
Article ranked top 10 on Medscape for 2018
He was the go-to sports guy in Washington, DC. A masterful surgeon with countless academic publications, he trained orthopaedic surgeons across the world and was the top physician for professional sports teams and Olympians.
Dr. Benjamin Shaffer had it all.
Yet Ben was more than a stellar surgeon. He was a kind, sweet, brilliant, and sensitive soul who could relate to anyone—from inner city children to Supreme Court justices. He was gorgeous and magnetic with a sense of humor and a zest for life that was contagious. Most of all, he loved helping people. Patients came to him in pain and left his office laughing. They called him “Dr. Smiles.”
Ben was at the top of his game when he ended his life. So why did he die?
Underneath his irresistible smile, Ben hid a lifetime of anxiety amid his professional achievements. He had recently been weaned off anxiolytics and was suffering from rebound anxiety and insomnia—sleeping just a few hours per night and trying to operate and treat patients each day. Then his psychiatrist retired and passed him on to a new one.
Eight days before he died, his psychiatrist prescribed two new drugs that worsened his insomnia, increased his anxiety, and led to paranoia. He was told he would need medication for the rest of his life. Devastated, Ben feared he would never have a normal life. He told his sister it was “game over.”
Ben admitted he was suicidal with a plan though he told his psychiatrist he wouldn’t act on it. Ben knew he should check himself into a hospital, but was panicked. He was terrified he would lose his patients, his practice, his marriage, and that everyone in DC—team owners, players, patients, colleagues—would find out about his mental illness and he would be shunned.
The night before he died, Ben requested the remainder of the week off to rest. His colleagues were supportive, yet he was ashamed. He slept that night, but awoke wiped out on May 20, 2015. After driving his son to school, he came home and hanged himself on a bookcase. He left no note. He left behind his wife and two children.
I feel a kinship with Ben, partly because I used to suffer from chronic anxiety that I hid under academic achievements, but mostly because I’m a cheerful doctor who was once a suicidal physician too. In 2004 I thought I was the only suicidal physician in the world—until 2012 when I found myself at the memorial for our third doctor suicide in my small town. Despite his very public death, nobody uttered the word suicide aloud. Yet everyone kept whispering “Why?” I wanted to know why. So I started counting doctor suicides. Within a few minutes I counted 10. Five years later I had a list of 547. By January this year, I had 757 cases on my registry. As of today that number is 1,013. (Keynote delivered at Chicago Orthopaedic Symposium reviews data and simple solutions to prevent doctor suicides).
High doctor suicide rates have been reported since 1858 (1). Yet 160 years later the root causes of these suicides remain unaddressed. Physician suicide is a global public health crisis. More than one million Americans lose their doctors each year to suicide—just in the US (2). Many doctors have lost several colleagues to suicide. One doctor told me he lost eight physicians during his career with no chance to grieve.
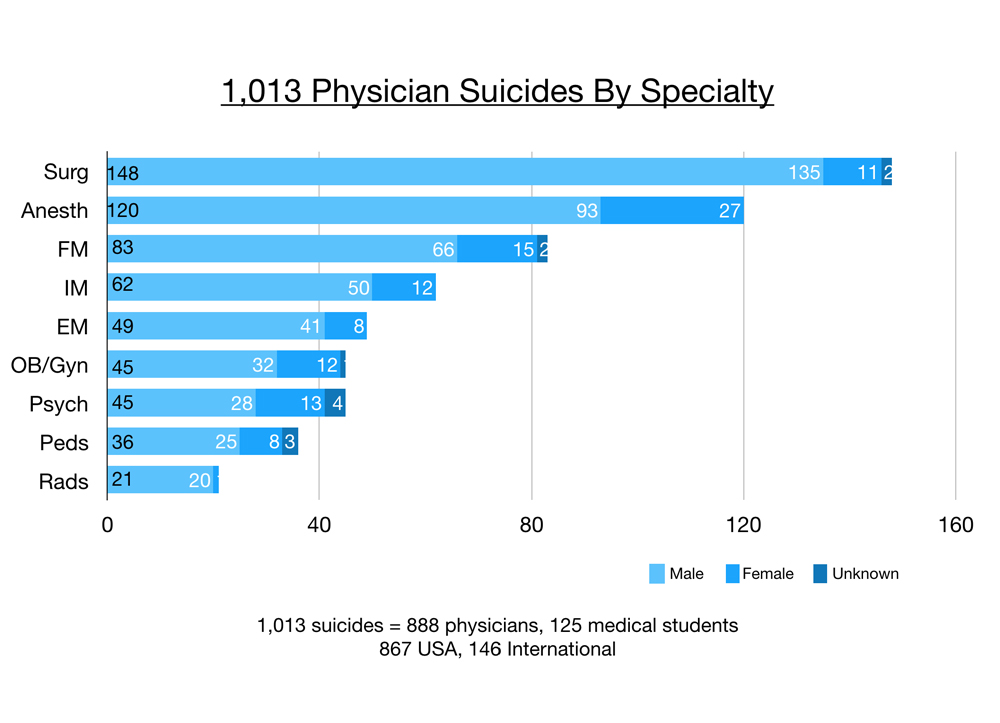
Of these 1,013 suicides, 888 are physicians and 125 are medical students. The majority (867) are in the USA and 146 are international. Surgeons have the greatest number of suicides on my registry, then anesthesiologists. (3)
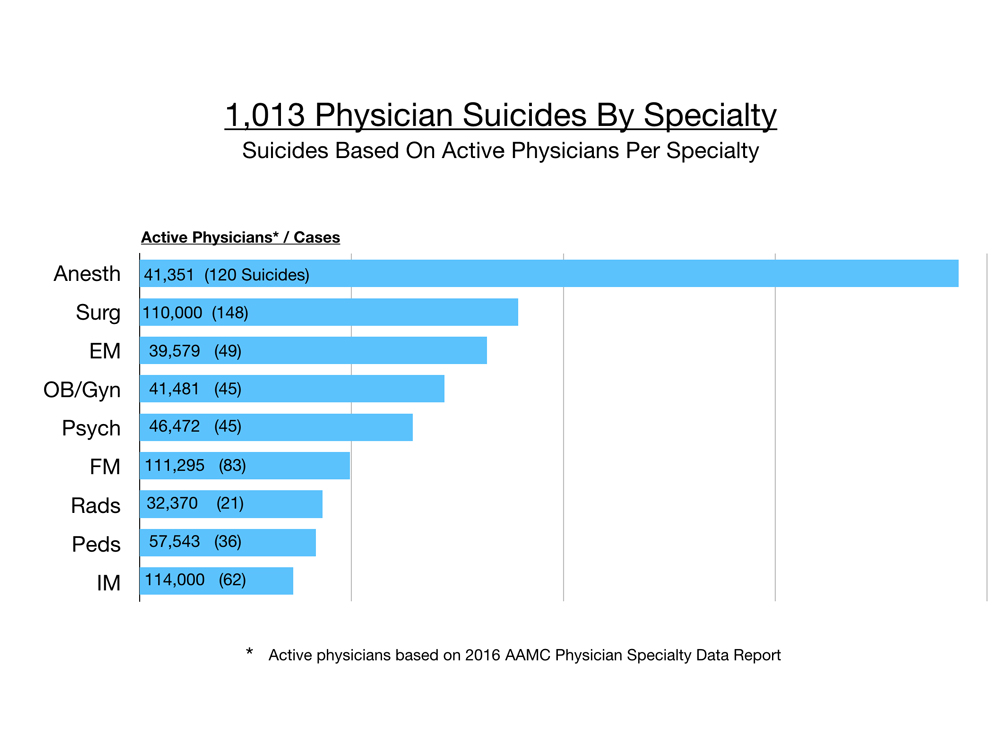
However when accounting for numbers of active physicians per specialty, anesthesiologists are more than twice as likely to die by suicide than any other physician. Surgeons are number two, then emergency medicine physicians, obstetrician/gynecologists, and psychiatrists. (4)
For every woman who dies by suicide on my registry, we lose four men. Suicide methods vary by specialty, region, and gender. Women prefer overdose. In the USA, men use firearms. Jumping is popular in New York City. In India, doctors are found hanging from ceiling fans. Male anesthesiologists are at highest risk among all physicians. Most anesthesiologists overdose. Many are found dead inside hospital call rooms.
Doctor suicides on the registry were submitted to me during a six-year period (2012-2018) by families, friends, and colleagues who knew the deceased. After speaking to thousands of suicidal physicians since 2012 on my informal doctor suicide hotline and analyzing registry data, I discovered surprising themes—many unique to physicians.
Public perception maintains that doctors are successful, intelligent, wealthy, and immune from the problems of the masses. To patients, it is inconceivable that doctors would have the highest suicide rate of any profession (5).
Even more baffling, “happy” doctors are dying by suicide. Many doctors who kill themselves appear to be the most optimistic, upbeat, and confident people. Just back from Disneyland, just bought tickets for a family cruise, just gave a thumbs up to the team after a successful surgery—and hours later they shoot themselves in the head.
Doctors are masters of disguise and compartmentalization.
Turns out some of the happiest people—especially those who spend their days making other people happy—may be masking their own despair. Reading this excerpt from the 1858 Manual of Psychological Medicine, I’m reminded of so many brilliant doctors I’ve lost to suicide: (1)
“Carlini, a French actor of reputation, consulted a physician to whom he was unknown, on account of the attacks of profound melancholy to which he was subject. The doctor, among other things, recommended the diversion of the Italian comedy; ‘for,’ said he, ‘your distemper must be rooted indeed, if the acting of the lively Carlini does not remove it.’ ‘Alas!’ ejaculated the miserable patient, ‘I am the very Carlini whom you recommend me to see; and, while I am capable of filling Paris with mirth and laughter, I am myself the dejected victim of melancholy and chagrin.’”
Many of our most inspiring and visionary leaders—artists, actors, even doctors—suffer from mental illness.
Yet students enter medical school with their mental health on par with or better than their peers. Suicide is an occupational hazard in medicine. Doctors develop on-the-job PTSD—especially in emergency medicine. Patient deaths—even with no medical error—may lead to self-loathing. Suicide is the ultimate self-punishment. Humans make mistakes. When doctors make mistakes, they are publicly shamed in court, on television, and in newspapers (that live online forever). As doctors we suffer the agony of harming someone else—unintentionally—for the rest of our lives
Blaming doctors increases suicides. Words like “burnout” and “resilience” are employed by medical institutions to blame and shame doctors while deflecting their own accountability for inhumane working conditions in failing health systems. When doctors are punished for occupationally induced mental health wounds, they become even more desperate.
If physicians do seek help, they risk being disciplined. Doctors rightfully fear lack of confidentiality when receiving mental health care as private conversations with therapists could be turned over to medical boards and illegally accessed by their supervisors via electronic medical records at their institutions. So physicians drive out of town, pay cash, and use fake names in paper charts to hide from state boards, hospitals, and insurance plans that interrogate doctors about their mental health and may prevent or delay state licensure, hospital privileges, and health plan participation.
With a great work ethic until their last breath, doctors are often checking in on patients, reviewing test results, and dictating charts minutes before orchestrating their own suicides. Many leave apologetic heartfelt letters detailing the reasons for their suicide for friends, family, and staff. One orthopaedic surgeon simply wrote: “I’m sorry I couldn’t fix everyone.”
Doctors choose suicide to end their pain (not because they want to die). Suicide is preventable if we stop the secrecy, stigma, and punishment. In absence of support, doctors make impulsive decisions to end their pain permanently. I asked several male physicians who survived their suicides, “How long after you decided to kill yourself did you take action—overdose on pills or pull the trigger?” The answer: 3 to 5 minutes.
Ignoring doctor suicides leads to more doctor suicides. Let’s not wait until the last few minutes of a doctor’s life when heroic interventions are required. Most physician suicides are multifactorial involving a cascade of events that unfold months to years prior. So reach out to “happy” doctors today—especially male anesthesiologists and surgeons who are least likely to cry or ask for help.
1. Bucknill, J.C. and Tuke, D.H. 1858. A Manual of Psychological Medicine.
2. Wible, P., 2014. “When doctors commit suicide, it’s often hushed up.” Washington Post.
3. Wible, P. Keynote, 19th Annual Chicago Orthopaedic Symposium, 8/18/18
4. AAMC Physician Specialty Data Report. 2016.
5. American Psychiatric Association (APA) 2018. Abstract 1-227, presented May 5, 2018.
Meet us in NYC September 12 & 13, 2018 for a sneak screening of the Do No Harm film in which Ben Shaffer and nearly 100 physicians who died by suicide will be honored. View trailer here & grab your ticket.
More on Florida physician suicides in Keynote delivered here














Pamela Great article. We lost a cardiologist a little over a month ago. Still hasn’t been shared as an accident or self inflicted. This particular physician and I shared idle conversation 2 days before it happened. Physicians I think have the ability to hide pain, grief, shame etc. As a paramedic in the past I had to tell people “there’s nothing we can do”, but on rare occasions and it was devastating to me, especially when it was a child lost. I cant imagine having to do it daily or weekly. The oncologist that diagnosed my Mom is a great friend and like a brother to me. He shared with me how hard it is for him on a daily basis to inform people that they only have a short time to live. People need to realize that physicians are regular people too and have the same feelings, hurt, guilt, etc that all experience. As you alluded to today’s media TV commercials about malpractice suits just makes it harder on our physicians to stay mentally healthy. I know the work you’ve done and sharing this with all has saved lives. As Patch said to me few years ago when we were all in Baltimore, continue chasing your dreams.
Tim
It’s not only stigma it’s poor diets due to being rushed and pressured constantly. Lack of sleep surely must top the list as well. Other doctors don’t take these things seriously unless they themselves suffer. I work in psychiatry and before antidepressants, anxiolytics or antipsychotics I address the sleep issues. It is often the root cause of the other problems. I talk about proper diet and sleep issues til people want me to shut up but give an exhausted person a good night’s sleep and watch the magic happen. There is too much fucking ego and too little common sense in our profession. Thank GOD for those like you who are working so hard to make things better!
Wow. I never thought about my lack of sleep especially good uninterrupted sleep, could be the reason for my worsening depression.
You are wrong it is not about ego and I think you should apologize. Until you have been a surgeon and the family of a surgeon you have no idea the unrealistic expectations that are poured upon your day after day. You have all the answers yet you do not have the level of responsibility that these people and their families have. And they are truly almost always some of the most humble kind and servant hearted people you were ever meet. There are many times that they never get paid for their work by the patient’s the insurance companies and even the hospitals where they serve on call oftentimes free of charge with no pay. Shame on you for saying its ego. I’m not sure why you’re involved in your field of medicine but that kind of attitude won’t help anyone
Thank you for your comment. I agree. When I applied for medical school in 1974, physicians were respected but the media has promoted physician bashing for years. I miss the comradery of medical school. I have few friends. I feel alienated. Physicians oft times cannot support one another because they can barely support themselves emotionally. Surgeons get little sleep and even less respect. It’s not just the financial reimbursement of medical care which has crashed. It’s a sense of respect that has crashed as well.
my wife played every sport in H.S., was a rock climber, now she hasnt worked out regularly since 2006. It has effected her mood, health.. just not enough time. I got her a great treadmill, used but professional grade so it wont move. And am building her a desk so she can walk while charting 3 hours nightly from 830-1130 pm
Wow!
Thank you for your comment. Although this article is addressing physicians, it affects advanced practice providers as well.
Absolutely. Impacts veterinarians, first responders, NPs, PAs. Nobody is immune. Empaths in the healing arts take a hit from witnessing human suffering & caring so deeply often without support. Starched white coats & fake smiles hide hide a lot of pain.
Wow! I was blown away reading why “Happy” doctors die by suicide. You have been the one and only person/resource that I can connect with. For the record, I am not suicidal, but I have looked at the ceiling fan a lot. Subconsciously?? That is bizzare. I have always been a bright and shiny “Happy” guy. As an ER tech back in the day, staff and patients used to tell me “Don’t change”. Well, sadly, I have. I look less and less forward to going to work. My friends think I have it made because I am a doctor, a beautiful family and “Stuff”. Currently, me and my wife are struggling terribly. Medicine has changed me. Yep, I smile. Yep, I’m charming. Yep, I can light up a room. But I am in pain. I am overworked, underpaid and micromanaged. I don’t have my own practice where I can work at a safe place. I have isolated myself from friends and family. Some justifiably so. I have been seeing a psychiatrist since medical school began up until now. I have major anxiety and insomnia. I spent 4 years in the US Army Infantry and used to be able to sleep on top of a tank in an instant. It was medicine that damaged me. Surprising. I thought Fort Benning, Georgia would have evoked what now ailes me. Currently, I am on multiple meds…..benzos and wine make life better right? I have had relations with my wife once in the past year. We have tried marriage counseling twice, but she did not like addressing her issues. I am transparent with psychiatrists and mentors. I have had people in my life that have recently committed suicide. All non-physicians. I always have thought how stupid. Just break up the marriage, get a license in California, buy a 40 foot custom retro Airstream and find a lot on the beach. But I have a beautiful 13 year-old daughter. And I want to see her through high school. I am afraid of failing my boards next month. I am up for partnership the following month..and that would leave a stain on my review. Pamela, not one person really understands the pain I feel. I have felt this way for years now that I had to exit the hot bed of an ER and work now in an immediate care. On a positive note, my stress has lessened. I finally had my first physical in 21 years. I work out as often as I can…that seems to be a strong suggestion from my therapist. It’s funny….he asks me every monthly visit if I’m working out..?? I’ll ask him next week. I do not know why I have never asked before. Back to boards. If I blow them and admin gets wind, well time to start a 3 month process for a job that does not require you to be ER boarded. I seek refuge by mentoring. Despite the above, I interview perspective medical students. I think I have a gift to sense if they will be able to handle the road ahead. I mentor students. I am connected with local colleges, speak and do mock interviews. That is my passion. To come full circle. The ceiling fan. I have stated it down many of nights, in my man cave since I snore and sleep separate from my wife. Once I had a vision of twine. I have “Friended” a personal trainer from my gym an left my phone unlocked. I’ll take the blame for that one. My wife is less than thrilled about our correspondence. I could say “Well you have not been affectionate for over a year”, but that may qualify as an excuse and not justication. Per your article, I started medical school less than par. I suffered bullying. Spiritual abuse. How much time do you have? Pamela. Thank you for being that voice that justifies my pain. I look forward to working with you. I hope my correspondence is not a burden. Bye for now.
No burden. Enjoyed our 57-minute conversation. Hope to meet up with you soon. Maybe a 3-day retreat in Oregon?
EM Doc, I feel your pain. I am an EM doc as well and going thru divorce. Same old insomnia and depression and feelings of despair, but worsened by loss of life-partner/wife. Not suicidal, but fleeting thoughts from time to time to end the pain, because it is pain. Anyways, don’t know your recertification status, but you should remain board eligible for a couple years after your current certification expires. Maybe doesn’t help dealing with humiliation, but you maybe wouldn’t have to leave the profession because for privileges and billing, etc, I believe board eligible carries similar status as board certified. I put off initial board exam for 2 years out of residency to work on new home and move. Was not a problem with the hospital because I was eligible.
It is so enlightening to learn of other docs like me who feel this pain and see that Dr Wible is so moved and caring as to devote her resources to reaching out to her professional colleagues.
I wish you the best and although I can’t know how you are feeling and the nuances of what you are going thru, there is an internal fight I think we as doctors in this field share. Just wanted to say thanks for your response. Helps me to think some things thru.
Jaime
Leave medicine try to work any thing else even for much less money
Deepest sympathy to his Family for him being one of the finest Drs. And caring about his Patients and the Hospital are as Bad cause they just want money
I read your sad but all too familiar case report. One of the themes I hear again and again ad nausea is that doctors either avoid care entirely or sneak to other cities (sometimes hundreds of miles, odd hours, back doors, of course cash). I can be very honest about limitations related to surgery but could never say I had a “mental illness” that required hospitalization and recovery.
Maybe we could help ourselves AND our patients with a major campaign to at least reduce the stigma/stereotypes/ignorance around mental illness, substance use disorders and intellectual disability. What are patients and the general public supposed to think if doctors are not able to get treatment??
Although it doesn’t say which anxiolytic he was recently weaned off of, I’m pretty sure this poor man was suffering from acute benzodiazepine withdrawal syndrome.
Ativan, Xanax, he was on many over the years.
Shouldn’t this critical public health information have been included in your essay? As a trained journalist, I believe it should have been. As a human being, I wonder why you, a doctor, intentionally chose to withhold such critical data for your readers and colleagues. Of all people, wouldn’t doctors want to know what drugs did or perhaps did not “work?”
I was given the difficult task of taking my 1 hour keynote down to a Less than 1500 word essay by the Stanford Journal of Bioethics as they wanted to publish so there ya go! The original has the full version here: https://www.idealmedicalcare.org/33-orthopaedic-surgeon-suicides-how-to-prevent-34/
This was benzodiazepine WD Syndrome, there are TONS of on line support groups with people suffering the imaginable…..it’s real….do the research on this most debilitating syndrome there is.
Ativan withdrawal is the worst most painful of all the withdrawals. Talk to survivors- Protracted withdrawal is not recognized by the medical industrial complex- the drivers of suicide are many and complex but to make a big dent find a way to deal with big pharma greed-the epidemic of psychiatric drugging and psychiatric corruption and falsified data. The medical model of mental illness is a bully drowning out choices and alternatives for people in distress
“Ativan withdrawal is the worst most painful of all the withdrawals.” If you ever went through heroin/methadone withdrawal, you might think differently. Imagine how it would feel to have the skin flayed right off your body and I imagine the pain would still not be comparable to full agonist opiate withdrawal. Not saying benzo withdrawal isn’t bad, I’m saying you just don’t know what a bad day is until you’ve gone through the soul tearing experience of opiate withdrawal. It’s a religious experience, for the damned. It’s hours or days in a hell where the realness of life slaps you upside your head like a bad nightmare. Seconds of agony stretch on to an infinite horizon. You’re hot. You’re cold. You’re on fire. You’re frozen. You’re melting. You’re shattered. You’re reborn. You are destroyed. Over and over and over. Ad nauseum. Invisible air currents are cat o’ nine tails. Scents are garrotes cloying and choking in their offense. And there is dread. And panic.Your life flashes before your eyes and it is all bad. You feel you will never be the same. You can’t. Legs kicking. Snot streaming. Sweat flows like a river. You change clothes every 20 minutes, discarding the wet and foul clothes for fresh ones. But even those have an overwhelming odor. You take a shower and the hot water hits like defibrillator knocking your breath out of you like a sledgehammer. Your heart convulses in your chest. It’s sensory overload on the ocean floor. Sounds are distorted like a bad nightmare LSD trip. Liquid sounds. God has abandoned you. God was never there for you. The devil is truly on your shoulder now. This is a mistake. You’ve got to get well. You vomit. Again. Nothing is coming up anymore. You were wrong to abandon your opiate mistress. Hell hath no fury. Maybe you relapse in that moment of abandonment. Maybe you take that opiate to make the pain go away. But the ghosts still linger. Haunting. You fear nothing but going through this again. You will stop at no cost in order to avoid this again. You must get well. You look at the clock. All of the above thoughts and experiences have occurred over 5 minutes. You still have days to go. Could YOU do it?
Doctor just emailed me: “Please stop sending all these depressing stuff.”
FYI: There is no way to solving the tragedies in the world without discussing them.
It’s impossible for people like you (and me) to look the other way without doing something – anything – to try to help.
Cognitive dissonance runs rampant.
Thank you for your work. ❤️
Great article. How true it is that doctors don’t want to die. They just don’t want to be in pain anymore. I wasn’t surprised by anything in the article except the time lapse between decision to suicide to actual attempt. Less than 5 minutes?!? Sometimes our ability to assess and act on problems can be very hazardous to our our health. DrWible thank you for this article and for your tireless efforts to diminish stigma and shame regarding physician mental illness.
Happy to share the message anywhere I’m needed. Hope those of you who see this in time can attend the NYC screening of Do No Harm film Sept 12 & 13th (2018) –> Get tickets here (and we will have a great panel discussion afterwards). I’ll be there. —> http://donoharmfilm.com
Maybe we should teach people to take more time than 5 minutes on such a permanent decision. Might save a lot of lives.
It’s probably best we not trivialize the significant pain one must feel if suicide is his/her answer.
So: What do we say to the Dead?
Better we say and act it while alive.
Do you know your Colleagues’ eye color? Their favorite escape? Red wine or White? Opera or Rap? Their best joke? Their most embarrassing moment?
Ask. Walk straight up and ask.
And take time– One time– to attend the funeral of a patient you met. Walk up to the front, sit in the back, and attend the graveside, not just the Service. Then when you walk back to the car, before you crank the engine, reflect on exactly WHO you are in this world, not what you do…. Might not be a bad idea to consider also just Whose you are, too.
Set your touchstone, retreat to it regularly; You can abde in it in the middle of a resuscitation if you wish–you’re completely capable of being in both places at once.
____________________
(From LinkedIn)
Thank you…
We commit suicide because we have to. Not as a result of being out of choices.
Black has a darker shade here than anyone else can imagine. And it’s not that far away, as if some remote shore, planet or time.
On my own journey, I’ve come to appreciate the absolute need within us to connect with others, even when we’re alone inside. Whoever you are, wherever you might be, under whatsoever circumstance you might endure: Stand up; rise. The Sleeping Giant lies within. You need but wake him. Or her.
The World is waiting. Every moment
Thank you for the words and way you went about writing a most meaningful post Keith.
When I worked in psychiatry, I found most patients oft struggling to find words to describe emotions.
The youngest however were particularly unaware of that and I found they felt shored up to not try so hard by saying, “I don’t think language was developed to express all we feel. Yet that doesn’t make our feelings and actions ‘lesser, unreal or crazier because we can’t find the right words.”
Today, while reading on Pam’s site, I came upon your reply. You wrote what has taken me a long time to find. Thanks!
My suicide attempt was over three years ago. It was one thought of a number of times, one I had been in treatment for, and one I felt sure I’d never act on.
Despite career changing injuries and surgery that forced me to cut back, I loved working and felt I was thriving despite the toll on body, in soul.
I did not anticipate the ‘less than 5 minute decision’, which occurred after a pleasant enough evening, and as best I can recall, occurred the moment I headed to bed, saw my wife sleeping peacefully and somehow moved to saying, ‘all will be okay; it is time,’ and then I simply moved on to the carefully deliberated machinations to end my life without further thoughts about the decision.
Surviving an attempt, an OD with meds that doctors might think would hit its intended mark, has presented a much tougher place to be.
It’s been a tough journey since.
I am not giving up however.
So, relating to your post, I am taking the time in which I read and reflected as the time I needed today.
I am moved by your written word and felt you ought know you added a helping hand to the things I do in a day, albeit haphazardly now that I have a disabling acquired brain injury.
I think it was both what you wrote and especially how you wrote it, going from question to prose to the poetic, that resonated and deserved my attention and was a balm, a place.
You captured that which keeps me going in the face of losing a career, face, trust, and disparate brain functions.
Connect!
-I could not do this alone.
But connecting is far more important than as part of healing. It is life!
For me, that’s even a connect to strangers or in chance encounters. I’ve found the best of humanity along the way.
-Be there for others and learn to ask for the presence of others if needed .
-Friendship is important and worth nurturing and is not a quid pro quo. Know what’s important to others and put their needs as possibly more important as best fits.
Find/Make Time:
– Know how to use that time to what best suits you.
Though I have plenty of it and can’t keep track of it, the time to do something fulfilling, purposeful, important, even if that’s making sure my dogs’ water bowls are washed out well because I care, is not only a beautiful reward but as vital as food and water for me.
-Be grateful for the time which is ‘now’.
-Be with someone who needs you as their time of earth is ending. To Be With, for me, is the key. And learn to accept, maybe even appreciate, all life’s twists, turns, changes, and passages along with others; they will learn and in that is value.
-I love my music and though life is a perfect backdrop for a playlist, I’ve found myself reading and spontaneously writing poetry.
For me, a poem does a pretty good job when prose, dialogue, even music, falls short.
Poems, in my opinion, are the right ‘place’ for me to be each day. Even just reading one is the right ‘time’ and has been pretty amazing.
Poems, taken in slowly, savored as the finest of the fine, and then reflecting on is a cherished moment.
And though all I wrote about, echoing your words best I could, takes time, the time is worth it.
For what we risk losing, if we don’t make room for that time, is ALL time.
I ramble a bit more than I want. In closing, I chose to write to you for reasons that included a thanks, trying to echo your points and complimenting you on your writing.
Your prosaic followed by your poetic lended to a very meaningful post for me and a nice spot oftime in my morning.
Truly appreciated it and wanted you to know, while you’re here!
Warmly,
Rich
Thanks for your reply – I’ve copied and pasted it to read over again, but what is the most important part is – Connect! That is life itself, and not just a means to healing. Thank you for giving me something to focus on, when I’m feeling that things are pointless/hopeless for me.
I wish you strength and fulfillment as you live the life that has been given to you for a purpose, I’m sure
For Rich….
No man is an island,
Entire of itself,
Every man is a piece of the continent,
A part of the main.
If a clod be washed away by the sea,
Europe is the less.
As well as if a promontory were.
As well as if a manor of thy friend’s
Or of thine own were:
Any man’s death diminishes me,
Because I am involved in mankind,
And therefore never send to know for whom the bell tolls;
It tolls for thee. — John Donne —
Pamela you’re a True Pioneer and only Advocate for Physician Suicide Prevention and leading the National Discussion! The AAP just announced in late May at their annual meeting that now out of all US jobs/professions – it’s not farmers/migrant workers who commit suicide at the highest rate ( that was the actual rate from Great Britain ??) but it’s Sad ? to say it’s All Physician’s !! In fact The current rate is 2X higher than veterans returning with PTSD !
In fact in 2016 I was interviewed by a reporter on News Channel 6 San Diego. Ca due to the fact that I was speaking out Against the Entire Veterans Administration for their Utter and Complete lack of Competence in Care for their Vetetans with PTSD and/or PTSD ! Why ? Currently the FDA has 1 approved drug for PTSD / it’s not good it has many side effects – significantly causes weight gain ; metabolic syndrome ; sexual side effects including prolonged erection – it’s an SSRI originally only Approved for Depression/Anxiety- Sertraline ( Zoloft) ! The VA refuses still to due 2 decade old technology- Pharmacogenomic testing- geisenger health systems in PA was just in Forbes for being the 1st HealthCare to lead the model for this and other Genetic/based Medical prevention models !
The CMO just asked to connect with me on LinkedIn and so did the CEO , Nick Arroyo – of Vantari Genetics now known as UniversalDx…
why is this most important?
Because PGtx testing tells us that 40% of all persons who are given Zoloft for PTSD it Will Not Work !
But the Big Pharma still go around with Criminal negligence & tell Doctors this technology is New & Flawed … lol ?
The model currently in US HealthCare is to treat Based on the Chronic Disease Model – that is why between 2004-2014 80+% !!
The Hospital administration profits have gone thru the roof / why would they buy the Doctors practice?
They were allowed to bill at 50% because Obama’s order allowed them to bill as @Hospital loopholes… wherein Doctor(s) owned practice’s were paid at 50% less …
well they CMS got wind ? of this and stopped it and realized they will now save > 790$ million dollars ? per fiscal year!!
So Hospitals stopped acquiring these in 2014-2015 !
Why is this pertinent to Physicians Suicide? That is the main cause !
Do we really think that > 80% of all US physicians said “ please just take my hard-earned practice ; to work for you as a jack-n-the-box doc punch ?-n-out for half the pay ? and < half. The time off ! The alternative was not good / go bankrupt or Lose your license at the State Medical board due to the label of “ Disruptive physician “ !! So the 4th choice is to “ commit suicide “ or go to jail !
Lastly there is no Opiod crisis it’s a hoax – Doctors are the Scapegoat- and it’s killing them by Suicide at as many as 35-140 a day !
So the California State board member let it slip that they were intentions were to take away the Opioids all – not just restrict and the 2nd was to take away all Benzodiazepines- I was appointed along with her to the 1st ever Los Angeles, Ca Opioid Drug Task Force ! We asked her what will you be treating the public with ?
She literally said “ they can just meditate , exercise and do Yoga ?♀️ “
The CMO/CEO and I walked out together as the meeting ended it was in 2016 June before this Hoax Of weaning Both meds started – and I said to him / I don’t know ?♀️ if you have particular interest in yoga & meditation ?♀️- I do ; I in the past have studied with yogi gurus internationally and can do my own transcendental meditation for pain relief . But the patients I see and refer to pain management or psychiatric or treat – those Spinal cord injured patient due to Assault from Gunshot wound ; multiple sclerosis; myasthenia gravies; Advanced Parkinson’s ; etc etc – if they could “ Do the Downward Dog ? they would “ he told me the problem is when certain people try to reach their way up the ladder of success if you will – they lose sight of everything they are there to go in the beginning- and for us and the only one- is the Patient- to prevent disease or to bring their body to wellness or at least try …
this is the Trillion dollar ? Pharmaceuticals industry and the 23.5 Billion dollar ? Criminal gang Illegal Opioid Drug in all states and county in the USA ??!!!
This Belovec Physician; Mentor ; husband; father Would still be Alive today – if it wasn’t for Men’s Corruption & Greed ! “ he was weaned off his Benzodiazepines/ Ativan and Xanax – to sleep ? he’d been on them for years !
Why ? There is no reason ! 1st to no harm! I’ve also been contacted last month by Harvard university physician they have gathered MD/JD/PhD for all of the above to fight this Debacle and Severe Attack on all US physicians- if it’s not too late …
THANK YOU. Every one of your points is so important.
PGtx (20 years too late) explained the very serious damage/disability caused by SSRIs.
Opioid *crisis* is exactly as you stated. The gvmt will never admit they can’t control the tsunami of illicit drugs conflated with legit RXs FOR THAT PATIENT. Husband is MD (in CA) and knows this, but refuses to discuss it for fear of his job.
Most importantly, the severe dangers of withdrawal-induced suicide with benzos,SS/NRIs, gabapentin, Lyrica,etc.
International Journal of Risk & Safety in Medicine 29 (2018) 175–180
DOI 10.3233/JRS-180018
IOS Press 175
SSRI and SNRI withdrawal symptoms reported on an internet forum
It’s finally being recognized, but WHY do patients have to go to the internet to find this information??? It’s obviously impacting physicians also,but most continue to disbelieve the patients, perpetuating further divisiveness and suicides among all.
There MUST be a way to work together, outside of the current business medical model.
(X-psychopharm involved in one of the biggest fraud whistleblpwer cases in hx,CYP & SERT variants, etc.)
Re the physician who emailed you requesting you stop sending “all this depressing stuff”: I must wholeheartedly disagree with them. Continue to send it. Send it far and wide, and don’t stop. This is for all those who have, and all those who might. It’s for those many many students and doctors bearing emotional pain, and for those who love them. Every day that you continue this work,Dr. Wible, you are telling them they matter. And you are telling the world. I count one of the kindest, most compassionate psychiatrists and human beings I’ve ever known among those who have been lost to suicide. I miss my doctor.
Who did you lose? Confidentially submit name and any other information here: https://www.idealmedicalcare.org/contact/
While very sad to read this, it is important to get the issue out in the open and help people understand compassion for anyone needing help. I am wondering also if there is a direct link to medical professionals in general not getting a lot of training in healthy lifestyles. Lack of sleep is mentioned in the article and comments.
I am not a medical professional. I study doctors who offer great information on healthy lifestyles. I also represent an organization and bio electric device that is awesome in supporting better health, healing, recovery, sleep and more. While knowing people reporting amazing results, relatively few people know about this or for that matter pay attention once they do.
There are solutions for this major issue. More awareness, education and action is part of the process.
Solutions are simple. The problem is secrecy.
I think I have a reason, it may not be accurate, but I am going to take a stab at it any way. Doctors are taught to deal with pain by professional isolation, they may smile and feel empathetic, but underneath they are still professionals and they keep a degree of professional isolation. The problem is that isolation is not necessarily a good thing, you see because when you try to isolate yourself from your pain and suffering, you pay a mental toll, Doctors need someone they can vent at, you notice I used the term vent “at” and not “to”, venting at someone who knows what you are going through allows you to let go, without fear of someone trying to “fix” you, when you are not broken you just need to vent. Now, I am not a doctor, but I use to have ulcers, bad ones, why because everybody told me to push my feelings down, hold back when I was angry, people in my religion said it was wrong to have wrath, but one elder told me to read a scripture that saved my life Ephesians 4:26 “Be Wrathful, yet do not sin”. You see it is OK to get mad, upset, and angry, just do not lose sight of the humanity of the other person and yourself. From that I now express my anger at people and circumstances, and then I go on about my day, I apologize when necessary, and I beg pardon when necessary, I try not to be hurtful yet I let people know when they have crossed a line. I have not had a flare up in over 30 years, I am 52 years old. All I can say to these doctors is to be honest find someone they can talk to and try to vent. This is not medical advice, nor is it theological advise, it’s just advise from a person who had success with venting.
Professional distance IS part of the problem. Disconnection begets disconnection and can untether you from the world—another risky situation for the human psyche.
I have been in his situation, it’s a miracle that I survived. Feel sorry about his family.
We should stop asking the question : “how and why he did it”. We wouldn’t ask the question if he was suffering from cancer. Problem may be that we don’t consider Depression as a disease. The sooner we realize that IT IS a Disease, the better.
Bullshit- show me a brain scan- blood panel- genetic marker- anything that proves this man had a disease.
I encourage all Doctors to engage in prayer. Before anyone says anything, I am aware that not everyone believes in Jesus Christ. However, when a person experiences enough pain to believe that suicide will be the answer for making the pain stop, prayer cannot hurt, (especially when you’ve tried everything else).
Always know that Jesus loves you enough to help you, and He won’t tell your secrets.
Besides, we all need assistance from someone regardless to who we are or what profession we have.
Thank you for a very informative article, which touched on so many important points. The pressure and responsibilities imposed on a physician by society and by him/herself to diagnose and heal a patient are crushing. Physicians receive little or no support in handling the loss of a patient or a poor outcome. It is impossible to save everyone or complete every surgery without complications, yet that is the impossible standard to which they are held. I believe more emotional and mental support should be paramount to keep the healers healthy.
I also wonder what is the percent correlation to substance use for all these suicides particularly with anistisiologists. Having worked in the OR in the past I have seen first hand the number of DR’s and nurses who use drugs.
Another study that should be undertaken. Right now just trying to get anesthesiologists to cover suicide at their annual convention (and they don’t seem to have any time in the schedule to address this topic unfortunately).
Although I applaud you for bringing a very important and necessary topic of suicides in doctors to light, I am perplexed as to why you did not reach out to me for this (and other) talks/articles you have given/written – his wife of 20 years. Shame on you.
Been in very close contact with Ben’s siblings and would love the opportunity to speak with you. Please feel free to contact me confidentially here.
Thank you for putting this out there. And thank you for providing details leading to Dr. Shaffer’s suicide assuming this was done with the consent of his family and legal to do so? Likely there is more to his story. My only point relates to med changes. I’m a therapist in private practice who has observed many people with anxiety disorders weaned off anxiolytics, people who have remained highly functional and successful because of them. New medications are introduced and trouble ensues.
Such important information! As a concerned mental health professional and wife, I will be talking with my husband (a happy physician) about this today!!!
Good move Mary!
Thank you for this great website, bringing attention to something so important.
I think one of the biggest issues is the threat of lawsuits. A single lawsuit from one angry patient can end a career and bring financial ruin. I know physician colleagues facing such lawsuits. After reading this, I will not sit by passively waiting to see if something happens. I am reaching out to them today in support and to see if there is anything I can do to help them get through this.
Pamela,
Please let me help. Thank you for cultivating awareness. I’ve worked with surgeons one-on-one in my yoga therapy practice. It is unfortunately very apparent the level of stress held within the body, energy, and mind. Through yoga therapy there is hope. I’ve seen it help first hand and the studies are there to support. I see clients at a boutique doctor’s office, as well, as all over the country and international.
Please contact me so I may help on any level needed. Thank you, again, for spreading the word.
This is very sad. The man was clearly loved and respected by many.
I wonder if there is a chance that when he was weaned off of the anti-anxiety drug whether he didn’t just experience ‘rebound anxiety’ but much worse anxiety and possibly other symptoms that are known to occur when stopping such medications. These symptoms are often very severe and mistakenly attributed to an ongoing or worsening underlying mental health condition as it may have been in this case.
Doctors need to be much more aware of the risk of severe withdrawal symptoms from anxiolytics such as Benzodiazepines.
I mentioned to my psychiatrist who was treating me for depression and P.T.S.D. (who was also vetted to me as THE psychiatrist in my state to be seen by for physicians) that I was not suicidal any longer but that I was surprised that after three prior years of nearly daily SI that I had not acted on it. Within 24 hrs this psychiatrist without further evaluation recommended to the board that I no longer be allowed to see patients and I was ordered to cease practice. No transition period for my patients nor any possibility to find appropriate care for their follow up. I was told to give them a list of possible providers and that I was not allowed to explain to them any circumstances simply that I could no longer see them. I remain horrified and hesitant to consider returning to practice despite horrendous need in an underserved area.
Very disappointing to see this doctor’s avoidable death might be used in a PR/political way to explore issues pertaining to the medical field and not used in a broader context to explore the Public Health crisis regarding akathisia and psych drug risks vs. benefits. I have doctors and medical professionals in my family and don’t want harm to come to them or anyone else. Yet, I also personally know more about akathisia-induced death than I ever wanted to know.
The physician suicide crisis goes far beyond akathisia and psych drugs (though certainly an element). And these deeper issues need to be explored.
Pamela please email me you have to know what the plan is by the AHA ( American hospital Association) and it’s started here in California…
Imagine being a professor or teacher who gets yelled at by students, who loses 5% of their pay if the student bombs a test, and then complains about it even though they did nothing to study for it.
Imagine working:
35 hours weekly in clinic
21 hours via 3 hours nightly charting
5-10 hours weekend hospital rounding
and nursing home rounding
plus 65+ hours off duty call every other week. Not sleeping right for a decade, unpaid
that is 60+ hours weekly + 65 being woken up and then the hospital administrators suggests you are a .8 32 hour position since you only see patients 35 hours weekly.
Imagine you get turned in for NOT giving a pill to cure colon cancer…there isnt one. Imagine people trash your name around town as being horrible, they are a drug seeker who lied to 3 MDs but you cant say that, you cant defend yourself. Imagine 70% of your baby boomer patients care so little about their health they are obese, do not exercise, imagine a parent says they cant afford $4 for their child’s antibiotic, yet spends more than that each day smoking….
Oh and admin want you to see more patients the month before your unpaid vacation to make up for having the audacity to take a family vacation once every 2-3 years.
and that, thats just scratching the surface. It has changed in the last decade. More paperwork, faster visits, less meaningful interaction, more drug seekers, less power to address it. Being one of the smartest people in America, studying 100 hours weekly for 12 years… and a nurse practitioner who studied 40 hours a week for their masters degree (all of ours worked full time while getting them) and has 1/7th or less the training can do medicine as good and nicer. I calculated mean GPAs between med schools and NP programs, more than 80% of nurses did not have the ability to even apply to med schools… That is modern medicine.. I actually cannot think of any way that it could get worse.. but hey politicians patients and admin have shown themselves to be remarkably gifted in surprisingly everyone in that regard so who knows.
When you try to end your life
There are no get well cards
No Meal Trains even though you’re afraid to leave the house to shop
No GoFundMe page even though the bills are outrageous and your brain can’t process them
No 5K runs to celebrate your fight with a deadly disease
You can’t post on Facebook the yearly markers of your struggle
Friends disappear, but you can’t blame them
Family hopes the pills work
In the community it’s like you never existed at all
No one wants to talk about IT
But just as if you had cancer, you fight for your life every day
The treatments are experimental and costly and don’t always work
The shame and grief are burdens you carry the rest of your life
Which will never be the same. Never
Your wounds are invisible but they feel gaping and raw
And you wonder how it’s possible that no one else can see them
And you live in terror that your kids will suffer the same pain
Because they are the only reason you’re still fighting
Because you ARE NOT A WIMP
And you’ll keep fighting as long as you’ve got fight left in you
At least for now,
YOU ARE A SURVIVOR
thank you
I think it’s great that you’re bringing this problem out of the closet. I’m not suicidal, fortunately, but I’ve suffered from anxiety and depression (I currently take a benzodiazepine). As a non-physician, I often view doctors as being “perfect.” Conquering medical school, residencies, then having the strength to risk failure in treating other people…how could they not be perfect? I had no idea this was such a problem, and it’s good you are trying to remove the stigma.
By the way, I was friends with Ben Shaffer in grammar school in Mansfield, Ohio. We were in several classes together. Even then, he stood out as someone special. If you’re in contact with his family, please convey my sympathies.
I want this article in PDF. It gaves me strenght to fight mi current depressive disorder. And I’m not yet successfully undergraduated.
I wish to read it again when I become a Doctor. I know that I will.
https://www.idealmedicalcare.org/why-happy-doctors-die-by-suicide
Dr. Eric Gluck Sep 14, 2018
@Susan Ricketts @Michael Rosenblatt
‘…there are lawyers and professional groups itching to CONTROL health and administration professionals and subject them to various and sundry regulatory and licensing issues…‘
I have waited to respond to this discussion thread until I read the previous 223 comments regarding the suicide of Benjamin Shaffer MD. What is troubling to me is that comments range from overwhelming sympathy to apathy. The unfortunate reality is these discussions should have and may have been made with Dr. Shaffer before he committed suicide. It is too late to discuss all the various erudite treatment options that Dr. Shaffer should have taken after he committed suicide. Unfortunately, we no longer have the opportunity to understand the reasons Dr. Shaffer decided to take the desperate action to end his life. Regardless, I personally cannot agree with anyone suggesting Dr. Shaffer should have / could have prevented his own suicide even if he was an individual with deep religious or other spiritual beliefs.
Michael Rosenblatt DPM and myself have previously commented during other discussion threads there are incidents when any member of the healthcare-legal industries can too easily destroy a physician’s and other health caretaker’s ability to practice their profession by initiating a Sham Peer Review / Bad Faith Medical Peer Review (BFPR) for economic reasons under the guise of protecting the safety of the general public. There are also legitimate reasons to initiate Peer Reviews against caretakers who actually are a threat to patients’ well being. Therefore, it is essential these administrative actions must not be drawn out for years on end so that legitimate caretakers’ reputations become so damaged their livelihoods cannot be salvaged.
So, I am left wondering if Dr. Shaffer was dealing with insurmountable economic / professional pressures, which I personally believe may not always be successively relieved by medication, occupational, physical, positive thinking, transcendental meditation therapies, etc. So what may cause such economic / professional pressure?
Many of us do not enter into health care in order to enrich ourselves, though some do. So, is anyone unable to acknowledge economic circumstances could possibly lead an individual to overwhelming psychic pressure that can lead an individual to take their own life following a Sham Peer Review / Bad Faith Medical Peer Review (BFPR)?
Anyone who becomes a target of a Sham Peer Review / Bad Faith Medical Peer Review (BFPR) needing to retain an attorney to defend oneself will be saddled with legal fees between $200.00 – $485.00 per hour depending on their location in the United States. The material fact is a surgeon like Dr. Shaffer, if employed, possibly working 7 days per week 24 hours per day earns between $40,000.00 (as a surgical resident) up to $150,000.00 annually (my highest earnings as an employed Board Certified general surgeon on active duty), which equates to approximately $4.60 to $35.00 per hour. This is a material fact that is rarely addressed in discussion threads regarding physician suicides. Even if a physician successfully defends oneself through a Sham Peer Review / Bad Faith Medical Peer Review (BFPR) the victory does not guarantee an employed physician and even physicians in private practice can return to practicing their profession or even change their career paths due to the resulting unrelenting professional stigma that the administrative action created.
I anticipate I will not receive many likes for bringing this up in this discussion thread especially from attorneys and hospital administrators who can earn up to millions of dollars annually without the stress of always having to achieve perfect results.
Dr. Eric Gluck Sep 17, 2018
Dr. Eric Gluck, Surgery, General
@Susan Ricketts @Michael Rosenblatt
‘…there are lawyers and professional groups itching to CONTROL health and administration professionals and subject them to various and sundry regulatory and licensing issues…‘
I have decided to submit another response to this discussion thread after reading now 240 comments regarding the suicide of Benjamin Shaffer MD.
I now propose all heath care professionals must focus on demanding the need to balance the inequity of power between healthcare professionals, hospital administrators, and attorneys during Sham Peer Reviews / Bad Faith Medical Peer Reviews to address the number of legitimate providers whose personal / professional lives have already been destroyed by economic competitors.
Let us all first agree extraordinary financial burdens can lead some healthcare providers to major depression and on to suicide whether they are manic or not. Overwhelming professional financial burden is a single issue all healthcare providers, hospital administrators, and attorneys can focus on and make recommendations as to how to address and lighten this burden. So, I will begin by listing some suggestions and hope others involved in this discussion thread will consider adding their input to the list of my recommendations, which hopefully may lead to a process that improves the current management of Medical / Surgical complications by administrators / attorneys and physicians with only the intent of bettering patient care.
My initial recommendations to consider are:
1) Some medical schools are addressing the growing physician shortage by offering new medical school candidates tuition free training so upon completion of their studies they can focus on patient care and not be distracted by overwhelming academic debt.
2) Death / Complication – Mortality / Mortality Conferences need to be incorporated back into weekly / monthly conferences before attorneys can disrupt physician – patient relationships because it must be acknowledged by all heath care providers and attorneys it will never be possible to eliminate all medical / surgical complications from occurring. Lessons learned during these conferences are valuable for all involved and future patient care.
3) Medical / Surgical physicians involved with the patient at the time of complication should stay involved in the care of the injured patient since they have a vested interest in seeing their patient have the best possible outcome.
4) Malpractice lawsuits must be limited in a heath care system by primarily focusing on patients’ medical / surgical needs following medical / surgical complications before physician – patient relationships can be disrupted by attorneys quickly initiating lawsuits.
5) Attorney hourly fees and Health Care Administrative salaries need to be addressed so that health care providers can focus primarily on the heath care needs of injured patients as opposed to focusing on how to avoid enormous financial damages that can be awarded by over zealous settlements in order to avoid civilian juries who are likely not equipped with the requisite knowledge to render life-altering financial decisions for both physicians and patients.
6) Employed physicians have been paid $4.60 to $35.00 per hour taking care of their medical / surgical patients while working for periods of 24 hours per day – 7 days per week. What would happen if Malpractice Attorneys and Hospital Administrators were similarly compensated for representing injured patients, physicians being sued and managing hospital affairs? The compensation gap between employed physicians and malpractice attorneys / hospital administrators must be addressed as a potential starting point in order to reduce the damage to physicians and patients created by malpractice lawsuits and adverse administrative actions.Are there any practicing healthcare providers currently charging, being compensated, and / or earning $200.00 to $485.00 per hour?
7) Physicians with similar expertise who are not economic competitors should be requested to review medical / surgical case complications to determine whether injured patients should consider dismissing the care of their medical / surgical provider and seek legal counsel but not before their current medical / surgical physicians are given the opportunity to continue caring for the complications their treatments may have created.
8) Patients should be able to purchase affordable hospital insurance prior to elective procedures so they can be financially compensated to the maximum dollar amount of the policy in the event an unintended complication occurs instead of initiating lawsuits.
9) The Federal Government should allow early withdrawals from Individual Retirement Accounts (Traditional and Roth IRAs) when available to be utilized without penalty for unexpected healthcare expenses.
10) Health Care Accounts (HCAs) could be established to function similar to Individual Retirement Accounts (Traditional and Roth IRAs) but used for urgent health care needs.
11) The General Population should be able to access similar healthcare coverage as offered to government employees.
12) Mentors who are not academic / economic competitors should be assigned at all levels of training and medical / surgical practice to solely monitor the well being of fellow physicians. This will be very difficult if not impossible to accomplish in view of the current status of medical / surgical practice in the United States and elsewhere.
13) Medicaid must be preserved for the most needy so that no one can be denied healthcare only because of their inability to pay for their own healthcare.
14) …
15) …
Please consider adding your suggestions to this list hoping something positive might be established that will return the physician – patient relationship to being seen as a venerable relationship accepted by attorneys, hospital administrators, patients and physicians, which should not be disrupted by the false belief that malpractice lawsuits benefit patients who have experienced medical / surgical complications.
see previous post dated September 14, 2018:
Dr. Eric Gluck Surgery, General 3 days ago
@Susan Ricketts @Michael Rosenblatt
‘…there are lawyers and professional groups itching to CONTROL health and administration professionals and subject them to various and sundry regulatory and licensing issues…‘
You need to add Pharmacists to your list if you are going to use the term doctor instead of physician. I could add some people to your list if you include pharmacists.
I do have a separate list including veterinarians, pharmacists, and other health professionals. You may submit here: https://www.idealmedicalcare.org/contact/
For registry I’d like the specialty, age at death, date of death, location, and any other circumstances you wish to share (which I shall keep confidential).
How terrible. Seems like the world lost a good man. This sounds like a benzo withdrawal story. I founded a nonprofit about benzodiazepines. We see this happen all the time. People are fine, they come off the benzo and they’re dead. Medicine is very undereducated about benzos and their real potential for harm.
Sadly i see this too often in many fields of medicine. I myself went to schook for a ph.d in psychology. i worked in the prisons, addiction and mental health. I lost many clients to overdose others to suicide. I was on call constantly trying to stop those from self harm or committing suicide. We had no suicide hotline so i was their only lifeline. Years of sleeping terribly, going to funerals and the guilt of what else could i have done took its toll on me. I am trying my best to be treated with antidepressants for panic disorder, anxiety and depression. I cant even conceive of treating patients in my frame of mind. I smile most days when i see people and help them when they ask, but i side im dying. I know first hand the stigma associated with mental health so admitting that i have a diagnosis is humiliating to me. Most days are torturous at best and i doubt i will ever be able to treat another clients knowing what could happen if i dont give my all everyday. We fight the good fight, but in the end we lose a large paet of ourselves duringthe process
I highly recommend that you schedule a session. Happy to talk to you. Reach out here: https://www.idealmedicalcare.org/contact/
I just lost my husband last month to hanging himself. He was not a doctor but he was a business owner. He had never taken any meds in his life but after reaching out for help with anxiety he was given Prozac, Xanax, Buspar and Klonopin. Three weeks later he was gone. I miss him so much and so does our three daughters 9, 14 and 18.
I am so sorry for your loss.
Do any of you people know about iatrogenic benzodiazepine withdrawal? If you have been on Benzodiazepines taking them regularily as prescribed for years – you may need a couple years to come off with compounding. The receptors in the brain for GABA change from the drug. The study on Xanax was so misleading and caused a lot of iatrogenic problems and doctors are not aware – even psychiatrists how to safely wean these…
This is a devastating tread. However, I would like to bring 2 issues to light that might be contributing. I was an Army Medical Recruiter for doctors and I was shocked to find that the majority were on ADHD medication to help them study. I had to turn away 1/2 a million in scholarships so many times due to these meds. This made the doctors unable to join the Army. Psychotropic drugs for high performance was the typical med student, the same doctors who turn around and prescribe them to Kids, go fiqure. The 2nd was when I asked why do you want to be a doctor, it was usually either “my mom and dad told me I had to be one” or “I want to make money” . They won’t be allowed in either. They were become doctors for the wrong reasons with little understanding of the world they were entering and the demands. Many had never worked in a hospital before or even held a job!
The medical field is a brutal world and cutthroat. These are high achievers and very competitive they are in literally in combat every day with the system and saving lives. They are humans not robots.
I feel so sad and dejected for these physicians who felt they had no other choice than to take their own lives.
I’m not a physician, and don’t know the pressure that you all face, but I have recognized a general lack of respect for those of us in the medical field over the past several years. EMR is making it worse. Patients demand 5 pages of forms to be filled out immediately, and EMR tracks everything you do and the time it takes. Every night I make it home, exhausted after a 10 hour shift, only to be greeted by red delinquent charts, and patients directly messaging me through the EMR to ask if they qualify for disability, or chatty people that think we are text friends, asking what people did before DPP4is came out, because their medication is too expensive. Of course, I have no one to talk to, because any doctor’s visit I go to will be recorded in my chart, which also seems to double as some sort of employee record, with people reading it at leisure. I keep my chart clean and all of my problems to myself. I lie constantly that things are done and everything is perfect, but no one seems to know the truth.
Thank you for listening. My heart is heavy for people that suffer and just set out initially to try to help people and make a difference.
What a great article.
May I translate this to Japanese so that everyone to know the terrible work environment around doctors.
In Japan the overtime work of doctors exceeds 1900 hours/year.(not total work time).
Yes, please just link back to the original article. Thank you.
I bumped into this page while Googling “Help me decide to commit suicide tonight.” I love being a psychiatrist. But I also had a lot of depression and some mania in my own life and being a “happy doctor” meant that nobody would help me. I had a mixed episode a few years ago and the doctors I saw did not recognize it. I ended up making my husband leave me and now we have been separated for three years and just when I thought things were getting better I ruined it again. I’m fine now – because I figured out how to treat myself, since most psychiatrists just want to put everyone on high dose weight gainers and meds that do the opposite of each other (Think wellbutrin dopamine agonist and abilify dopamine antagonist all at the same time and then tell the patients “we don’t know how these drugs work” and I never do that). But during the time I relied on these fancy schmancy expensive other doctors I ruined my marriage. And so now I want to die. There is no point in being a good doctor if you have nothing else to live for. I think one of the reasons the suicide rate is so high is that most psychiatrists just pander to the pharma and insurance companies and don’t know what the heck they are doing. It is tragic.
I’ve emailed you. Please respond.
I am sorry for the deaths. I believe the money stress and jealous people cause smart people to go over the edge. Should a doctor taking these meds. treat people? I have been yelled at by pharmacists and doctors in the past five years than in the other 65 years. I remember the doctor who delivered me. He did it all. He was respected and saved my life. I should be in the hospital now. I have a fever and my arm will not move. They say come back if it is worse. How bad does it need to be? Doctors we care about you.
Great Article! My husband was an OBGYN. He was warm, funny, bright, and engaging. Loved by most everyone. He suffered with depression for almost all his adult life.(mostly well managed) He had terrible sleep habits on top of the demands of delivering babies at all hours. As he aged his depression became more difficult to manage. He was hospitalized 4 times. The last time he was suicidal and had anxiety which had not been present before. He began ECT therapy, with good results initially. He began to exhibit physical symptoms that mimicked Parkinson’s disease (not true Parkinson’s). His decline was rapid over the next few years, mentally and physically. He was unable to drive, read, everything was overwhelming. He told his Psychiatrist and me that he wouldn’t act on his suicidal thoughts, but he did. August of 2018 he took a massive overdose of his Nortriptyline. I know he had lost all joy, his brilliant mind betrayed him. It was hard to watch this accomplished man suffer to the point of hopelessness.
Oh no. I am so very sorry Cheryl. I’ll email you privately. I’d love to speak with you. Do you have an online obit? Was there a memorial service by the hospital? How did his colleagues respond? Just devastating to lose someone so brilliant and compassionate. What do you think we could have done differently? What would have prevented his suicide?
Thank you for your response. My husband had made a change in his work situation which precipitated his first hospitalization.(this was about 10 years prior to his suicide) Working for a large hospital which was away from our home and very demanding. It only lasted 3 years and he was let go. He was unemployed for almost a year. He found another position a little closer to home, however he had to stay within a ten minute drive when he took call. His depression was escalating at this time and he was hospitalized again. He was let go after 2 years. He then began to do Locums which took it’s toll. He became suicical 4 years prior to his death during which time he underwent ECT treatments which helped his depression but diminished his affect. By the time he passed he very little contact with his colleagues. His world was very small as everything was overwhelming. I don’t know what could have been done while he was working. He had made some changes during his life that always seemed to turn out positively, so I didn’t realize the toll that the changes he made over his last 10 years were impacting him negatively. To see him dimished and nothing helping was frustrating. The medical community seemed to be at a loss as to how to treat his physical symptoms. They ran every test and they all came back normal. His family physician referred him to a neurologist as he presented with Parkinson like symptoms. The neurologist said it wasn’t true Parkinsons. His severe anxiety, depression, and physical maladies were so limiting I think he felt hopeless. I am not sure what else could have been done. I locked up the gun cabinet not thinking of an overdose. It’s hard to go back and think if a different medication would have helped, but he was limited on what he could take because he had reduced kidney function. There were so many factors working against him I’m not sure what the answer was. Our whole family tried to help him. His obituary was posted by our local funeral home not sure if it can be found on line. Dr. Michael Kush OBGyn, DuBois, Pa (8-6-2018)
I believe all medical professionals need ongoing mental health care. Prevention and early intervention is key. If we as medical professionals wait until we have incapacitating psychological distress then we have done a disservice to physicians and our profession. The culture of medicine must change–starting with destigmatizing mental illness and encouraging mental health care maintenance (kind of like dental health care maintenance). Much easier to intervene and save a tooth while the cavity is very tiny (versus not going to the dentist for decades and then needing implants). I am so very sorry we were not able to help your husband sooner. he deserved support from his colleagues and profession.
I think its safe to say that no student has ever matriculated into a medical school with the game plan:
1- I’m going to work hard and deprive myself of sleep until I’m numb,
2- I’m going to slowly lose all hope of ever being happy again,
3- I’m going to end this suffering.
If you ever suggest this to a 1st year student, most will laugh and dismiss it, but this is basically how it plays out for many doctors. At any given time, most doctors are stuck in Step 1, or Step 2. Reaching Step 3 is mostly a personal decision that some reach earlier than others.
I think the fact is, the lives of doctors are misrepresented on media and leads to false expectations by medical students. By the time these students see what is actually in store for them, they are hundreds of thousands of dollars in student debt. Trapped. With only one realistic way to pay off those loans; stay in a profession you despise more each day.
Maybe we owe it to future doctors to portray their lives more accurately on mass media.
Mental health problem? I don’t think so. I think it’s just plain long-term grief over great loss. And that’s emotional of course, but not a mental-health problem (unnatural).
As opposed to doctors almost exactly 45 years ago, doctors subsequently are not rewarded properly for their hard-earned knowledge, power, sacrifice, and sleep deprivation, because now the HMO’s/Insurance Companies get many of those rewards…instead. (We saw it coming long ago.)
Think about it. Where can an unhappy doctor go with his/her profession but down. Just make sure his/her problem is not a personal one instead of a professional one before he/she gets categorized as a ‘doctor suicide.’ We shouldn’t put any of these suicides in a ‘doctor suicide’ category unless we can rule out personal problems that might have been the cause. We must know ‘why’ a doctor takes his/her own life before categorizing any of them. I was shocked by the numbers, assuming their accuracy. It’s profoundly sad.
Most suicides are obviously multi-factorial. However when one profession has a rate of suicide nearly 3 x the generally population that is alarming. Physicians have all endured human rights violations in their training and many continue to experience the abuse in their practices with hazardous working conditions that would be illegal in any other industry that truly values safety. Think about it: when a doctor works 100+ hour weeks, suffers from chronic sleep deprivation (not to mention bullying, harassment, witness to or unwilling participant in health care corruption)—and then ends up with a divorce or a “personal” problem, what is the genesis of the “personal problem?” Could it be tracked back to professional issues that have destabilized the doctors ability to have a normal personal life?
Thanks for responding, Pamela. I do agree that suicide can be multi-factorial and many likely are. So I guess my point would be that finding the cause of the greater number of physician suicides is important because it appears it could be more their profession than personal life that’s driving them off the cliff. And if that’s true, then isn’t it very important that things change? It would be up to the Medical community to stand up for themselves to change things (not just make more concessions to the HMO’s and Insurances).
I do hope that med students must know what they’re getting into these days? Well, they’re bringing it all on themselves. And… how many doctors are just as unhappy as the suicidal ones but choose to just live with it. How ’bout a survey?
Oh yes, absolutely. The root cause analysis reveals that (at least among the 1,300+ cases I have) human rights violations within medical training and practice have destabilized these otherwise high functioning brilliant and compassionate people.
Getting a medical education (MD) has always been difficult, and serves to weed out those who would most likely be wasting their time trying. This is not all bad. But I see the ongoing after-graduation abuse as inflicted by the HMOs and other Insurance companies who think they’re the doctor instead…getting the bulk of the money while the doctor gets all the work/exhaustion/liability.
Just one more thing. I believe that people that want to die are suffering from a personal need that is not being met in their own lives: physical, spiritual, social, emotional, whatever… figure that out and there’s the cause?
Hi there, I am trying to find statistics about the incidence of suicide in physicians and other providers who have been involved in a medical error. I know that it can be a source of self-doubt, depression , grief and even self-loathing; i am sure it has been a reason for some of those suicides, but cannot find statistics on incidence of suicide attributable to making a medical error or even a near-miss. i wondered if you might have seen any numbers, given your interest and expertise in this area!
At my institution (i am a hematologist/oncologist and palliative care specialist), we have developed peer support and training in peer support. I am hoping it will help. Thanks and please keep up the good work!
Dear Pamela, thank you so much for your incredible work and all the passion behind it.
Dr. Shaffer was, hands down, unequivocally, the best, most caring, most off-the-charts incredible doctor I have ever seen for anything. He operated on my shoulder when I was in my mid-20s and, because of the decisions he made and care he took, I had a remarkably fast and total recovery. I still think of him every single time I need to go to a doctor. He was an A++ in terms of skill AND bedside manner– and benchmarked against the incredibly high standard he set, I don’t think I could honestly rate anyone I’ve seen since above a B+.
I reached out to him in 2013 when I needed a trusted recommendation for an ortho in NYC. He called back so quickly, was warm and vibrant and caring as ever, and remarkably remembered so many details of my situation from 20 years earlier. I was starting a new organization to help adult tennis athletes at the time and told him I really wanted to find a way to involve him somehow down the road to have him present if we could ever work it into his schedule. I’m glad I had a chance to tell him, once again, how much he meant to me. But I’m devastated to learn about how he was suffering. I had no idea and wish so much that I could have helped somehow.
I’m so grateful for your work. I’m sure it will save lives, and it’s such a beautiful tribute to Ben and other wonderful, remarkable souls like him.
thank you for this web site and page- we do need sanctuary in our healthcare system-
at the end of my career, I am now coming to terms with some of the trauma I endured in medical school –
these physician suicides are a marker for a system that needs healing.
back in the 90’s, a good friend, psychiatrist that I worked closely with, committed suicide – your website reminds me that us physicians are people, afflicted by the global scourge/epidemic of suicide
WOW. What an interesting and intense article. Akathisia is the culprit. Anxiety is terrible, so is depression. But akathisia was the worst thing I have ever experienced. These poor doctor’s need help. Thank you for your excellent write up.
I actually did know this person as unkind and not sweet. A certain job held may have led ppl. to think otherwise. Suicide is particularly a bad way to go out.
‘We lost’ —because State-licensed, State-privileged physicians belong to ‘us’.