Sometimes there are no words.
Not even a eulogy.
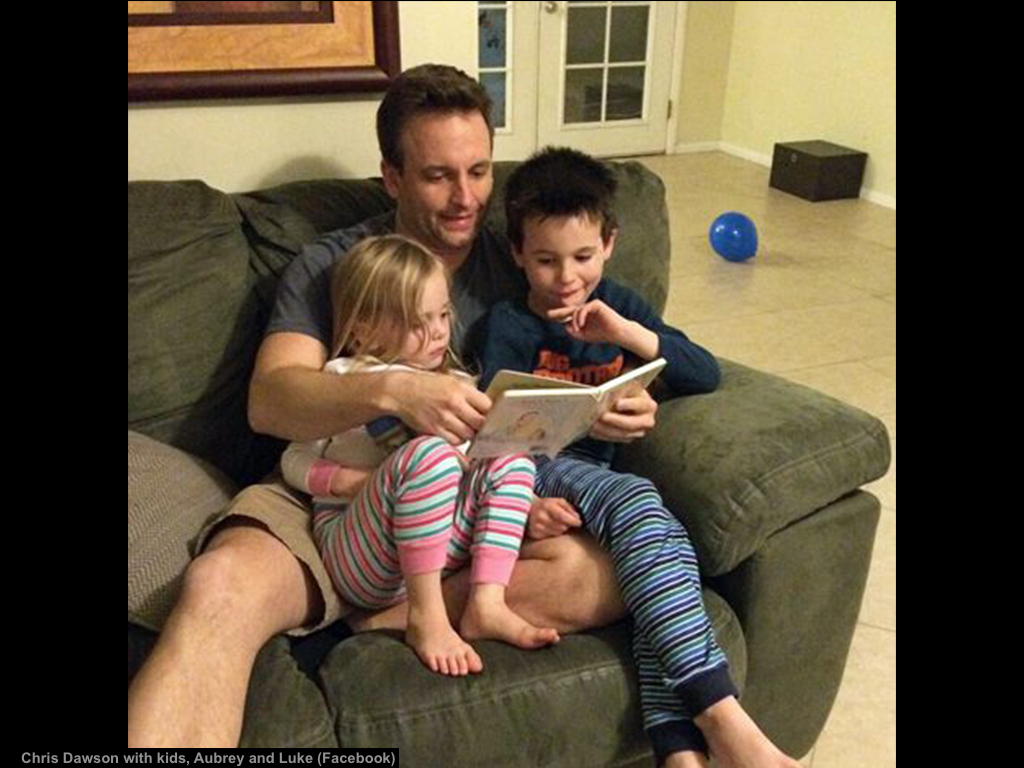
Then one courageous family writes this obituary. [This obituary was written by Rachel Dawson, his wife, with the blessing of his parents] In it they share how their son lost his battle with severe depression. How he adored his children. How he sacrificed fun, free time, and relaxation to receive his medical degree. How he took on the challenge of surgical residency. How he was so very damaged by his untreated anxiety, long work hours, and intense stress. How he attempted to self-medicate his hurt. How despite being an intelligent surgeon and a loving father, he did the unimaginable.
I first heard of Dr. Chris Dawson just hours after his suicide in a Facebook private message:
“My friend who is also a doctor’s wife is going through a nightmare at this very moment. Her husband graduated residency this summer along with my husband and he killed his two small kids and himself this morning. Her husband suffered from depression due to the difficulty of residency season and never recovered from it. I know residency is hard, I always said it’s a real b#%^*, but if you know your partner is having a rough time, suffers from mental illness or is going through a depression get him some help. At all cost! My heart is broken for my friend who no longer has her babies. This med journey can be very hard and can take you through a darkness if you don’t get the help needed. It was so close to home that I had to share. Mental illness is nothing to be ashamed of.”
I’m a doctor, a problem solver. I study human suffering so I can help people. That’s my job.
In 2012, I became alarmed by how many doctors were dying by suicide. So I started counting dead doctors. I began with a list of 10. Today I have 699.
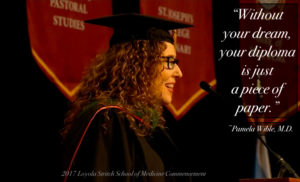
Now I run a suicide hotline for doctors.
During the last 5 years, I’ve spoken to thousands of suicidal doctors; interviewed surviving physicians, families, and friends; and published a book of their suicide letters, I’ve spent nearly every waking moment since 2012 on a personal quest for the truth of why we lose so many doctors to suicide. Here’s what I’ve discovered.
Of the 699 doctor suicides I’ve compiled, only 2% (15) involve a homicide. Half of those (7) are male physicians who killed a female spouse/girlfriend (all in health care—4 nurses, a nursing student, pharmacy tech, and dentist). Three male physicians killed their young children. Another strangled his disabled adult daughter before killing himself. Less than 1% of all doctor suicides involve homicide of their children. Of the 3 cases involving young children, all suicide victims were having marital/relationship problems with the mother. One also killed the mother.
Why would a doctor dedicated to saving lives take his own? And the lives of his loved ones?
Many doctors write suicide notes explaining their motives. A few leave extensive documentation—even videos (often they are whistleblowers exposing fraudulent hospital systems). Still questions remain.
Motives for murders perpetrated by doctors often involve ending perceived suffering of others. Four of the 15 physicians were attempting to end distress in dependent family members prior to taking their own lives. They wanted to protect siblings from an abusive parent; to stop an aging mother’s misery; to prevent institutionalization of a severely disabled adult daughter for whom the physician was full-time caregiver; to end the suffering of a child tormented with the same anxiety disorder as the dad. None of these four physicians seem to have been acting with malicious intent when they took the lives of others before killing themselves.
So how do we respond as a society to these suicides? Often with an outpouring of love for the surviving family amid condemnation of the suicide victim mixed with lots of confusion.
And then comes silence.
Until it happens again. In the house next door. The one with the Christmas lights and candy canes. And the soccer ball in the yard.
Our collective rage resurfaces. We pray for the family to find peace. Then the story falls to the bottom of the news cycle.
Until it happens again.
And again.
‘Round and ’round and ’round we go.
I’ve read hundreds of doctor suicide obituaries. One common theme: euphemisms obscure the cause of death and prevent discovery of answers we so desperately seek.
Secrecy, shame, and silence are 100% ineffective as problem-solving strategies. They also prevent us from healing.
Full disclosure: I do not know Chris Dawson, but I feel like I do. Maybe it’s because I grew up in Dallas down the street from where he died. Maybe it’s because we both graduated from medical school in Texas and completed our residencies in Arizona. More likely it’s because we both fell into a suicidal depression at age 36. Since he can’t share his story, I’ll share mine.
From October 22 through December 7, 2004, I couldn’t get out of bed. For 6 weeks. I wanted to die. I prayed that I’d go peacefully in my sleep. Despite my pleas with God and the universe, I woke up each day horrified that I was still breathing. I could not figure out how to release myself from my unbearable pain. I was fed up with being forced to practice assembly-line medicine like a factory worker. I had just been let go from a job (contract nonrenewal “not a good fit”). I could not face one more day. My bills were piling up. My marriage was on the rocks. I felt like I was in a suicidal coma. If I had a loaded shotgun, I may have pulled the trigger too—and this story would be mine.
The fact is we all have a breaking point—a threshold over which we would consider killing ourselves. And even our loved ones (in our disordered thinking) as a mercy killing.
So what shall we do now?
Here are 5 ways we can prevent the next physician suicide
1) Increase awareness of our physician suicide crisis. Be alert to mental health risks of medical training and practice, including high-risk specialties for suicide. We can’t solve a problem nobody knows exists. Talk about it. See the forthcoming film, Do No Harm. View trailer here. To arrange a screening at your medical school, hospital, or conference, email info@donoharmfilm.com.
2) Avoid a medical career if you have pre-existing anxiety or depression. Medical training will worsen your mental health—and may be life-threatening to those who are not resourced to cope with chronic high pressure and ongoing exposure to suffering and death. In fact, 75% of med students are on psych drugs just to survive med school.
3) Allow access to nonpunitive mental health care. Physicians have unique occupationally induced mental health needs and currently risk punishment for help-seeking by state medical boards, hospitals, and insurance companies that may prevent a doctor from practicing medicine. If you are suffering, I’m available to speak with you and I can refer you to confidential care by phone or Skype 24/7. If you are in imminent danger please call 911.
4) Allow access to nonpunitive marital counseling. A physician friend had her state license delayed for 6 months because the medical board demanded to review her marriage counseling records because she was depressed during a divorce. Doesn’t everyone need help during a divorce? Why should physicians fear seeking counseling for their marriage? (Note: a lot of physician relationships fail because there’s no time to spend with your spouse when working 100+ hours per week!). One request: Please support Rachel Dawson who has lost her entire family.
5) Humanize medical training. Residency is brutal with chronic sleep deprivation and human rights violations (plus lack of legal protection). Surgeons used to brag about 100% divorce rates! (as if toughing you up and destroying your family would make you a better doctor). Let physician trainees sleep, eat, and see their loved ones. Doctors are human.
Doctors are extremely gifted, complex individuals. Most people attracted to medicine have brilliant minds and are able to tackle immense complexity. Yet the culmination of such intense personal and professional pressure contributed to this surgeon’s complexity becoming confusion and such horrific torture that he just had to end it all.
So how do we preserve our humanity? That was the one thing Chris was unable to do at that moment—preserve his humanity. He most assuredly loved his children and as a surgeon saved many lives. Though he saved lives, he may have been unable to feel fulfillment. Medicine conditions physicians to be withdrawn and professionally distant. For somebody like Chris who suffers with anxiety to be groomed for emotional distance and discouraged from seeking help is deadly.
We are all born into this world with our own eccentricities, quirkiness, and a certain predisposition to anxiety and depression. Nobody is immune.
Did Chris have pre-existing anxiety before medical school? Seems so. If he were a realtor or an auto mechanic would he have been able to access confidential nonpunitive care for his anxiety? Yes. Would he have been more resourced to assist his children with anxiety? Yes. Would he have had more time to spend with his wife and invest in his marriage had he not been a surgeon? Yes. Would he and his children be alive now? I think they would.
My hope is that this honest obituary allows us to begin an honest (and long overdue) conversation about mental health.
Because our silence nearly guarantees our suffering will continue.











I read this week that veterinarians have a much higher suicide rate than MD’s and Dentists combined. Can this be true?
I believe none of the data we are collecting is 100% accurate because it has been shielded in secrecy for so very long. There are many doc suicides (and vets too I’m sure) that are deemed “accidental” overdoses and “accidental” car accidents etc . . . that are really suicides. More on how these suicides have been hidden from us all here.
Yes veterinarians have a high suicide rate. According to a 2015 study the rate is 3x the national average and 1 in 6 veterinarians has considered suicide. The factors contributing to those numbers are similar to what physicians are facing: long work hours, demanding internships and residencies (I worked 100+ hours per week and was on call the remainder of the time for multiple months of my internship), demanding clients, compassion fatigue, etc. Personality types drawn to veterinary practice are similar to physicians as well (highly intelligent, driven, empathetic, not accepting of failure) and have the same blockades to getting help. We all need to raise awareness of mental illness and that it is nothing to be ashamed of. Removing the stigma hopefully allows individuals to talk more openly about the challenges they are facing, but those barriers regarding insurance still exist. I don’t have any answers but hopefully talking about these issues is a start.
Thank you so much for sharing the facts. I’m certain we can cross-pollinate with solutions.
Yes, we Veterinarians have a very high suicide rate. I am glad that a light has been shed on this recently because we are beginning to form groups to help each other.
In contemplating the few suicidal weekends I had after my life was turned upside down by betrayal and divorce I realized in Veterinarian Medicine when we are faced with patients who are suffering & there is “no hope,” we help end their suffering with euthanasia. So… it isn’t such a big stretch when we are going through a very stressful life event and feel life will never get better to decide death is a perfectly reasonable solution.
In Emergency Medicine we might euthanize up to 10 patients during a long shift, especially during the holidays.
We are now working on this issue as a group.
And, I plan to reach out to my daughter who is doing a fellowship in a human Pediatric field this week to let her know she can reach out to me ANY time if things get rough. We are losing way too many great people from both areas of Medicine!
Marianne your insight is profound. Thank you.
Thank you so much for posting this. I am Chris’s aunt and what you have posted is so very true.
Oh Dena, so very sorry for the pain & grief. I do hope in some way that my words will help in healing others. Please do share with your family how much their honesty means to me—and to so many others who are reading the obituary. Takes courage to share the truth. By the way, I would love to invite you to join our Facebook support group for survivors of doctors suicide (family members who have lost loved ones in medical school or beyond). Here’s how to request to join us: https://www.facebook.com/groups/881571115309068/ (I do need to know names of who want to join so that I can admin approve them).
I would like to join. Rachel is my niece.
I just added you to the group. I can also put you on our mailing list for retreats and we have 3 conference calls (I can send you links to listen to them). I’ll email you now. Let your family know we have so much love & support to share with them and quite a lot of wisdom on the doctor suicide topic.
I am sorry for your loss.
Gina Anderson DO
Hi Pamela, I just read your email about the latest tragedy and I emailed you back about Bella, My co resident who committed suicide in 1992. I just wanted to say that I am glad I went into medicine because I found the perfect niche for my talents. I am a hospice physician and very happy doing it. (I think I do a good job because my patients and their families and Hospice nurses ect love me.) I suffered from some depressions before going to medical school but I made it through and my understanding of what it is to truly suffer, secondary to severe depression, makes me a better physician and uniquely suited to hospice medine. So I would not say “do not go into medicine if you have had depression”. I think you should just understand the risks of going into such an all consuming profession when you are biological primed to under go depression; Including the risk of death. For someone to tell me I could not be a doctor because I had a history of depression would of been devastating for me. I am so glad I persevered and went through it all because I would not trade anything for what I do now. I love being able to love on my hospice patients and take such good loving care of them.
I’ll add Bella to my registry (#700) & so very sorry that you lost your co-resident to suicide. Talking about this suicide crisis among doctors is the first step to healing. I also had pre-existing anxiety before medical school (mostly because I am a very sensitive loving person in a world that has way too much pain and I am an existential thinker so I am always thinking way too much mostly about solving problems that are way too big to be thinking about for one person so I can really sort of spin my wheels).
What I am suggesting is that we have INFORMED CONSENT. That people know the risks of a medical education to their mental health so they can make a decision to pursue medicine or not. I’ve been on the phone with premed students and others in high school who have already had multiple suicide attempts. Do I recommend they go into medicine? NO!!!! With support that you can survive medicine with some mental health disorders (but not on your own and without treatment). I’ve spent more on therapy to recover from the mental health effects of my medical education than I spent on tuition.
Do I regret being a physician? No.
Did I almost lose my life to this profession? Yes.
I wish I would have known what I was really getting into. And both my parents are doctors so you’d think they would have warned me. They did advise against going to medical school but never, never, ever mentioned the mental health impacts of medical training. So taboo and held in such secrecy that my parents did not even have words to describe the trauma of what I was about to endure.
I think this medical student nails it when she describes being less stressed in Afghanistan.
This issue jumped out at me too. I didn’t know about my anxiety/depression before med school. It was brought out in residency. Was it always there? Perhaps. But when you’re in the thick of training, on the train that can’t stop, it’s hard to have time to reflect and do self care. Even just 3 years of that can really do a number on your mental and physical health, your self esteem and your happiness. HAD I had severe symptoms before jumping on the train, I think I would have never boarded.
Curious how you would know not to board the train. Were you aware of what was to come? Because I was totally blindsided. I didn’t know what was happening until I was already getting my soul slaughtered. That is EXACTLY what it felt like in medical school. Like my soul was being pulled out of my body. I cried so much in my first year of med school my eyes literally were sealed shut one morning and I couldn’t see!
Add my friend Dan, from residency. He was an intern 15 years ago who killed himself by motor vehicle crash. Left a note, but it seems only his fellow residents and family admitted that.
Separately, I will try to call you to see if you are aware of suicides among physicians who have lost or are in the process of losing their licenses. I was suicidal when I lost mine due to sex with a patient (a commercial sex worker who took advantage of me as much as I her). I have an addictive disease, was misdiagnosed by my psychiatrist, and have additional mental health diagnoses. Medicine shoots its wounded, and covers up the bodies in the interest of “protecting the public”, the very public which is hurt by the loss of yet another healing provider who can truly identify with and help suffering patients. The suicide issue is another terminal aspect of this medical system wide sickness.
A great percentage of physician suicides can be correlated to malpractice proceedings. In order to fully understand parameters that may be influencing our decisions, I would recommend checking out the book “The Unquiet Dead” by Dr. Edith Fiore. When it is hard to categorize a specific treatment (especially in criminal activities) we must search out additional unforeseen explanations/influences.
Interestingly active malpractice cases are involved in a minority of these 699 cases. It was once thought that litigation was a major cause It is not.
I outline many of the causes here: https://www.idealmedicalcare.org/blog/ive-learned-547-doctor-suicides/
I also must allude to the fact that enzymes and hormonal influences also can exacerbate depression which if left unchecked can lead to suicidal tendencies. Especially prevalent in residency conditions whereby exhaustion, muddled thinking, and finances can prevent someone from seeking proactive treatment.
My family has know the wonderful Dawson family many years. Our sons played and grew up together. We loved Chris and he will always be in our hearts as the wonderful person he was. Mental illness can strike anyone of us. Be careful not to judge, it could happen to you or your child. Thank you for the frank article on this subject.
Absolutely. Nobody is immune. Judgement also interferes with healing and has the adverse effect of shutting down valuable conversations.
Very well said. I am so sorry for your loss.
We are living in such tumultuous times; health professionals seem to be in a particularly vulnerable position, with expectations of unrealistic perfection and diminishing support and resources. Thank you for your on-going courage and determination to increase awareness and decrease unmitigated pain.
Suicide is an occupational disease of doctors, in the same way that mesothelioma is a disease of asbestos workers. Ongoing examination and care is, or should be, part of the job. If you’re getting therapy while a physician, you are practicing preventive maintenance.
I really love the heart of the physician vocation. It sometimes is beyond just labor, but is a spiritual expression of self.
Meanwhile, we live in a society increasingly eager to stuff humans into boxes and make them operate according to mechanistic rules, such as “quality measures,” which are more about superstition and control than quality.
Humans often die when treated this way, and such casualties are foreseeable. We doctors, and others who can see this degradation of human existence – ministers, therapists, others – are treated as oddballs, like the Biblical prophets. “Going about insisting that humans be treated like humans – such arrogance! Who do you think you are!? (just a doctor.)
We simply are one of the most exposed of the population to these hazards. No wonder we succumb.
“Suicide is an occupational disease of doctors.” Warnings should be on all applications and at minimum parents and families alerted to the risks so they can monitor their children. Surgeon General’s Warning: Medical school may kill your child (video)
Sincerest grief and hope for healing to the Dawson family.
Pamela, what if you moved up to #1 a requirement that all medical training be structured so that 8 hours of sleep is possible and that less than 6 hours is acknowledged as unhealthy? Good sleep is a cornerstone of good health. It is impossible to have a healthy population of doctors without it. I think trying to be super human is the downfall of the medical profession- like they’re trying to win some medal in a very strange Olympics.
I withdrew very early from the University of Missouri School of Medicine in the fall of 1985. Part of making that decision was an administration that considered 6 hours or less of sleep a night normal. With my limitations that made a career as an MD impossible.
Agree 100%. 8 hours sleep minimum for human safety & health. That’s what we tell our patients.
From I have heard, Japanese workers do some form of physical exercise before they start work. Maybe the all hospital staff and those in private practice should do something like that before they start work and after their work ends.
Certainly in heath care the environment should support health for all. During med school I met a resident who had not left teh hospital in a week. His wife brought him clean underwear every day or so. I just watched Michael Moore’s film SiCKO again tonight. The level of inhumanity in American health care is shameful.
As a nursing leader in the unit of the hospital where Chris did residency, I was appalled when I heard that our residents work 12 out of the 14 days every 2 weeks. How is that healthy?! But who in their right mind would think that that would promote learning?! We have these people who are devoting themselves to fixing others when they are have no resources or time to fix themselves. We were all rocked hard by this and will spend a great deal of time supporting his friends and colleagues that must continue on. Wonderful article.
Regarding work hours (which are in violation of the UN Declaration of Human Rights): On March 10,2017 the ACGME (Accreditation Council for Graduate Medical Education) made the reckless decision to increase work hours to 28-hour shifts for new doctors (after receiving a petition with nearly 80,000 signatures begging them to intervene on these very issues to stop stop the suicide crisis among residents. Here are the catastrophic consequences of their decision. Here are actual quotes from physicians (de-identified with some patient details changed to protect confidentiality):
“I did my internship in internal medicine and residency in neurology before laws existed to regulate resident hours. My first 2 years were extremely brutal, working 110 – 120 hours/week, and up to 40 hours straight. I got to witness colleagues collapse unconscious in the hallway during rounds, and I recall once falling asleep in the bed of an elderly comatose woman while trying to start an IV on her in the wee hours of the morning.”
“I ran a red light driving home in residency after a 36 hour shift. Got pulled over. It was sobering: I was not fit to use my driver’s license, but I had just been using my MEDICAL license for over a day non-stop!”
“I have made numerous medication errors from being over tired. I also more recently misread an EKG because I was so tired I literally couldn’t see straight. She actually had a subarachnoid hemorrhage and by misreading the EKG I spent too much time on her heart and didn’t whisk her back to CT when she came in code blue. She died.”
Read more here. (And listen to my podcast on this topic).
Hi Pamela, Thanks for verifying that asking for help should not be punitive. All mainstream mental health “care” is punitive. If you go inpatient you are stripped of all human rights and that can be extremely traumatizing for many people. Even seeing a therapist involves getting a diagnosis put on your record. You can be coerced onto disability which will reduce your chances of ever working again to about nil. This is true not only of doctors but of anyone.
Many organizations exclude people who have sought help. This includes churches, Big Brother Big Sister, dating services, many landlords and places of employment, and job training organizations. They exclude whether it is legal to do so or not, and many of these organizations will flat out deny that they do this. The colleges are now forcing people who seek help to take a leave of absence. This is now written into college policies around the USA and Canada, and many other countries. There’s a petition going around demanding that these policies be scrapped, which of course I signed.
I can’t tell you how many applications I’ve filled out that ask me if I have ever sought help for…and then they list various supposed mental disorders. I have learned to leave that blank.
Julie
I think many doctors have learned to leave this question blank too.
I find this story so interesting, as well as heartbreaking. This couple lives in the same town & Rachel went to the same school as my husband & his brother.
When I was in nursing school (LVN), we were encouraged to journal our daily thoughts & experiences. We were also encouraged to do yoga & other various self healing activities. I found it therapeutic when I’d had a horrible week to recap & kind of debrief if you will including learning some ways I could’ve handled situations differently & carried this practice into my BSN training. What if this same practice were included or introduced in medical schools? Along with getting enough rest, practicing some healthy activities would likely be beneficial. You cannot possibly be prepared to heal, if you as the healer needs healing. It may sound over the top granola, but maybe crunchy is what we need!
Just when will enough be enough?
Either we change this very broken system now or attach a black box warning to medical school applications!
Here it is: Surgeon General’s Warning: Medical school may kill your child
I probably have had as much exposure to physician suicide as any medical professional I know, maybe besides you. I have helped numerous colleagues off of edge. Many I just didn’t see coming. I am still trying to get the reprint of the article I wrote for our national spine magazine on MD suicide relating my personal journey. What kills MD’s is suppressed anxiety and anger, but those are words that are now allowed in our profession. I think this is a great article and I am great affected by each one of these stories. I just discovered that we will be on the air together this next Thursday night and am really looking forward to hear your thoughts. David Hanscom
So excited to speak with you in a bit David. Getting ready to log on to the session now 🙂
I suppose there are many like me who lurk, read your posts and tweets, read your blog, may occasionally contact you in fact, and just say thanks. Good job. I appreciate your message. I thought of you the other day and I wish I could say it was for good reasons, though I believe it had a good outcome partly because of you. And all of us out there.
I experienced depression for the first time I think in medical school. There were multiple unexpected and tragic deaths of friends and family, strangely in a cluster of time. I also struggled with my perfectionism the first two years and couldn’t figure out why I was so bad at taking exams (read that developed severe exam anxiety, I suppose). I was exhausted from arriving at 3am and leaving at 8pm every day for clinical rotations. One day, I broke down and cried. I realized that I actually didn’t care if I lived or died. Mind you, I had no intention to die, no plan, nothing like that. But I had always had a fear of dying previously because there would be so many things I wanted to do in my life that would be left undone. So many loved ones I would leave. Just terrifying. And then one day, it was not. That was so disturbing to me that I put myself on an SSRI after carefully researching the right evidence-based treatment for depression, making sure not to underdose like so many do. It did get better and I did successfully stop the SSRI later. But the only person I ever told about this was my spouse, who was shocked. It’s sad but I somehow knew that going to seek help outside would have labeled me and created issues later, and now I have seen that instinct was right. I’m happy I did not pursue help officially, but sad that I could not, as I probably needed it.
Through the many years of postgraduate training I have on and off experienced anxiety, moderate amounts of depression, feelings of isolation, feelings that I would never be good enough. Total imposter syndrome. We are always reminded of our flaws, our lack of knowledge, what we need to “fix” about ourselves. And it wears on you. It is like this irritatingly sore stimulus that I want to retreat from but stick it out because I’d hate to suddenly be seen as a wuss.
I was in a really bad place the other night. And this is when I thought of you. I had an argument with my usually supportive spouse who for some reason was in a terrible mood and decided to lash out at me, pointing out annoying things that I do and reasons why they just couldn’t even look at me sometimes. Yeah, people say mean things when they are fighting (most people). Perhaps opening up an unhealed wound, I could not take the criticism and things just escalated. But that’s not really the important part of the story. People in relationships can have issues when they get so close for so long. I know it wasn’t real. BUT. After taking that irritating stimulus endlessly poking for so many years at the hospital, always thinking I wasn’t good enough, I was incapable of taking any more suggestion that I was doing things wrong. Especially in the only safe place I had. I shut down. I sobbed for hours. Alone. In the bedroom. In the dark. Next to my nightstand. Which contains a handgun. So, yes, I have access. And I sat there on the edge of the bed. Thinking about how I could stop feeling how I felt. Imagery of what I could do with the gun entered my mind. Vivid imagery. I fought the desire to open its hiding place and feel its coldness, look at it. I thought about how ridiculous I was being. After all, I’ve taken care of so many GSWs. They are horrid, especially to the head. But it would be the best way to not face who I’ve become. This ridiculously in debt, useless surgeon, who will never be good enough, and who is absolutely terrified because at some point everyone will discover how incompetent I am. Not good enough. Never good enough.
And I thought of you. Of stories you post. And I stopped. I may still believe some, or a lot, of the “not good enough” things that I hear almost daily at work. But I refuse to become a statistic. I have too much to offer in medical education. And damn it, I know I am at least a good-enough surgeon. I know I do not put patient’s lives in danger. I may be slow at times, but I am meticulous. I may not be able to answer a rapid fire pop quiz question in detail about this or that but, before I operate on a human being, I review every tidbit of information I possibly can get my fingers on to be sure I do the right operation, the right way, and help the patient. I know when not to operate and who not to operate on. I also know how to recognize and appreciate those around me in the operating room that keep the day going and not be an a-hole surgeon who treats people like crap. Nobody, for all their criticism, could ever say I am unpleasant or have a bad bedside or work manner. I am professional. I avoid confrontation (perhaps to a fault). I believe in negotiation. I gave myself enough of a pep talk to make it through a weirdly dark night. Though, I do feel like I just talked myself up so that I could go back in to work and “take it” like I have for so many years, at least I know I will not be part of your 600+. Hopefully I will remain strong to lead by example, since I am in academics. I know there will be new stresses. Old ones will creep up on me as well. But the culture of change starts with us, the ones who silently “took it” for so long.
Thanks for everything you do.
I am so very glad that you knew you were now alone, that the stories of others who have survived these dark times could pull you through. And I hope you know that you can always call me. 541-345-2437 (if I don’t answer, I’m with a patient or talking to another doc so just leave a message and I WILL call you back. You are not alone.
Wow what a story. I too want to chime in that yo are not alone. Surgery residents are grateful for attendings like you/ Surgeons that are thorough and thoughtful and treat patients well. Doctors that take it seriously when they tell a family member “we will take good care of your loved one”. Please continue to do the good you do, perhaps the only thing I can add is please remove the gun from your nightstand drawer. Lock it away safely for the purpose you obtained it which I suppose is for protection. Just a few days ago, a young child died by one at his home. I don’t know if you have children or grandchildren so just as you are mentally keeping it away from you, physically keep it away from all.
Excellent advice.
I am stunned by what you wrote not only about Dr Dawson but all you have studied and found out about 669 doctor’s. It’s frightening and shocking all in one. My deepest condolences to Mrs Dawson and all who have been through the same. God grant you love strength courage and healing. Go in peace! ????????????
699 – now closer to 710 I believe. I need to update the list on my blog. It’s a cycle that won’t stop until we talk about it.
It has often occurred to me in these years of training that the demand for perfection and all the criticism is handled differently by different personalities. This is regardless of skill in the OR. It is meant to motivate surgeons, who have the humbling privilege of patients who put their lives in our hands (literally), to be as good as possible. Almost all who survive training do have the effect of reading more, practicing more, and trying to learn from every situation. People like me, and when I think of it honestly, are pretty skilled technically, but plagued by anxiety of not doing enough, not prepping enough, second guessing decisions. Others have an already present social personality disorder fueled and seem to develop an over the top ego, no self doubt or questioning of their assessment and plan (which I consider dangerous), and have variable amounts of actual skill. Bad results, if they even admit / accept there are bad results, are blamed on patients. Whereas people like me blame every nonideal outcome on something we should have done differently, even if there are factors totally out of our control, even if whatever it was that should have been done differently eludes us. It’s easy for me to say I don’t want the other type of surgeon around because they make me nervous from a patient safety standpoint, and from a personal standpoint, but that’s too simple a view. Some of those high ego folks are damned good at what they do, and make good decisions, and save lives. Perhaps it’s not just that we should select out that personality type but teach better coping skills for each type. One needs to learn to question or play devil’s advocate even if just for a split second, the other needs to learn to trust their training and instinct.
Thank you do much for your candid analysis. Tonight I will be speaking with surgeons in a private group setting and will certainly share many of your perspectives for further group discussion.
Hi Pamela and Ideal Medical Care Community.
I’ve shared the following with my contacts:
I suggest you check out the American doctor, Pamela Wible’s work on doctors’ suicide and mental disorders, here https://www.idealmedicalcare.org/
She has been trying to get the medical profession for some years now to change its schooling, practices and insurance policies which are authoritarian and coercive and serve only the few at the expense of the many. The high rate of suicides and mental disorders of doctors are caused by the Un-Health System itself. As Pamela points out we do not need seminars on “burnout” and “building resiliency”. We need to change the System.
I would add to the suicide of doctors the deaths of their patients–iatrogenic harm–due to the lack of care for patients our doctors understandably display due to the lack of care for our carers. Medical errors are the 3rd leading cause of death in the U.S and most other developed economies as well—as some researchers have put that as 1st.
Do away with the crony capitalism—the corrupt cartel of governments and their regulatory agencies, insurance companies, the pharmaceutical and other medical industries—that currently infects everyone within the Un-Health System and is the root cause of the suicides and mental disorders.
I do not think more “Forums” by government backed panels will make any substantial changes to the destructive environment.
As I have been pointing out on the Facebook page I created to address this issue, Carers for Health Carers
the “Iron Cage” as I call this crony capitalist collusion of special interest groups, is not made for free humans but for obedient slaves.
It is not a matter of lessening the number of beatings the inmates receive or giving them lessons on meditation to make them more compliant; rather the entire penitentiary must be abandoned and new forms of direct patient to doctor interactions created without all the intermediaries interfering and taking their slice of the profit.
As Buckminster Fuller advised, don’t fight the existing reality, to change something, create a new model that makes the existing model obsolete. Pamela is doing that with her “Ideal Medical Care” movement as is the Free Market Medical Movement.
Thank you Jack!! This is a global public health crisis and needs to be treated as such. Really appreciate your advocacy & support. Keep talking. Keep sharing. Tides will be turning in 2018.
Very good article. It’s time for the silence and stigma to end. Hope for healing for Rachel.
This article hits very close to home for me. I have a severely autistic son. My husband has chronic kidney disease and is on dialysis. I work in a very busy hospital and I am often stressed out by the fact that I am alwAys giving… giving myself to patients, my husband, my son. I am so tired. I often fantasize about escaping it all.
Please contact me. I’d like to speak with you. https://www.idealmedicalcare.org/contact/
And then there’s the suicidal spouses. I was one of them. Plastic surgery residency was BRUTAL! And being a new attending was WORSE! “Wait! What? Is this my life? REALLY?!?!”
Praise God Almighty for His healing touch!
With much prayer, counseling and perseverance we are in a very good place!
I can understand suicidal doctors. What I can’t understand are homicidal ones. The stress of being a surgeon propels this man to kill his children? This is a downright malevolent act. Much more to this story than meets the eye.
Absolutely more to the story. Many missed opportunities for intervention. It didn’t have to come to this. Surrounded by medical professionals every day, a med student or doctor should be able to get the help they need without fear, secrecy, hiding, self-prescribing, drinking alcohol to excess. Many, many missed opportunities for health professionals to have intervened properly in this case. Ignoring a problem is never the way to solve it. Things will inevitably get worse if untreated.
IT ALWAYS HAUNTS ME THAT ONE OF MY CLASS COMMITTED SUICIDE SHORTLY AFTER GRADUATION. HE WAS A B STUDENT BUT RELATED TO ME ONCE HIS MOM EXPECTED ALL A’S. I HAD NO IDEA HE WAS SUFFERING. HE DID ATTEND A RELIGIOUS SERVICE WITH ME ONCE BEFORE HE GRADUATED.
Can you please share name & obituary so I can make sure he is on my registry? Thanks. I’ll also email you.
I can understand why doctors commit suicide because they were whistleblowers considering how facts that government at all levels don’t do a thing to protect them.
Read about Steven Ortiz MD. Active FBI investigation. Died as a whistleblower. Justice coming posthumously.
Somehow as educators and even as fellow students we fail our colleagues in not recognizing this level of depression. In 1980, I had a heart attack at 38 yo and the same year 4 of my medical school classmates took their own lives. As I reminisced in the coronary care unit I realized that the 4 all could have been recognized by us as astute observers that we were training to be. One very close friend went into surgery to match his father, but I felt he was not the type to be a surgeon but would have been a great internist.
We need to look at the holistic approach to medicine but also to the holistic way of training students and residents. We need to be able to help our residents transition to a more suitable residency when we see dark clouds ahead.
We hope to start a medical school with these concepts in mind and keep the process going well into post-graduate training and future career!
Thank you so very much for your incredible and incredibly important work.
Oh and I just accepted your Facebook friend request. You are the last one in (they only allow 5000 friends). Let’s talk soon 🙂
Pamela,
I saw your TED talk. I loved it.
I love my field of medicine. However, physicians don’t have anyone representing them, when they are employed. The AMA?! Please..I figured out how useless they are, back in Med school.
When the healthcare-pharm-insurance collective came up with the oblique term “Providers”, they automatically pushed us into a Proletariat category.
We become the same as far less trained “providers’.
If we are proud of being a physician, we are chided: don’t be Elitist and Arrogant!
Unqualified (often) administrators and families become VIPs in clinics and EDs. The physician (primary care) is demoted to slave level.
The specialists, as long as they bring in money, will be “respected” by Admin. What if their fees are capitated? When there’s no fee-for-service? When the economy dictates a more realistic reimbursement for them? Then they [specialists, surgeons] too become Worker Bees. Then all Providers will have to listen to our incompetent Masters.
This scenario causes great stress.
Physicians who stand up for themselves are labeled as”difficult to deal with”, no “team spirit”.
They are expected to be good little slaves.
They are expected to say “Thank you for my job; I hope to keep it! How are my Press Ganey scores? I’ll work harder on Patient Satisfaction!”
Expected to ask “how can I help you skim more money from my services, O Administrator-parasite?”
We need Unions, Pamela. What do you know about viable physician unions?
We need to stop referring to ourselves as ‘’Providers’.
I agree with a previous Kevin MD doc, who said:
“I didn’t go to Provider online school. No, I went through 16 years of full time, on campus, rigorous academic schooling/training after high school. I didn’t get a skimpy, online medical degree., and a rubber-stamped certificate to practice Medicine.”
We physicians are not Administration’s well-trained monkeys.
We won’t have power unless we have a seat at the negotiation table.
Powerlessness is the preamble to depression, worsening depression, and possibly suicide.
Some physicians may snap, and go postal.
Shouldn’t we do some Preventive Care before some of us go Postal?
Before they take away guns. That won’t solve a damn thing.! We have money. We can find any gun on the black market.
And guns aren’t the only way, right? There are cars, trains, ropes, tall buildings, rivers, drugs… can the government remove those too?
Physicians, unite. Get back our power. Power to reduce work related stress. Power to change the conditions we work in. Power to keep more of the money we earn. Power to hire and fire Administration.
Agree 100% and a legal teal is assembling now (JD-MDs). Organizing. Unions. Legislation. This next 12 months WILL bring some exciting changes. Have you seen the forthcoming film – trailer here: http://donoharmfilm.com