A physician shares his suicide survival story with me. The 51 words that saved his life.
Hi Pamela, Here is the text that prevented my suicide:
“Hey I’m so sorry about your patient. That sucks. I’m very thankful that we have you as an excellent otolaryngologist to learn from. You take care of so many sick patients and do a marvelous job educating us how to do it safely, skillfully, and compassionately well. Thank you for that.”
It’s been a particularly hard year for me. But I’m surviving.
Thanks for all you do Pamela.
I shared his text as closing slide in my keynote last weekend on creating a culture of wellness among orthopaedic surgeons, anesthesiologists, and veterinarians. Concepts apply to all specialties and professions.
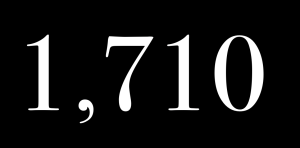
After interviewing male physicians who survived suicide attempts, I discovered the average time between their decision to die by suicide and the moment they grabbed their gun, pills, scalpel (or method of choice) was–3 to 5 minutes.
Average time it takes to type a text message—less than 1 minute.
Your best and fastest way to save a doctor’s life may be a text message.
* * *
If you need more proof of the lifesaving impact of your words, read this:
RIPPLE EFFECT: Never underestimate the power of your words to travel 8,158 miles to inspire a random woman 991 days later. I just got this email today—nearly 3 years later!
“Hello Pamela, On 3rd November 2017, I was seeing an orthopaedic back surgeon, Dr. Gary Speck in Australia (where I live). While taking my history he discovered my daughter would commence Medicine the following February (2018). Instantly he told me of an article he had read that very morning and said it was a must read for my daughter. He kindly printed a copy for me to take home. The article is: Loyola Commencement Speech ‘Live Your Dream.’ My daughter is about to commence her 3rd year of a 6 yr medical degree at the University of Adelaide here in Australia. She has been home for the holidays and she still has the article. I asked if I could read it and she said yes but I’m taking it with me. I want to thank you for this article. Gary gave it to us because he thought it important to share your message. While she is still 4 yrs from being an intern, I love that she values your advice and that you inspire her. Keep being the amazing woman, doctor, mentor you so obviously are. Love from a very grateful mum/mom downunder in Australia xxxx”












Good job, Pamela.
I am going to quote your work ( and your book about human rights violations which i just finished reading) in a forthcoming book which is being edited as I write this. Stay tuned!
I just received this message from a resident who has hesitated to share her support with colleagues. I hope to normalize kindness and humanity in medical training and beyond. Thank you for spreading the word through your writing,.
“I love this, Dr. Wible! As a pathology resident, especially when I’m on the autopsy service the thought has crossed my mind to email the resident who pronounced the death (especially if they’re interns) and say I’m sorry about their patient, but I never have because I thought it would be “weird.” But perhaps now it’s something I’ll start doing!”
I think that would be a great idea. I’m a nurse practitioner and I have had patients pass away unexpectedly it was a horrible feeling. It affected me so much I switched specialities. I feel like it’s no place in healthcare to really talk about this. You just have to pick up your stethoscope and get the bed ready for the next admission. But reaching out would be great ?. At least he or she would not feel alone and know that some one cares for their well-being.
Love this, thank you for all you are doing every single day, Pamela.
This sounds exactly like a text I received few years ago! Words actually mean a lot to someone who is suffering.
Sharing note from Twitter in response to this article:
Got thank u note from pt fam. Actually it was a long letter describing how I saved ‘s life,how I did not “give up on pt”, etc. What they dont know- they saved ME. I was able to continue doctoring?( I was NOT suicidal). Words matter. Life is precious.
I laff and weep at once! You are a glorious blessed soul, a shining light in a dark forest
like the hermit Virgo card in Smith/Waite tarot walking thru a dark forest at with lantern blazing unafraid of the dark of night.
Thank you Dr Pamela Wible. Though i am not a doctor, i am very grateful and thankful to you for the work you are doing.God will definitely bless you for that.
when i was following the suicide of Dr Deelshad Joomun i came across your article. So inspiring and helpful. Am a mauritian and i know her and her family. What a great loss for us.
Anyway, have a blessed day ahead
Thanks and regards
Reshma Bhugel
Ah Reshma – please know I am here for anyone who is suffering.
Deelshad is a treasure. I somehow still feel her presence.
Pamela
amen amen amen
Thank you, Dr Wible, for doing what YOU do.
Pamela: I don’t know if you heard, but USMLE announced this morning that the USMLE 1 will be changed from a numerical score to pass/fail beginning in January 2022. I believe this is going to be a very very big change in a good way for the pressure on medical students during the pre-clinical phase of medical education, which I think is the starting point for a lot of physician burnout and other psychological trauma. I am hopeful that the other steps will also follow. However, Step 1 has always been the most traumatic and where many students get stopped in their tracks, being forced to change residency choices and face disappointment and self-doubt due to the score. DB
That is fantastic!!!
Thanks for sharing.
Pamela
WOW!
A patient’s parent is the one who saved me.
Her words were simple: “How are you doing?”
She cared. And expressed it.
I really admire the work you’re doing, and hope to talk more after the 16th or so.
Best wishes,
How are you all addressing those physicians who harm patients frequently? What about those who have been found not to be physicians and have been granted rights to continue without any accountability?
The problem we are finding is that the trust has been tainted. With all of the hidden information and refusal to tell the truth about a harm or death make it very difficult for one to trust anyone in the medical community.
How do we address this?
I am addressing the root cause of the cycle of abuse in medical training and practice that wounds these compassionate humanitarian doctors who just wanted to help people but find themselves in hazardous working conditions without legal protection resulting in harm to themselves and to their patients. I address the common human rights violations in medicine and simple solutions here: Human Rights Violations in Medicine: A-to-Z Action Guide. I think you will find it horrifying and empowering at the same time. Simple solutions that give power to patients and doctors as allies (as we are so often both victims of the same system dysfunction).
Thank you and you are correct as it relates to the compassionate humanitarian doctors. How do we help with that?
Be compassionate with your doctors. Realize that we are all allies. Don’t hold us to superhuman standards. See this: https://www.idealmedicalcare.org/heart-wrenching-photo-of-doctor-crying-goes-viral-heres-why/
Anonymous comments from a physician:
“Hi Pamela, I want to thank you for all that you do and your caring towards physicians who have dealt with mental illness, trauma and may be suicidal. I was suicidal 2 months ago and almost reached for my pistol. thankfully my husband had taken away my ammunition. My depression medication has since been adjusted and I’m doing better. Honestly I don’t know whether I will stay being a doctor/psychiatrist as it’s very stressful but I have more hope than what I did. Your messages have helped me and have made me realize that I’m not alone. thank you!”
It is SO important that we reach out to one another for comfort & support!!
Pamela,
this is amazing. Saying Thank You and appreciating everyone can do so much – for anyone and everyone. As well as stepping up and taking responsibility when you see someone in crisis. Medical Professionals and First Responders are under so much stress, most people do not understand. They don’t appreciate what type of impact the stress has on someone or what the responder could gain from saying Thanks.
I actually have 2 examples where communication is Essential & Taking responsibility changed the outcome.
I have been an aspiring premed student for years. Money & circumstances about my life & health has currently prevented me from taking the plunge. In addition the lack of support for MD’s and premed students concerns me. I have a disability and did not know if I would be supported enough to complete my dream. I had been encouraged to go to medical school by 2 of my PCP’s. My IQ has been measured at 181 when younger. It was not a lack of ability that prevented me.
In December of 2017 I was in a tumultuous relationship where communication had gone south very very quickly. The man I was in love with declared to me that “He was Done”. I was totally and completely in love with him, and had trusted him completely, and this shocked me to the core. Yes, things were difficult- but I did not view it as unsalvageable. I thought an increase in communication would improve things, a discussion of boundaries and expectations, and of wants, needs, and desires in this relationship. I thought that could turn things around. Upon reflection maybe I was too attached to him, but at that point in my life he was my only stable support through a very difficult time.
When he stated he was done, panic and loss overwhelmed me. He had indicated he was choosing another woman instead of me. Him being polyamorous – I knew the other woman and about her and one other. He had been mostly honest so I thought. I had the other woman as a friend, a close one. She too was affected by a lack of communication with him, and her expectations had not been realized. She had cut him off, and out of her life in retaliation. He clearly wanted to mend things with her.
Me, being who I am, wished them well. I wasn’t thinking clearly being overwhelmed by life, and told him I would remove myself from the situation so that He and she could be Happy. I then went and while being completely overwhelmed and in turmoil reached for the pain medication I had been on for years and proceeded to consume over a bottle and a half of Kadian 80mg sustained release – prescribed at BID dosing. One month was prescribed at a time, yet I spaced it out as far apart as I could when I felt better, so I had accumulated a small stash. I unthinkingly took it – not wanting to be in pain anymore. I had been in physical pain for over a decade. Excruciating pain barely controlled. The emotional pain was too much. I wanted to end it.
I told him. I took a picture of the bottle as I wished him well & said goodbye, something I never said. Ever. I then proceeded to take a full bottle of Glucophage XR 500 mg bid – a 3 month supply. I am a pharmacy technician and figured it would speed the process dropping my blood sugar enough to put me unconscious so I didn’t suffer when I started to suffocate.
He told me to not do it. Said I couldn’t. I proceeded anyways, and after a few minutes he said he had other things to deal with. Later I found out he had asked the woman he had chosen to check on me, and she instead went to bed and ignored his request until the next day – evening.
Myself – recognizing what was coming, chose a few key people and messaged them good bye. Again, I never say this. I always say talk to you later.
One exceptional young woman and friend noticed the word change immediately and asked what was going on. I sent her a picture of the empty bottles and said I wished her well & hoped she would be happy, and that I was sorry I would not see it.
She responded immediately & reached out. Told me to call 911. I refused. I was alone and resolute. Only 10 minutes had passed from being told He was done and all of the above. She went above & beyond – taking action and responsibility for my safety and care. I had sent her a care package a couple of weeks earlier to help her out. She lived in Georgia, I lived in Massachusetts. She called the local Emergency Services and got me help. When they arrived, all 4 of them, they said she had sent help. I willingly went to the hospital with them.
I must be clear here. My decision to die – to remove myself for their happiness was made in an instant. I had become resolute and had acted immediately. I had been suicidal in the past a couple of times, but I had NEVER acted before and had ALWAYS sought help, getting myself seen and checked into a hospital or other program for care and evaluation. This time – I was not seeking treatment. I only survived because of the young woman living in Georgia who had acted to ensure someone came to my door to check on me.
Much is a blur – except for knowing that after some observation the hospital tried to release me to get evaluated. Told me to get dressed. I had been laying there awhile so I attempted to get up and get dressed. I collapsed on the floor and couldn’t move. I got yelled at several times. The man said / yelled – while I a woman in nothing more than a dressing gown on the floor in hysterics with a history of rape and abuse, not knowing why I couldn’t move my body, “What are you doing?!!! Get up! Get dressed! You are going to be evaluated!!” I sobbed hysterically. Soon I was roughly picked up, thrown on the stretcher again. An IV was started, which I could not feel. I was aware of being poked several times, but could not respond, and it no longer hurt.
They continued to evaluate me, and I deteriorated slipping in and out of blackness. Sometime later I was brought into a trauma room and Narcan was administered. I started screaming it was so painful. I was vomiting continuously for what felt like forever. Then I started hallucinating I thought. I was in a blue hallway full of light. It was so peaceful & I no longer felt any pain. None at all. I saw many flashes of light – looking like shooting stars, pass me by as I stood there, gazing at the lights in the distance. I was aware those were souls who were passing on. The peace and love I felt were complete. I was no longer afraid and knew things would work out. It was indicated to me it was not my time and I had a lot of work remaining on earth.
Next thing I knew I was back in my body and filled with agony again. I had never hurt so much in my life. A nurse asked me if I was ever going to do this again. I replied vehemently I would not. I promised myself to never go through this again willingly. I would preserve my life. She scoffed and said “That’s what they all say.”
Later I was dehumanized. Talked about as an “It”. I was talked about in the third person as if I was no longer in the room. Someone asked the nurse if I could see. The nurse said, Directed to me, “it needs to open it’s eyes”. I struggled and complied, barely able to do so. Blackness ensued.
Sometime later I woke up in a recovery bay, oxygen in my nose, an IV in my arm, and heard I had barely made it and they had to resuscitate me. I hurt. I believed it. I was in recovery for 3 days. I am gluten free. They struggled to get me food I could eat. Pain was not an issue until the 3rd day. I then expressed discomfort and pain and they got me a Percocet and ibuprofen. That was it – after 80mg of Kadian twice daily for years. I understood but was in agony while in the psych unit for weeks. They would not adjust any of my pain meds despite anxiety and inability to sleep because of pain. I got up constantly and wandered the halls in the middle of the night I hurt so much. Anti-anxiety meds sent me through the roof with anxiety, even Benadryl agitating me. I took my meds on time precisely to try to achieve maximum pain control. I showered several times a day – trying to use heat to soothe the pain and aches until I got yelled at and told I could not do it anymore. Sometimes the showers had been the only thing allowing me to get through to the next dose of ibuprofen or Percocet. I was miserable. No one understood or cared to understand on how much I hurt – except one nurse who had fibromyalgia as well. I also had severe back pain, and sciatica, and several other issues.
This nurse tried getting me a weighted blanket she used, to try to comfort me. My skin became severely aggravated and I developed a rash. She had been washing it in regular detergent. I was sensitive to fragrances. I soon could not even tolerate my bed sheets and blankets. I was itching incessantly and my skin was burning. Luckily the only local friend I had brought me my fragrance free detergent and some clothes. Soon, after washing everything – even the hospital sheets and blankets in that – soothed my skin, with hydrocortisone cream 2%.
The weighted blanket couldn’t be used though because she wouldn’t use my detergent. Pain continued.
After severe and several counseling sessions and talking to my PCP it was determined I could never use Kadian again, the risk was too great. I understood and complied despite being in agony. I expressed several times wanting my pain regimen fixed and they refused. Only once I got an untreatable migraine while admitted did they administer Fioricet, and that allowed my pain cycle – all of it to break. I finally could sleep and rest. They wanted to adjust my meds, I refused. I had a huge Lack of trust since they were not listening to me and responding to what I was saying. Plus it was lithium. I knew as a pharmacy technician that I was severely sensitive to meds and regular blood work would need to be administered to ensure the dosing was correct. They were not listening to me, so I was fearful of going toxic despite telling them how I felt. So I refused. Trust had been broken several times by them not adjusting my pain meds, and before that by the man I loved. I was not trusting easily.
I got released on my old meds, and to my PCP. My MD could not see me for several days (10). They wanted to release me with a script of Percocet saying 1 tablet every 6 hours for 10 days with a quantity of #12. As a pharmacy technician I looked at that and said “seriously! Are you trying to get me back into crisis? The script will not carry me through to see my MD, especially when I can barely move while taking maximum dose of Percocet and ibuprofen now!” They brought the conundrum to the discharging MD. It took over 6 hours for them to decide to rewrite the prescription.
The second incident was a couple of weeks ago.
I was attending a Science Fiction Convention I volunteer at regularly and annually for the past 8 years. I am actually considered staff on the convention because I volunteer so many hours a year. Over 150 hours a year.
I am the Assistant Dealer Liaison for the Dealer’s Room for the convention. This is where the participants buy their souvenirs for the annual convention. I had been given increasing responsibility over the past 5 years I had been in this position. I had the respect of several senior staff, dealers and participants. During the 5 day event I would work tirelessly to ensure it ran smoothly, sometimes putting in over 80 hours in that 5 day weekend. I was on call during closed hours in case of an emergency. During the years I also got up and checked on the room during the night to ensure security was doing it’s job and had several times found them lax. I had actually been able to enter the Dealer’s Room area, unobserved and unchallenged where millions of dollars of merchandise was displayed openly. That was unacceptable. I communicated with the head of our area of security to fix things. In addition I made several rounds during the day – checking in with dealers to see if I could address various issues that popped up during the day. They are usually quite busy with customers, and cannot always send a minion- aka employees for help or to run messages they are so busy. So I made myself available. It increased communication, happiness of vendors, made small crisis disappear if I could handle it quickly. I had after the first year of volunteering been given Autonomous decision making because my judgement was fair, accurate, reasonable and just. I got things handled quickly and avoided crisis. From a bee being found in a dealer’s merchandise and inventory in the middle of the winter when the vendor was from New York, to trash needing to be removed, room temperature adjusted, water stations filled, dressing rooms needing to be fixed and adjusted so customers could try on outfits prior to final purchase, to even assisting dealers who needed food and could not get away from their table to get any, and were about to collapse. I handled it all professionally and smoothly, reporting everything to my superior including what had occurred, actions taken, and resolution.
In addition I was responsible for opening and closing the room, and ensuring it was secure. I handled hotel staff and security issues – issues that arise yearly due to a lack of communication. I got my superior for assistance when necessary to resolve these issues. I also held the dealer’s accountable when they broke their contract, leaving early without communicating why, making the dealers room look empty in the middle of the convention. This would affect and effect all other Dealer’s sales since if a customer sees an empty spot they may assume we are closing and therefore stop shopping.
I was repeatedly assured my judgement was sound. I also coordinated volunteers in how they could work in the room, and signed off on their paperwork to indicate acknowledgement of them working. I took responsibility to ensure that they didn’t over extend themselves and took care of their needs.
This year though I overextended and a medical crisis ensued. I was a bit stressed, and things felt out of my control. I had worked a 12 hour shift on Thursday to get things ready for the convention opening Friday, in particular the Dealer’s room at 5pm Friday.
I was tired and irritated and in a huge amount of physical pain Thursday evening. At midnight things were not resolved regarding finishing securing the room, despite my supervisor being present. It was past midnight, the latest it had ever been in previous years had been midnight. My supervisor / superior indicated they would finish things up for me since It was taking so long, unreasonably long both he and I felt. I almost never take him up on that. Every other year I had stayed when it was offered due to my sense of responsibility. I had felt under appreciated during the day, overwhelmed, discouraged, and frustrated. Nothing seemed to be running smoothly this year, despite all my efforts. Even volunteers I had had no issue with previously were giving me flack and issues.
I agreed and went to bed, resolute the next day would be better. I took 1 additional Percocet 5/325mg over my usual 1 tablet. It was ok’d by my PCP that I could do this in occasion. I had very rarely used this and as long as I informed her the next time the office was open it was allowed. I figured I would call her in the morning – approximately 8 hours, to tell her. I had last taken 1 extra tablet Several months previously and not had an issue. Trust had been re-established and she was confident I was safe and using my medications effectively and safely. In fact she had just agreed to allow a 1 month supply of Percocet instead of a 10 day supply that I had been getting filled regularly since my discharge in December 2017. Due to an increase in sciatica pain in April of 2019 I had also been put on morphine 15mg bid in addition to the Percocet. I only took the Percocet as necessary, but was usually taking 1 tablet every 6 hours the pain was so severe. It was the maximum they would prescribe yet only succeeded in getting me out of bed for 3 hours intermittently during the day, the pain was so severe. I was determined to fulfill my obligations to Arisia through sheer will power if necessary and would recover afterwards I felt.
After realizing that I could not control everything or everyone that night, in defeat I said “I give up. I can not control everything and anything. People have free will and I must respect that”. That was at 1am Friday morning.
I awoke 3 hours later in blackness In My hotel room. I remember feeling I felt strange, off. I noticed my left eye would not focus, and had increased pressure in it. My right back head (I believe occipital lobe) hurt like hell. I was a bit disoriented. I lay there for a while trying to figure out my next steps. I realized I had to use the restroom. I struggled to get up, Went to the restroom and decided to look in the mirror to see if I could figure out what was wrong with my left eye. I immediately noticed my pupils were fixed and pinpoint. Not responding to light at all. I was concerned and went back and laid down to try to look up online what was going on. Slowly the awareness came over me I was not thinking clearly. I reached out via text ( not wanting to bother my roommates and looking back clearly not thinking logically or clearly) to 3 friends. One was the head of security for the convention this year. Bobby and I had a good relationship from his time as head of the dealer’s room in security. We had worked together closely and resolved many issues, some of them with innovative solutions. We trusted each other’s professional judgement, and had started asking each other’s opinions on personal issues. He is highly responsible and highly accountable for his own actions and has very high reasonable standards. If rules aren’t followed, and you pay attention – it is easy to satisfy him.
He responded to my text concerned. He urged me to call 911 if I felt necessary. As I decocompensated rapidly I followed his advice and called 911 for assistance. I soon woke up my roommates with my call to 911, and I soon couldn’t communicate any more so they took over the call. Bobby – the convention’s security division head had contacted the hotel to tell them I had called an ambulance and to coordinate getting the ambulance to my hotel room.
I feel his quick actions and attention to details, responsibility, and commitment to service saved my life. I soon was no longer feeling my body, was an observer at best, and only able to respond to precise questions with one or two word answers. I was very aware of being nestled in the hands of creation and that my life depended upon the free will and actions of those caring for me. I was at peace, and aware I was only holding on due to my sense of responsibility and love for those remaining. My connection grew very thin and dim at times. I could not move my body, or respond to painful stimulus. No call bell had been given to me while I was in trauma room 8, not that I could move to use it if I wanted.
Bobby felt responsible for my outcome. He was over stressed overwhelmed and highly concerned. It got to a point he didn’t even want to see me or speak to me during the rest of the convention. In trying to respect his space and wishes I complied. I wanted to thank him. He had saved my life I felt by his quick thinking. The other 2 people I had tried to contact – only 1 had replied, and the other naught. The one who replied – a nurse friend in Utah, responded hours after the event encouraging I go to the emergency room.
I had several issues during the Convention. I ended back at the ER being admitted for the third time in 2 days. I stayed at the convention among friends, relieved of official capacity and duties so I could care for myself. I did not think it wise to go home so soon after a health crisis to where I would be alone and isolated for the weekend and week.
I urged convention staff, through a Thank You letter to the convention – and Bobby the same time, to recognize him for his service, quick action, timely response, and caring for others to recognize him as a Hero. I want to thank him personally, but wish to respect his space.
He needs and needed care and attention also because he almost lost a friend, and a convention member while he was responsible for the security of the entire event. I know he was feeling stressed and responsible. I am highly thankful for him & his quick thinking and actions, while he was respectful of my autonomy.
He truly is a HERO and deserves recognition.
As do also all the hero’s in the various fields of service.
Feel free to share my story.
“I must be clear here. My decision to die – to remove myself for their happiness was made in an instant.”
impulsivity in these emotional decisions can go either way. A kind gesture can save a life in an instant. I think we all must understand how much a little love and care can go in saving the lives of those who need just a little compassion and understanding.
Thank you for sharing your story.
You are most welcome.
Again I must stress I would not have survived except for the heroic actions of the 2 people that went above and beyond. They both recognized my crisis, and took responsibility for my life and acting to save it.
That is not something seen very often in today’s society.
In fact I must even point out that the man who I loved while overwhelmed had asked someone he trusted and cared about to check in on me and help me. That person – who I had thought a friend, instead put it off and went to bed. I did end up hearing from her – after I was admitted to the hospital and had been resuscitated. Her lack of action could have resulted in my death if the young woman in Georgia had not recognized my distress and acted. Heroically I might add.
Hi Pamela. I’m a psychologist doing suicide prevention work with medical schools. I recently read your post about how a text message can save a life, and wanted to reach out to you about a text-messaging system I created, which a number of medical schools are using now. The system, Early Alert, uses text messaging to check in with students every week, and connect them with support resources if they need help
I’m so impressed with your text system!
Of course, personal texts are best though
having a system like yours is a great service
to busy med students and docs.
~ Pamela
I have been in the position of almost committing suicide. Between you, good friends, patients, and family I was able to make it through the darkness.
I am the only physician in my community who has not presented a “Friday conference”. Somehow i got out of it. Despite having a theater background I never felt good enough to present (as a family physician.).
Right now however I feel very strongly about presenting something related to physician depression and suicide. We have had a physician suicide in our small community of 25K (and it was another thing that got my attention). I am just trying to think of how to present this topic. I never felt supported by most of my community. There were several folks who were good support though others not so much. I really want people to know that what they say and do makes a difference when another physician is struggling. I am hoping they can be more aware.
We have a “Fall Clinics” where we have big presenters come. I wonder if any of your videos might be helpful. I have made a change in my practice to DPC but still believe i need to be doing something more to change the landscape regarding physician health. Any thoughts?
Thanks so much!
Happy to help and if you want to link to any of my videos or writing just let me know.
Thanks Dr Pamela Wible for sharing the post
I took my own advice yesterday and sent a nurse an email thanking her for her crystal-clear documentation of the events surrounding a patient’s death. She had the whole timeline documented, including the calls to the medical examiner, the investigator she’d talked to, and the ME case number, which was a HUGE help because we had to touch base with the ME regarding the death certificate and autopsy. This morning she wrote back and said thank you and that she really needed that email after everything that had happened with her patient.
So yeah, I’ll be doing that again in the future! 🙂
This is a fantastic resource and solution for Physicians, Trainees and Students. As a student another helpful resource I have witnessed residence utilize in the program I have had the pleasure of working in as a student assistant is a buddy system check in program. Residents are assigned “buddies” which may include senior residents and Chiefs via e-communication. This is best supported when group trust and respect for each other is upheld. Similar to the text message support system. Another solution that may be available is confidential counseling/therapy services, unreportable to programs, although my hope is in the future programs will prioritize providing counseling, therapy and mental health services to their trainees; outside of the “we have mindfulness therapy” offers. While this is a great step forward, we also need to find ways to integrate holistic support for our Providers. In addition, studies have shown nations that have removed their Tort system have had better outcomes and overall job satisfaction among their Physicians. Should we gain universal health coverage in the future my hope is such programming may follow. I also think gaining leadership within residency programs and medical schools that promote health and wellness among trainees and support physician advocacy and political involvement in such issues is vital to the progression and positive change in the field to be attainable and achieved. For those of us in the USA it would also be helpful to have changes in the education system, in terms of cost of education, student loans, the amount of pre-reqs that are nessecary vs. unnessecary (ex- time, money), and an increased push towards integrating measures to promote more socioeconomic and overall diversity/representation within the medical schools. Making strides as a community to encourage changes in Congress to promote such changes as well as increase the pay and seats available for trainees is also important.