he recommended Lorazepam, which he gave me. The ‘top student’ in our class was rumored to be a serial user of cocaine. To avoid having a drug test reveal his dirty little secret prior to third year, he took a hiatus by engineering a family emergency to give himself adequate time to pass the contents of amphetamine (he passed). Elicit substances in medical school may seem like taboo to lay persons, however in our eyes, it’s a natural and regular experience. In fact, it is astounding how many medical students (myself included) smoke marijuana in order to experience a night of restful sleep. With each puff, it’s as if I escape a bit from my hectic reality. A reality dominated by judging, vengeful, and heartless administrators/faculty who can care less if we live or die, as long as we perform on USMLE Step 1. Yup, its that bad.”
In 1990, even I was severely depressed as a first-year med student. So my mom (a psychiatrist) mailed me a bottle of Trazodone. I thought I was the only one crying myself to sleep. Turns out occupationally-induced depression is rampant in medical training. Now schools dole out antidepressants like candy. Stimulants are used by med students like steroids in athletes. So where do we go from here? Should “progressive” med schools distribute samples of Zoloft and Adderall during orientation?
Problem is physicians must answer mental health questions (right next to questions on felonies and DUIs) to secure a medical license, hospital privileges, and participate with insurance plans. Check the YES box and be forced to disclose your “confidential” medical history and defend yourself—again and again for your entire career. Treated like a criminal for taking meds to cope with the torment of medical training (and practice).
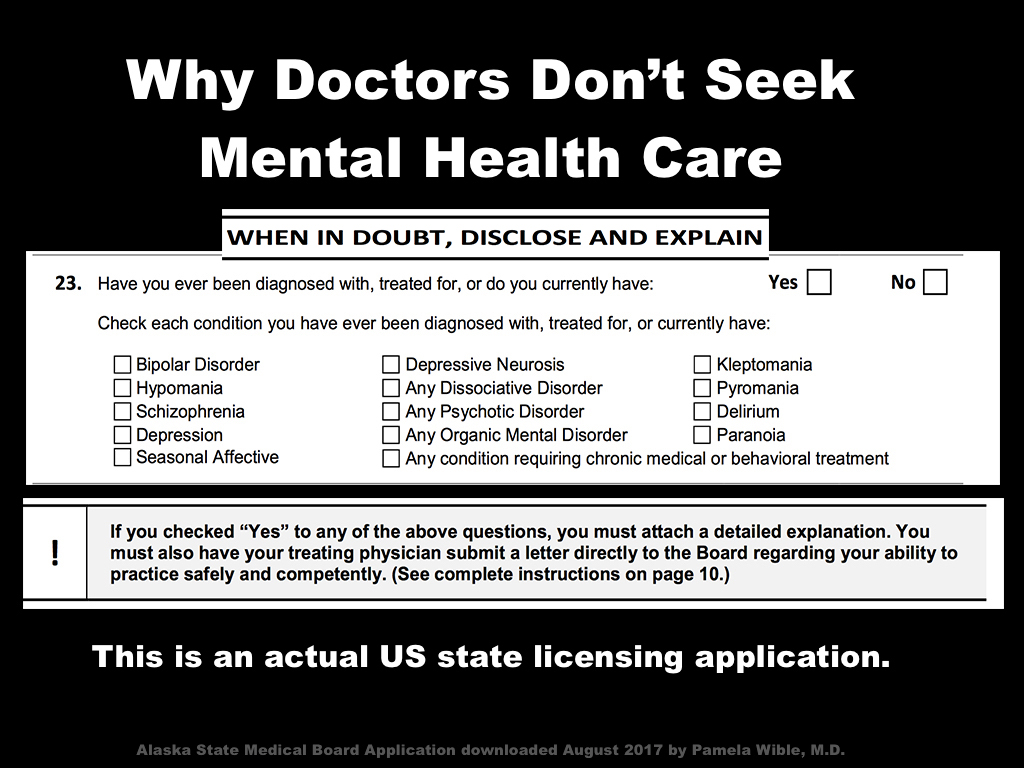
Maybe that’s why so many future (and current) physicians sneak drugs and go off-the-grid for mental health care.
“I’ve been in practice 20 years and have been on antidepressants and anxiolytics for all of that time,” says Jason. “I drive 300 miles to seek care and always pay in cash. I am forced to lie on my state relicensing every year. There is no way in hell I would ever disclose this to the medical board—they are not our friends.”
What if we stop the mental health witch hunt on our doctors? Why not replace threats and punishment with safe confidential care? What if we address the root of the problem—the great sickness in medical education—rather than shifting blame to 75% of medical students for not having enough serotonin or dopamine or norepinephrine in their brains?
As scientists, we can’t continue to approach medical education reform as a neurotransmitter deficiency in medical students. Can we?
___
Pamela Wible, M.D., is a family physician in Oregon. She is happy in her solo practice and takes no psychiatric medication. Turns out her depression was environmental—entirely related to the culture of medical education. Dr. Wible is author of Physician Suicide Letters—Answered. View her TEDMED talk Why doctors kill themselves.












Pamela
I am a Podiatrist that graduated in 1979 Back then only 50% of the graduated got residency programs.
I was #4 in my class which did not mean much but I was able to get a 1 yr surgical program.
I remember the first hospital that I rotated through and they did not have a Podiatry Department so I worked in the surgical department assisting all of the MD surgeons and even Orthopedists.
I recall that he MD surgical resident”s had to work 36 hrs straight, and I recall that most of them relied on drugs to keep going.
I felt sorry for them because They were under so much stress which I did not have fixing Bunions and hammer toes
Podiatry NOW has changed where the graduating student must complete a 3 YEAR Surgical Residency JUST to be licensed.
Look How All these changes occur?
So you are telling me that it now takes 3 years to learn how to do a bunion surgery???
Hello Pamela
Our students have to complete a 3 yr surgical residency
just to obtain a license.
Many go on and do fellowships in wound care,reconstructive foot and ankle surgery
after this type of training many of these new Podiatrist’s over 50 % female by the way become certified to repair fractured ankles and to do internal ankle implants. I always tell my 3rd year students that I am envious of them all because they will get so much more rigorous training that I had and will not just be Fixing bunions.
Sincerely;
Steve Levitz DPM
Aha! Now that makes sense.
I am an internationally trained medical doctor who have worked closely with attending, fellows and residents in training in acute settings in the US. I have been following your body of work for over 2 years now and wanted to drop in to say I appreciate you being a voice for those who have none. I see the “martyr syndrome” in medical training and life whether in the US or internationally, it is same. I have had residents, pharmacists all in training tell me they cope with wine or antidepressants…it has made me question a lot of things. I have seen how we as doctors who supposed to be the healthier one eat fries and coke and pizza to deal with stress. My question is how can we make medical education and training not an act of “self-death” considering we all have different levels of self-resilience and support system? Thanks for being a voice and a support system. I respect your body of work.
The first thing we need to do is be aware that this problem exists and label it honestly as a SYSTEM malfunction (not a defect of the individual). Once we can honestly discuss the situation, I’m certain the solution will manifest (we all certainly have the IQ and resourcefulness to solve this once we stop burying our heads in the sand). Big roadblock is the resistance to declaring this a problem. Medical institutions seem to be doing nothing to address the underlying SYSTEM issues and prefer to continue blaming the victims by sending them to work-life balance PowerPoints, resilience workshops, and psychiatrists (likely none of which they would need had they chosen another profession)
Richard Layard, the UK’s renowned economist, has recently published significant observations pertaining to the extent competition is self defeating to society as a whole and has offered his insights into more than one area of medicine as specified topic consideration. My interpretation of his writing is comparable level of appalling shock and recognition of substance misuse as coping strategy amongst medical personnel to Pamela’s, my own, and others’. “How can we encourage outcomes we most want to see – in our culture, in medicine? In ourselves? How can we increase the stability of family life, of social connection?” – to quote him, in part.
A recent statement made by a spokesperson of the American Hospital Association has been to the effect hospitals are working on better ways to communicate with patients, e.g., teach back quizzes and education videos.
Glaringly missing in this commentary is mention of doctors. The hospital, the patient and the doctor are the health care team, can that be conceded? What happens when the door is closed on one of those — MD’s who are stringently penalized for any admission of challenges related to depressive state triggered by anxiety perpetuating in reaction to stress? Just what one would suppose — chemical dependency and, sometimes, suicide.
This conclusion is not drawn on conjecture. It is based on fact. And yet….. what is being done to address this tragedy?
Pamela’s instigating talking about these issues opens the door to possibility of positive change. Our time is well justified to wedge the door farther open, joining her in the opening she has created. There is no limit to what change can be instigated, one voice added to another’s.
Too often doctors have no value other than revenue-generators for corporate medicine. Cease to bring in the bucks at the level demanded of you and see how long you last in your job. Physician mental health isn’t even on the map.
I wonder how many of them got hook on those drugs thanks to the drug companies?
I know lots of docs who raid sample closets.
Dear Pamela, This explains the high rate of suicide. These drugs cause akathesia, not unlike the akathesia that is from the antipsychotic drugs. This causes a very powerful agitation, like you want to move constantly, but of course, in med school, you cannot. This drives anyone, any sane person CRAZY. You feel transformed, in a really bad way, driven, driven mad. I can tell you. Only once did I feel it, but it was like a drumbeat inside me. This is why kids do Columbine-style shooting and why so many mothers kill their kids during “treatment” for post-partum. Antidepressants cause violence, and the pharmaceutical companies (and your doctor) do not want the public to know. Yes, these drugs are killing our kids. Not only that, long term use causes early death, possibly early dementia, chronic pain, and heart trouble.
Anyone out there please check Mad in America dot com, you will see many resources there.
Julie Greene, MFA, Escaped Mental Patient
We are turning our future physicians into polypharmacy patients. What IS the impact of Adderall + Lexapro + marijuana + alcohol + sleep deprivation + STRESS???
You dont understand Its a brain disease.
Its scientific, just ask your doctor.
yours truly
paitient doctors f**ked
It’s the patriarchal system. Any medical training that demands sleep deprivation should be closed.
The exploitive nature of the medical industry starts at school and continues until the USA, despite its fame for health care, is harmful to many, partially from its pharmaceutical profit ties.
Once women entered the medical field, changes began.
But it is a CULTURAL problem of profit and exploitation.
Spot on. Systemic human rights violations that trickle down from abused doctor to med student to patient. Free ebook (quick 20-min read) explains the cycle of betrayal that sustains the abuse cycle in medicine: Physician Betrayal: How Our Heroes Become Villains.
I don’t like hearing this. Better than drugs would be coping strategies and mental health evaluations to really see if all of these drugs are necessary. You have to learn to cope with life with drug fog. My concern is that their patients would be tossed on such medications without an appropriate evaluation. They are learning this lesson in the wrong way. People need to be properly evaluated before such therapy. Legitimate therapy for legitimate diagnosis – it is not being done. It is not clear why it is not being done. I actually question if this is all bogus!
I agree with you. Sadly, this is not bogus. I wish I could say I just made all this up. I’m as shocked as you are.
Unfortunately, most “mental health evaluations” these days involve checking off symptoms and prescribing, which is part of how we got to where we are. There is little to no acknowledgement that stress, abuse, bullying and trauma are the biggest contributors to depression and anxiety. The basic message is “You should be able to cope with this, and if you can’t, YOU have a problem and need to be fixed!” The whole system works this way, and a lot more people than just doctors get this kind of “treatment” from the system. To illustrate, a study in the recent past had grad students go to residential treatment facilities and ask the residents a range of questions, including whether or not they have experienced traumatic events in the past. Not surprisingly, over 80% of the residents reported trauma histories. But what WAS shocking is that only 20% had trauma histories recorded in their files!!! So a full 60% of residents were comfortable sharing their traumatic histories with a total stranger, but they were either never asked by staff, were uncomfortable telling them, or the staff thought it unworthy of inclusion in the file! Of course, there is a good chance that more of the remaining 20% either didn’t recognize or didn’t feel comfortable sharing their traumatic experiences, so the disconnect is probably higher. Bottom line, our current mental health system actively ignores the importance of stress and trauma, and not only doctors, but a very large proportion of their total patient/client base suffer as a result.
Thank you Portland!
There is much that can be said for safe sharing of traumatic histories for virtually every individual. It is a mental health dialogue that needs to be included as early on as possible. We are now realizing that without this dialogue the door to psychopathy is left open. Dialogue is the new community.
The suicide rate for nurses is half that of physicians. Anecdotally, I don’t think the rate of antidepressant usage among nurses and nursing students is anywhere near the rate in medicine. We have no match. We do not compete against each other in school. We tend to help each other in school, even greatly so. I don’t think of my classmates as competition. Instead, I see them as people to turn to for help and support. If we stumble, we can take another semester or two to finish. There’s no shame and it’s not disruptive or career limiting.
Nurse practitioner students are somewhat analogous to residents in level of responsibility, but the similarities mostly end there. We have to work hard as NP students and put our social lives on hold, but we have good lives. We’re not sleep deprived and we work together. Faculty members repeatedly tell us to take care of ourselves and get enough sleep. As an undergraduate nursing student working a 12 hour shift, I was caught skipping lunch. I was dressed down quite firmly being told that was unhealthy and inappropriate behavior. I never made that mistake again.
On the first day of orientation at undergraduate nursing school and also at graduate nurse practitioner school, we’re told to work together if we want to succeed. In NP school, everybody is an RN, everybody is a peer. Faculty members listen when NP students bring their clinical expertise to the classroom. We believe we can all learn from each other. None of us know everything, but we all have expertise. We’re comfortable collaborating with each other.
Depression is twice as common in nursing as in the general population. Research comparing western medical students to nursing students is lacking. It’s my opinion nursing school is psychologically healthier than medical school. I highly confident NP school is healthier than medical school or residency.
NPs and nurses are not subject to the same lengthy training and abuse so I have found that they are much healthier emotionally. Though I do hear “nurses eat their young” I think overall they are more collaborative than competitive (after all they are not going for limited residency slots requiring them to throw colleagues under the bus). More regulation and legal protection. Less sleep deprivation. Break rooms. Lunch breaks. Mandated by state law (somehow these don’t apply to doctors!). I think having a more female-dominated profession is a HUGE benefit when it comes to nurturing and caring for one another. Not that machismo our-way-or-the-highway mentality so common in medical school. Still we all need psychological support for all the tragic and terrible things we witness in the course of a day in the hospital or clinic. Yep, we all need a good cry every once in a while (and not just numb out on SSRIs!!)
From my experience of training few NP in my office,students close to their graduation from the program their functioning level and responsibilities are closer to 3rd year medical students. After completing NP program they should go to NP residency.
It is an outrage that more competent medical specialties residents make half of the money of starting NP’s or PA’s.
And it is an outrage that they are held hostage after graduating med school, not allowed to practice without residency, yet NPs are opening independent clinics with far less training.
I wish NP residency was an option. I believe the majority of NPs want to provide high quality care however do not obtain the proper education to do so. I am forever grateful to the doctor that continued to mentor and train me for years after I finished my formal education.
Hey Pamela,
Hope all is well.
I think more med students, resident, and practicing physicians would never again need happy pills if their patients paid for services rendered in bitcoin.
Perhaps we should start charging in bitcoin?
Blockchain tech and a decentralized ledger can save healthcare and maybe even save our sanity.
Just look at Patientory. This blockchain tech company will both prevent hacking into EMR, but also provide a way for everyone to view EMR from other institutions, clinics ect. Just check it out if you want to know more.
Sincerely,
Dr. Bitcoin
Being chronically undervalued is a HUGE stressor for docs and many dream of working at Starbucks or even as dogwalkers or something to get away from the stress and terrible working conditions.
Right on Pamela! The hardest part of moving on to my next career, whatever it might be, is ditching the golden handcuffs! Dog walker would be great! The dogs love you and you get to walk for a living!
And you get to be human! Plus you might earn MORE money! Can you believe that? Read this: https://www.idealmedicalcare.org/blog/doctor-earns-dog-walker/ (I may have already posted but a great wake-up call on other career options nonetheless)
As I read this, Doc, it seems to me that the system is causing a life meltdown here. I’ curious about how big a part spirituality, in any form, plays a role in the physical and mental health of med students and interns, and in the medical community generally. Our culture has cost us our connections to the deeper forms of spirituality and separated us. A lot of my community’s ability to withstand the culture around it derives from some deeply shared sense of the collective good and some sort of shared spiritual core – well grounded that way. So we can work together on a lot of things. I was hoping that the medical community could really become one – but also better integrated into the rest of the community. I think you’ve done a great job of that, in Eugene, and in fostering the heart of it everywhere. I’m reflecting these days on how to take such heart-centered work to scale – to the core of the system. Sorry about the second intrusion. Your work very much stimulates reflection. CS
Loss of one’s connection with the original purpose for entering medical school is a HUGE part of the problem. These young bright-eyed humanitarian idealists who just want to help people are preyed upon financially (300K student loans) and emotionally/physically (sleep-deprivation with 80+hour work weeks witnessing unbelievable human trauma and suffering) without the support they need to thrive in a profession they once loved. Tragic for all.
After all medicine is a spiritual calling for many and the dehumanizing process of medical education quickly beats that right out of the students.
Wow, if this stat is true, this is both sad and scary. Sad because there is obviously something wrong here either with overall medical training, hours, expectations where we are throwing pills at students/residents and scary because we have sick doctors trying to help everyone while often times learning in training to neglect themselves and their needs. Unfortunately, this is something they continue to do throughout their careers which leads to burnout and depression. Wow just wow. I feel for my colleagues. We sacrifice ourselves much too often yet typically described as always rushing, and uncaring and even greedy. It’s a shame how many doctors are sad. I can’t name any of my friends who would do it all over again if they had to. That’s a problem.
I am as shocked as anybody with these stats. It’s unreal that we in medicine have allowed our future physicians to suffer like this. How can we ignore this?
tell them to write a suicide note about why they should commit suicide
and a love note about why they are worth loving
and notice which pile of pages is higher
it wakes them up and they start sharing their pain and healing
when done in schools the suicide rate goes down
Thank you so much for your in-depth research!
I certainly don’t think you are making this up!
I know many doctors who have made awfully strange mistakes or behaved so Terribly with myself (as a patient) and others,that my First assumption was always that they were overworked, stressed, traumatized and exhausted.
I commend you for getting this information out there to help reform this whole system.
When doctors are sick, it can lead to sicker patients, as we all know.
I have so much compassion for all medical professionals. It is grueling work.
I’m trying to learn more about the secret medical-abuses to patients that go on inside Psychiatric wards. I have often assumed it was primarily a result of a really broken Medical System, too.
I hope you are not struggling too much yourself, Dr.Wible.
Thank you, again, for your service to all of us.
-Well-wishing for all medical professionals and patients,
-Meredith Williams
Doctors’ health is too often sacrificed for short-term corp med financial gain. The long-term impact of this chronic institutional abuse to the health of patients (& our “health care” system) is profound. We are just beginning to understand how profound.
Ever since I can remember upon completing my residency and fellowship in the late-80s physicians have been overworked, their opinions discounted , bred in a fierce culture of impossible competition rather than collegial cooperation was the norm.
I can even recall situations where residents were prescribing psychotropic and antidepressant medications to each other in order to cope with in enormous expectations made of them.In fact Friday nights were normally reserved for ” Liver rounds” ie., go out and drink ( not because we lacked pressure cooker stressed lives) .
Working continuously for 36 hours often lead to dehydrated residents in the emergency room requiring IV’s to recuperate go home and come back and work again .
No compassion kindness or even mercy were shown to those who they expected to emulate these qualities to their patients. I myself was not even given the time off as a intern to be at my wife’s side for the birth of our first child( Luckily she gave birth at same hospital I worked at ) so despite being promised the Chief residency position I resigned. That’s right, new father unemployed physician ( for 1 week, but for that 1 week I was devastated; I fortunately found several offers and a newer and better program).
Medical residency programs instructed their chief residence to systematically miss treat their own colleagues for hopes of career benefits .
What doctors in full participation with these program directors did to them selves continues to be doled out to them today on a regular basis by not only program directors medical schools but insurance companies the government and society as a whole . Physicians are held to unrealistic standards and are expected to cope . They are denying us our very humanity and penalizing us for even being physically or psychologically ill as a result. In essence they sweep us under their acceptably and politically correct carpets, remove our injured from world view to conveniently cover up their continued crimes against our very humanity.
These assaults must be publicized, the perpetrators openly identified, shamed and punished. Our affliction must be properly identified as occupational illness, hazards and induced disease and accorded appropriate care, compensation and full rights afforded to our effected colleagues just as would any other occupation under our laws. The abusers must be identified and prosecuted to the full extent of the law. A new chapter in occupational medicine effecting medical students, residents and physicians must be codified and enforced. After all, are we any less human than anyone else?
It’s never too late to stand up for our own rights and demand equal treatment during health and illness and stop this rampant abuse of our most noble profession the world cannot afford to go without. The time to stop talking and start doing is now!
Class action lawsuit. Need a heroic attorney (or a few). Mostly victims need to stop consenting to being abused. So proud that you stood up for your RIGHT to be present for the birth of your child. None of this will change unless current doctors stand up against these human rights violations as they will be continually inflicted upon the next generation of doctors. Public outrage is mounting and once this film debuts the world will know the truth. View Do No Harm: Exposing the Hippocratic Hoax movie trailer here: http://donoharmfilm.com
Sad, unfortunate and a national disgrace.
Just a note to say we are still following you and your work. Attitudes are so hard to change… keep up the good fight!
Dr Pam…It really saddens me as to the distress medical students are forced to endure. It may be one thing if you knew when signing up you were being medically trained in guerrilla warfare;however,most students don’t strike me to be able to carry such burdens.
NOT UNTIL THE STEREOTYPICAL VIEW AND CONDESCENSION ABOUT MENTAL HEALTH ISSUES CHANGE WITHIN THE MEDICAL ARENA ITSELF,PEOPLE ARE TERRIFIED TO OPENLY SEEK APPROPRIATE CARE. The military makes asking for help,the end of your active duty career,it goes into the medical records and it decisively affects everything you then attempt to do. UNLESS AND UNTIL THE MEDICAL FIELD AWAKENS TO REALITY PEOPLE WHO NORMALLY COULD BE POSITIVELY TREATED WITHOUT NEGATIVE AFTER EFFECTS,DO SADLY SEEM TO BELIEVE ALL IS LOST. ONE SUICIDE…IS ONE TOO MANY.
Insanity seems to reign supreme,soldiers/veterans with PTSD are being given ECSTASY and Marijuana as treatments. How can this be helpful??
Pure, pharmaceutical-grade “ecstasy” is a chemical called “MDMA”. When given in micro-doses, in clinical settings, under careful supervision, it has shown dramatic positive results. Cannabis in various forms has also shown very promising results. It is NOT simply a case of seeing how many bong hits of skunk you can rip. Also, edibles, tinctures, and extracts of Cannabis are being used with excellent results, and few if any serious problems. CBD, usually in oil form, has proven effective for a whole range of medical conditions. Pretty much everything you *THINK* you “know” about Cannabis and MDMA is blatantly fake news and false propaganda spewed by the FedGov and PhRMA. The 20+ daily suicides of active duty and veterans is the result of the lies of the pseudoscience drugs racket known as “psychiatry”. The psychs use of so-called “polypharmacy”, i.e., multiple neuro-toxins, is the REAL KILLER. Please educate yourself.
I posted this article on Twitter and Facebook!
Thanks! Awareness is the first step to the solution. Can’t solve a problem nobody knows exists. Appreciate your efforts Juan.
People have NO clue…
Average person? No clue.
Those of us in the field? Know it well….
Im hopeful it will improve…. or God help us all.
Let’s take action now. Not sure we can wait for God (at least that approach has not worked yet).
A few more comments rolling in via email:
“But I’m really pissed off at this- we really have to do something. I see my colleagues wasting away, afraid of their own shadows, drowning in misery and despair.( maybe that’s why big Pharma sponsors dinners- to get Docs a bit inebriated- and believe me they do! But that’s not reportable apparently)”
“I absolutely agree with you. Medical training and medical practice are toxic environments. I appreciate all the ideas about resiliency and burnout treatment/prevention, but why is the onus on the physician to adapt to an unhealthy environment? The answer is not antidepressants or adderall but a change in the paradigm!”
“Pam, Great god amighty. Can these data be representative? I get it that med school and residency training are brutal……but so are a whole lot of other human ordeals. I get it that Big Pharma has churned out many drugs that affect the way people think, feel, and behave, and has pushed them relentlessly. I get it that psychiatrists have been turned into pill prescribing machines. But I dont get it that such a high percentage of medical students and residents really need these kinds of chemical escapes. And I dont get it that the benefit/harm ratio is favorable long term. But I also do not know the answer to that question. What are the short, mid, and long term outcomes of such rampant concealed psychiatric medication use. Any good references on that which you can recommend?”
From anonymous doc tonight: “I have corresponded with you before, bless your heart for hearing me, but now that I have sought help for alcohol abuse, ptsd and complicated grief I am unable to obtain health insurance off the ACA market. It’s ironic to me that as a hospitalist at an urban academic center I kept alive easily 15,000 patients (and taught others how to do so) but taking time and trying to save myself leads to a lack of coverage and fucking slim offerings in mental health help. I paid oop for 90% of my care (secret, under the table), but still cannot get insurance based on one pay for mental health and an rx for naltrexone, I cannot get insurance.”
Letter submitted from a doctor who wishes to remain anonymous:
“Hi Pamela – these letters could have been written by me. I had no idea what ADHD is before 3 year of Med school. After reading this, I wonder how all my classmate “gunners” A students really got their grades… But hey, it’s all water under the bridge… thankfully! I saw guys dipping tobacco during tests and pretending they were sipping drinks, so they can spit… (ok I went to school in Texas and this may be a regional thing) but really… I carried a bottle of (then legal) ephedrine in my short white coat and proudly showed it to surgery residents while waiting for my turn to scrub in. I told them in my home country it was a common remedy for asthma (which was true) and now it helps me to stay awake during 36 hr day… without the side effects. No really, that’s what I said and did. I really liked Surgery but didn’t do well after a night up in OR or ER barely able to pretend to learn and quietly hating it. At about 5:30 am, I would feel an acute sense of despair and strong urges to just walk away and drop everything. But hey, my friend OTC ephedrine inevitably saved the day. (Without the side effects of course.) I received great reviews and overall had a pleasant experience during this rotation.
Fast forward 6 months or so. A medical resident, well respected by me, suggested In passing that I have ADHD because I was bored during never ending rounds in the hallways and, at the same time, was really worried about discussing patients’ confidential info in public… (I guess I looked preoccupied and distracted. The truth is – I wished that I would be the only student answering all the questions – I would have really learned the stuff much quicker that way and we would’ve been done in half the time!). I got a referral to an expensive private psychiatrist who diagnosed me with ADD after 10 questions and asked me what I would like to be on. I said ” you are the doctor, you tell me.” And he said” it doesn’t work this way, you are the patient – you tell me.” I was really clueless as I haven’t been through a psychiatry rotation yet. I saw a TV add for Adderall XR – behold, I got a script for 60 and, in the following months, 90 pills of 10 mg tid. (and Xanax to sleep at night for good measure). I started getting “A”s on tests – to the endless surprise of my seasoned professors. Wow!!
I need to add that as the “expensive private” doctor was saying this to me – I literally saw my respect for him fall below the floor… but I stepped over my dignity and continued to see him for monthly Med checks for a while…
The price was periodic self loathing but hey, my grades improved! Who needs self respect in Med school – you are really not much of anything, so the “positive” feedback and grades at the end were the only thing that really counted, right?! …
The end of my treatment experience was an interesting one. One day I called the office to pay a bill which did not arrive in the mail. No one answered, and I had to get creative (and rather tenacious) to track down someone at the same office building. I was told by an office assistant that the doctor lost his license due to inappropriate relationship with a male patient. I was off the hook for payment and got a freebie but felt confused and violated in a way… Still do. I went to the board of medicine website and confirmed it. Wow… I still don’t know how I really feel about this and haven’t processed this fully, as my colleagues would put it. Oh well – my PCP was willing to give me the scripts and I just left it at that.
This is only a half of the story. Another half is about antidepressants but I’ll save it for another day. And then, of course, there is another story for the time in residency. (In a different state – I saw no one dipping tobacco. Just lots of coffee – which seemed to be
more culturally acceptable practice overall.) And with all of that, I went to a student friendly medical school. No one in my class (or other adjacent classes) committed suicide or died under mysterious circumstances, as far as I know (or remember). My teachers (especially in the first 2 years) were kind and compassionate people. My school had an official open door policy. Professors and administrators gave us their home numbers in case we get stricken by fear before a test or have difficulty coping in any way… Looking back, I really can’t complain… But “here is my story and I am sticking’ to it. ” 🙂
(You really can’t make this stuff up!)”
This is truly insightful and sadly…its ALL TRUE. I am a Canadian Physician and despite being trained in a different country, all this is true in Canada as well. I went to a medical school that is well respected and it does amazing work training young physicians. However the competitive culture and the emotional and physical strains of training are simply ignored. Bright, young and vulnerable minds who have never known failure in their young lives often are left with few options for coping. Mental Health is often relegated to ” lip service ” Young physicians may be required to do 3 days of continuous on call ( especially on weekend call) leaving them exhausted, ill, and frankly , not in a good position to make critical decisions for patients in life threatening circumstances. They are often the least experienced, caring for the sickest patients. The young physician feels ill prepared and without proper back up. The internal emotional toll on ( especially) caring physicians is indescribable. The physician is left making more critical decisions in this sleep deprived and often traumatized state….with no acknowledgement or support … I for one have seen many young physicians turn to alcohol, and drugs to cope day to day…I have also seen young physicians and older more experienced ones have their lives cut short by their own hand ( typically by gunshot for men, and drug overdose for females)
There is typically little warning…because you are not permitted to talk about it. The lucky ones seek and have the fortunate experience of having an excellent therapist/psychiatrist …This is probably easier to fund in Canada rather than the US because of our universal health care system. I don’t pretend to have good answers to this systemic problem. First we need to acknowledge the reality of the problem. Second we need to provide support and resources for health providers so affected. We certainly now acknowledge the reality of PTSD in the Military and also in The real of First Responders. I believe that the symptoms of severe anxiety, and panic, and chronic sleep deprivation and severe depression leading to physical exhaustion and personality change are related to PTSD relating to the complex, high stress, and high stakes experiences of medical practice every day. Governments and insurance companies everywhere are laser focused on containing costs in a chronically underfunded system ( both sides of the 49th parallel . The result is that wait lists expand, time for patient care is compressed, and poorer medical care is the result .Patients ( to their credit) are more informed than ever, and expectations for perfection in care are higher than ever .Then add in the litigation conscious society we live in. Its a perfect storm. Expectations of perfection, from human beings who expect perfection of themselves, who have less and less time for individual patients and less and less resources for the purpose of care. Mistakes will be made. They are usually totally honest mistakes. But mistakes never-the-less. Perfectionists making mistakes takes a huge toll on the provider. Add exhaustion, sleep deprivation, and day to day stresses of revolving door medicine. Add an unexpected legal action. Add family problems . Add human frailty. Add a lack of a sense of spiritual and existential purpose . The result is emotional distress…which does NOT go away. Because….tomorrow you get up to do it ” all over again” Do this long enough, even the most resilient will fall ….and some will chose an exit plan … I am aware of at least four physician suicides during my career in my community. I am also aware of many more health care providers who now take antidepressant medication, anti-anxiety meds and I now am aware that many medical students and residents take psychostimulants. A simple observation. This is not a healthy system. Who benefits from this type of system ? A short list of those benefiting from all of this ….. Politicians who wish to perpetuate the myth that health care is ” free” and available to “all” as a social right ( as we find here in Canada) In the US, “for profit hospitals” , and a large pharmaceutical industry benefits ( and their investors) and large “for profit ” health insurers(and their investors) Large Insurers really control the system in the US . Our single payer system in Canada leaves this privilege to Provincial Governments. We all need a ” reset” in a system now gone ” mad” Principles to start would be putting the patient back into health care….and that includes ” patient responsibility and accountability ” In our country …patients visit a physician without financial accountability. This is a crazy system that leads to the inevitable result that the demand for service is infinite and the resources are limited. The physicians are left triaging patients for priority of illness….If you get that wrong…you also get sued ! The pitfalls in all these systems are beyond what a ” mere human” can reasonably handle with full perfection day after day ….It is quite impossible actually ….
Patients need to take a higher level of accountability. Governments an insures need to provide more resources for the job on hand. The truth is….the provision of all this care for everyone, every day, in an affordable system is structurally impossible….Given that reality….perhaps some care and concern and support for the providers would be a good investment. As long as physician suicide rates rise, and a system of medical education that leads to PTSD type symptoms in care givers and without supports …will lead to a worsening of the overall system, and its ultimate collapse. Are government’s listening ?
Great summary of our dismal situation. I’m one for getting to the root of the problem. Hopeful kids enter medical training and leave with their hopes and dreams shattered. The central problem we need to address is medical education. What are we doing to these beautiful new doctors who just want to help and heal others? It’s unconscionable. What kind of civilization does this to its youth?
For everyone waiting for the scientific study and all the data, I fully support a more robust investigation of this topic (though have doubts that many med students would feel safe enough to participate—especially if in any way linked to their email or identity). In the meantime, shall we not do something about this (obviously) broken system that torments so many into drugging themselves—legally or illegally?
The tide turned when Medical Schools became “for profit” non profits.
$1 Million Mistake: Becoming a Doctor
There is absolutely no reason why research of this potential magnitude should be published in credible journals using anectotal evidence and heresay as evidence! I do not doubt the possibility medical students and medical professionals are relying on prescription and herbal supplements for mood, sleep and cognitive supports. A recent credible research article identifies depression to be the major source of disability in American society and that even when workers feel better and return to work, cognitive deficits in memory, judgement and motivation can linger for up to a year. As a Stanford Fellowship trained and board certified emergency physician, I cannot emphasize enough how much shift work disorder, chronic sleep disturbances due to pain and frequent interrupations along with constant exposure to high ambient noise environments and toxic interactions with patients and stressed out medical and emergency personnel, adds negative transferance to mood and self esteem. The phenomenon of physician suicide cannot be addressed until we recognize the tip of the iceberg…that doctors in training may be relying on prescription medications that in themselves are contributing to death by overdose. This study needs to be conducted with the same rigorous epidemiological and population based standards we apply to all professional research studies to avoid disseminating potentially non factually based and legally defaming information!
I’m all for more research. I’m shocked by the numbers of med students requiring meds to make it through the day.
As an addendum I would add it is even more likely that 100% of medical students and medical professionals have used OTC and or prescription sleep aids at some point in their career! The benzodiazepine class sedative hypnotics are irrefutably linked to cognitive and memory impairment, cardiopulmonary depression and and the class of medications, along with opiates, most often seen in the cocktail of prescribed medications detected on autopsy in accidental and deliberate Rx overdose deaths.
You are probably 100% correct on that one!
It would help if the psychiatric profession began to shift away from the “it’s all in your brain” story and start acknowledging that the majority of “major depression” and “anxiety disorders” are a reaction to adverse circumstances (like Med School!)
I am a physician assistant in internal medicine, I count my lucky stars I did not go to medical school. 75% sounds right for our program, too. I entered happy, motivated, calm. By graduation I was on daily Zoloft, Klonopin, and Ativan for breakthrough panic attacks. One afternoon I was feeling brave and told three classmates: all three of them had also started psychiatric medication since starting the program. 4 out of 4 in my sample size.
5 years later I am still on a lower dose Klonopin.
On a *good* day I make dozens of life altering decisions that keep me up at night, see patients with complex symptoms who want a diagnosis on the spot, and get yelled at by patients for taking two hours to return a call about a rash they want diagnosed over the phone. No one ever says “well done!” You are not allowed to be anything less than perfect.
Last month I worked while having a miscarriage. You simply can’t cancel dozens of appointments. I hated my patients for keeping me from being home, crying with my husband. Of course, they had no idea, it’s an inhumane system.
Sarah, I think you are AMAZING! Thank you for giving so much to so many others. I really want you to care for yourself and not allow anyone to take advantage of your hardworking compassionate soul. You deserve to be appreciated and have your human rights respected. Come to our next retreat. I want to meet you. Call me anytime 541-345-2437. I promise I’ll call you back right away if I don’t answer. Please leave a message 🙂
Dr. Wible, I’m starstruck 🙂 Thank you for the kind words. As a new-ish provider with less training than a physician, I want to shout to the world “this job is really hard, and I’m scared I’m not good enough at it!”
Just today I was ruminating about a patient I thought I managed poorly. My instinct was to pour a drink and climb in bed, instead I channeled my inner Wible – I called an attending 30 years my senior to talk about feelings! I ended the conversation feeling confident in my skills, and able to the enjoy the night with my husband.
Nothing bad should happen when you break the taboo and talk about your feelings, odds are the other provider wants to, too.
You channeled your inner Wible! LOL :)) Keep the faith . . . <3
I’m a psychiatrist and ACT therapist HIGHLY concerned about this issue. “Who Cares In Sweden” is a superb documentary in 3 hour long parts exploring common adverse effects of SSRI’s, and why we are so often unaware of these. It features the best experts in the world on these matters, and presents the material in a highly engaging, sober and measured manner. In particular the effects of SSRIs (and stimulants aren’t dissimilar) on EMPATHY and JUDGMENT for / of others is HIGHLY concerning when it’s our physicians taking these medications.
I highly recommend Who Cares In Sweden to anyone taking these medications, prescribing them, or knowing anyone who is taking or prescribing SSRI’s. I’m very interested in your thoughts, Pamela
I understand that suicide rates are quite high for medical students and doctors. Obviously, the ridiculous expectations for students and residents contribute to this. But we also know that SSRI antidepressants can create or exacerbate suicidal feelings and intent. How much of the increase in suicidality can be attributed to the attempts to “treat” what is actually a normal human reaction to an abnormal, inhuman situation?
Probably most. You nailed it. Example: an SSRI was not the treatment for depression cause by my shitty marriage. Divorce was the ultimate solution. We are driving many bright compassionate people to suicide by tormenting them with human rights violations and inhuamne work environments within “health care.” Tragic beyond belief.
This is so powerful, Pamela! Thanks for doing the research and publishing it. I would hope for some kind of a more legitimized study, like an article published in a peer reviewed journal. Have you submitted there? Or a reference to the same in your article. Does it seem out of the ordinary to ask for this? And how about a study on therapists, counsellors, psychologists, and psychiatrists–one separate from the medical school? Thanks again, Pamela, for your pioneering work.
Oh yes! We do need more research and would love to get this into a peer-reviewed journal. Let me work on that when I get a moment of free time . . . . lol . . . I’ll try!!
Its intriguing and curious to me, warranting perhaps empirical exploration, that veterans, physicians, and those who are bereaved are both medicated at a significantly higher rate than the general population and that they are also more likely to commit suicide. This could well be the next tobacco scandal.
The human mind is the last frontier.
Everyone has an addition ,drug, drinking.food buy things you don’t need and keep going on!!doctorthat tell you how you you feel i no this for fact i went to hospital 4 times stayed i week or more still nothing wrong with me got new doctor thank you god saw him i less then a week he told me don’t get up set he had me go to hospital up around corner pulled in ER passed out (i dye right in front of ER doors)the Doctors that are good they fire them ,,,, i think i need layer to sue some them but florida only has 2 years to sue anyone for anything ,even though its been an on going thing from some problem
This is why it is essential to have a good primary care doctor who can oversee your health care. There are some great ones out there. Don’t lose hope.
Dear, Dr, Wible
I found your article, after one of the med students at LSU Medical school, in New Orleans mentioned these very appalling statists.
I have been with the wellness center for almost 10 years, presenting programs relating to mindfulness training & stress reduction, and I am happy to say that mindfulness techniques have recently gained popularity and support here at our university.
In my work, I follow the guide-lines and basic methodologies set fourth by Jon Kabat Zinn,Ph.D.
A committee was most recently formed on Mindfulness and a guest speaker brought in to bring everyone up to speed on the theories and application of an ancient and alternative way of understanding and creating tools of awareness to help better deal with stress, anxiety and depression. My programs are open to all student, staff and medical professionals… After launching these on going programs for little over a month,
I have many wonderful letters testifying to the wonderful benefits and outcomes of simple presentations and quiet insight meditations.
Thank you for your article and blog, Sincerely Rolf VanAnders, LSUHSC Wellness Center, New Orleans, LA: rvanan@lsuhsc.edu
Wonderful Rolf. I don’t doubt the benefits of mindfulness. However, mindfulness is not the solution for human rights violations, sleep deprivation, bullying, hazing, and sexual harassment. All of these abuses continue in our health system in medical schools and teaching hospitals around the country. Also, not sure mindfulness will help with the stimulant issue addressed in this article. Have you had success getting medical students off SSRIs and ADHD meds with mindfulness? Just curious . . .
Sad statistic, unfortunate and a national disgrace. I am just shocked.
After 10 years working as a psychiatric physician assistant, the state in which I held a medical license informed me that I was not competent to practice medicine because of bipolar disorder. Up until that time, my supervising physicians praised my work and gave me full autonomy in seeing patients. My license is indefinitely suspended. I don’t know if I want to go back to the career. I have been suicidal and had attempts. It wasn’t all the bipolar disorder alone. Much of my psychiatric symptoms were the result of the stressors of working in the medical profession and not being able to discuss mental health problems for fear of license suspension or revocation, which is exactly what happened to me.
The problem is that many young people feel pressured to become a doctor or otherwise they will be deemed as unsucessfull by their family or their surroundings. Young people feel the increasing pressure to get highest paying job in a middle of slow economical growth. Inflation rates are higher, mortgage is more difficult to get but salaries are plateauing. There are only few fields where you can make safe money (not self made) but safe jobs that can be guaranteed with a university graduation paper. One of the best and most luxurious ones is medical. For this reason young people are slithing each other’s throats and avoiding any sort of normal teenager-hood to be able to get in. For this reason, their coping skills are lacking as they never got the chance to have proper life experiences. Why do you think it is so hard to write a motivation letter? it is a common conversation between people applying to medical school about which traumatic experience they are planning to write. (Of course they have to have traumatic experince, because who has happy live right?) Medical schools make it seem like only students with detahs on the family, illnesses and other accidents you can come up with are acceptable. These people are so much more suspectible to be helpless and resort to drugs.
The problem is that the years when medical school was for people who were passionate about medicine is gone. Now you see people who never lived their life being pushed in a tough system where they are expected to know what they don’t know.
SAD But TRUE .
Dr Breggin has just posted your link.
Thank-you for what you do.
I thought it was just me.
Started on temazepam from ED as intern to sllep after long stressful shift with too much caffeine, got depressed and instead of eating and sleeping and taking a break to deal with complex adoption related issues (2 mothers), my friend referred me to her consultant and i ended up on a psyche drug roller coaster fro 1993 -2001 when I had a suicidal psychosis from effexor, and ended up on disabilty pension.
Since some of the adverse effects of antidepressant drugs is lack of empathy, aggressive and/or violent behavior, this is a very dangerous mix to have i.e. a MD license + lack of empathy and/or aggressive, violent behavior = a disastrous recipe for patient harm.
Empathy is wiped out when one is fighting for personal survival in a fear-driven teaching environment that pits our brilliant compassionate young doctors against one another.
Exactly. But instead of calling for transparency that might build broken trust between the system & the public, the call is to end the “witch hunt” and provide privacy that doesn’t exist for the public subjected to the same inherent discrimination created by “mental health” labels the system insists on using – even though they have been repeatedly been exposed as without scientific credibility. This is of course the state of affairs that most medicine functions under.
The “chemical imbalance myth” has long been exposed, even by high level members of the APA (inventors of the DSM) as something no credible dr would believe or repeat. Pies, explained it as a convenient allegory to coerce people into taking and remaining “compliant” in drugs widely documented & proven to be both ineffective and dangerous. In fact, access to “mental health” services and psych drugs is documented to increase suicide rates.
No one who is unfamiliar with these basic facts and issues that need to be litigated as Junk Science in a court of law, should be lecturing on them and spreading further disinformation.
When I shared your post, I got a response question asking for verification of your statistics. Where can I see the statistics that you’ve used in this article, 75%?
From interviewing 220 doctors as noted in the article. Further research required as the results of my interviews were shocking to say the least.
When I shared this article, someone posted an inquiry about where you got your statistics and how they can be verified. Can you share that? Can you tell us how you got the 75% statistic?
Hi Pamela how do you know that this is true? What you have offered here is anecdotal evidence. If true this would be very valuable information.
Based on a survey reported above and should be extremely valuable information for anyone concerned about the health of our trainees. As stated in the article more data is needed. Unbiased. As you know doctors and medical students would be unwilling to release the facts of their situation to any organization connected to their employments for fear of career repercussions. The fact that multiple sources (med students, residents, program psychologists) from various schools were reporting numbers in the 75% + range is shocking to me and deserved to be published (just as the nearly 1200 doctor suicides that have been submitted to me deserve to be published and investigated further). BTW: Outrageous levels of caffeine and other stimulant beverages OTC not even included here—-and there are additional health hazards from these Red-Bull-Starbucks cocktails TID.
What’s most disturbing is the willingness of medical profession to remain in denial about the extent of physician suicide crisis and widespread drug use (legal and illicit) among trainees, while harping on “burnout” and other victim-blaming terms and suggesting doctors just need to meditate, do yoga, “be more resilient” without addressing the underlying toxic culture and eradictaing human rights violations from medical training. I could go on . . .
Hope this helps. Happy to talk.
(St Louis U Med School Class of 1965)
–we started with a class of 112, 80 graduated the same day, 10 or so graduated a year late after repeating a year, and another 10 or so added to our class after repeating a year earlier. There wasn’t much drug use at that time, just hard work and fear of failure.
We ought to have liberty in medicine and let the field freely restructure.
Ever since, over a century ago, medical lobbyists commissioned the Flexner Report to use government coercion to restrict the medical field and increase physicians’ remuneration and prestige, medicine has become a racket —and one that is bad for the physicians as well as the patients.
I am a medical student, and while it is true that the prevalence of depression and use of psychiatric drugs is higher in medical students I do not think it is 75%.
According to one study 27% were depressed and 15% of those that were depressed sought treatment.
My class did an anonymous survey during a wellness lecture in the final year of medical school and found approximately 65% had experienced either depression or anxiety episodes during their training. Prevalence may not be as high, as many learn resilience and can bounce back but incidence rates of mental health disorders throughout medical school and residency are absurdly high. Some people cope better than others, or have healthier approaches to doing so. Some have better support systems. Many residents are chronically fatigued; mentally, physically, emotionally. And not the type of fatigue that you can remedy with a few good sleeps. The fatigue is binding.
Antidepressants are a class of drugs that reduce symptoms of depressive disorders by correcting chemical imbalances of neurotransmitters in the brain. Chemical imbalances may be responsible for changes in mood and behavior.
There are many meds available at online pharmacy stores for Antidepressants treatment mygenericpharmacy.com is the one that i know.
I hope one day that there will be test that that measure serotonin levels in one’s brain to show that there really is a chemical Imbalance in the brain if Rx is needed. I also hope that big Pharma will come up will a pill that will reverse the side effects or withdrawal symptoms of these harmful drugs! It’s so sad to see people suffer so bad behind the drugs. You would think with all the people who suffer, that more would be done to counteract their suffering.
Maybe we need to take our cues from the movies that we see: When a potion is created that causes havoc and destroys…Somehow there is always an antidote that reverses the damage that has been done.
Mmbs education system its self wrong we all lost our traditional food going towards medicine in India food it’s self medicine but now in India every thing is changed hybrid seeds pesticides chemicals change in life style then how can a man be healthy in body wise and mind wise
I agree the hazards of pollution, chemicals, pesticides, even pharmaceuticals in our water supply. We must get back to traditional low-impact lifestyle.
My Xanax addiction started innocently when I was probably about 22 — in the prime of my life, at the time. I found myself struggling with a bit of insomnia as I was in the process of applying to medical school and taking Adderall in the name of vocational success.
That’s how Xanax entered my life: upon an initial and cursory complaint of difficulty sleeping. Had I known this garbage would leave me grasping at the strings of my very existence, I’d have scoffed at the concept of ingesting even a single milligram. But I swallowed those first few pills quite eagerly, as I was exhausted, and nobody (including my prescribing physician) told me that my life would eventually be on the line as a result.
After two attempts at the MCAT, I was accepted to Albany Medical College, where I proceeded to pass all of my classes while simultaneously delving into an abyss of narcotics, all prescribed to me by my long-time general practitioner. Sleep became impossible as the stress was inexplicable but, as the Dean of AMC put it during one of our first introductions into the Masonic Cult, we could no longer compartmentalize ourselves and we’d simply have to adapt to swallowing information from a metaphorical fire hydrant as opposed to the “sippy cup” that was our premedical education.
After several all-nighters-in-a-row, I realized that my GP wasn’t providing me with quite enough pharmaceutical speed in comparison to my most successful, cracked-out classmates. So, I sought it out from a psychiatrist at my medical school, who told me that “At that point, everyone had adult ADHD” and not to worry. Whether this was true or not, I started easily speed-balling 50 mg of Adderall alongside 4 bars of non-generic Xanax every day, and somehow continued functioning.
Fast-forward to 2015 — after an “accidental overdose” on an almost-lethal cocktail of Xanax and Tramadol, which landed me in the ICU with Seratonin Syndrome for a week during New Years. Intubation and all, I’d voluntarily torn the skin away from half of my face by that point under the strong conviction that I had alien fibers in my dermis and there was a palm-sized bald-spot on the right side of my head. According to my dad, a nurse asked rather concernedly “Honey, were you in a fire?” and my response was “Long story.”
Within the deepest realms of my mind, I preserve the fragmented memories of my mother, father, and brother visiting me there, all of them crying and telling me how much I meant to them. At the time, it disgusted me and I experienced the situation as a bystander, unable to control my own reactions. I have one recollection of asking a guard at my door “Who ARE you?” after I’d apparently held an hour-long heart-to-heart with him just moments prior, and the fleeting memory of calling my mom from a bedside phone at 4AM to tell her that I planned on breaking all of her fingers.
Humiliation.
And then, the fallout from that — complete distrust from my family, on whom I called the police just a week prior with the claim that I was being kidnapped (just before being admitted to the ICU). I decided to leave medical school shortly afterwards, without so much as a “sayonara” to my lifelong dream of becoming a physician and not because I was failing academically but, as I put it in a final email to my Handlers, I simply could not “uphold the pressures of medical school without being an unhealthy person.” Isolated in my depression, I quickly lost all of my all-too-cool “best friends” from both home & college who told me, quite frankly, that I had become irrelevant. Maybe it was because I’d gained about sixty pounds after stopping Adderall cold-turkey, but likely it was because they were fake friends in the first place.
Regardless, enough was enough. I spent a year tapering my Xanax dose with the direction of a psychiatrist but not without a couple of ER visits here and there — either because my fingers were twitching out of my conscious control or because I felt that I was floating outside of my body during panic attacks so severe that I’d sometimes hold a knife to my wrist to recenter. In those sick and twisted moments, the thought of dying was calming, as a last resort to silence the infinite discomfort of my withdrawals.
Eventually, though, I emerged from my descent — with the help of Lexapro at 20 mg daily and lots of exercise including a half-marathon. My OCD vanished via daily behavioral exposure therapy and, after many nights of deep-breathing exercises, so did my insomnia. After dropping out of medical school, I tutored and was eventually hired by an engineering company, where I now make more money than most of my peers (including doctors from the medical school class that I should have graduated with).
The sad thing is that 400 female medical students and physicians commit suicide every year, but almost all of these deaths are due to “accidental overdose,” similar to the diagnosis on my own ICU discharge papers. This puts over one million American citizens out of healthcare every year. Because their doctors are dead.
Today, in 2019, I am thriving. I am married, just bought my dream house, and I am back within my own very beautiful body.
So take this as a very important PSA: you can leave, and you can thrive.
Please see the Twitter comments
@joannamoncrieff