Late last night I got this email: “Hello I am a nurse struggling with a medical error that may have led to a patient death and I need support.”
I texted her:
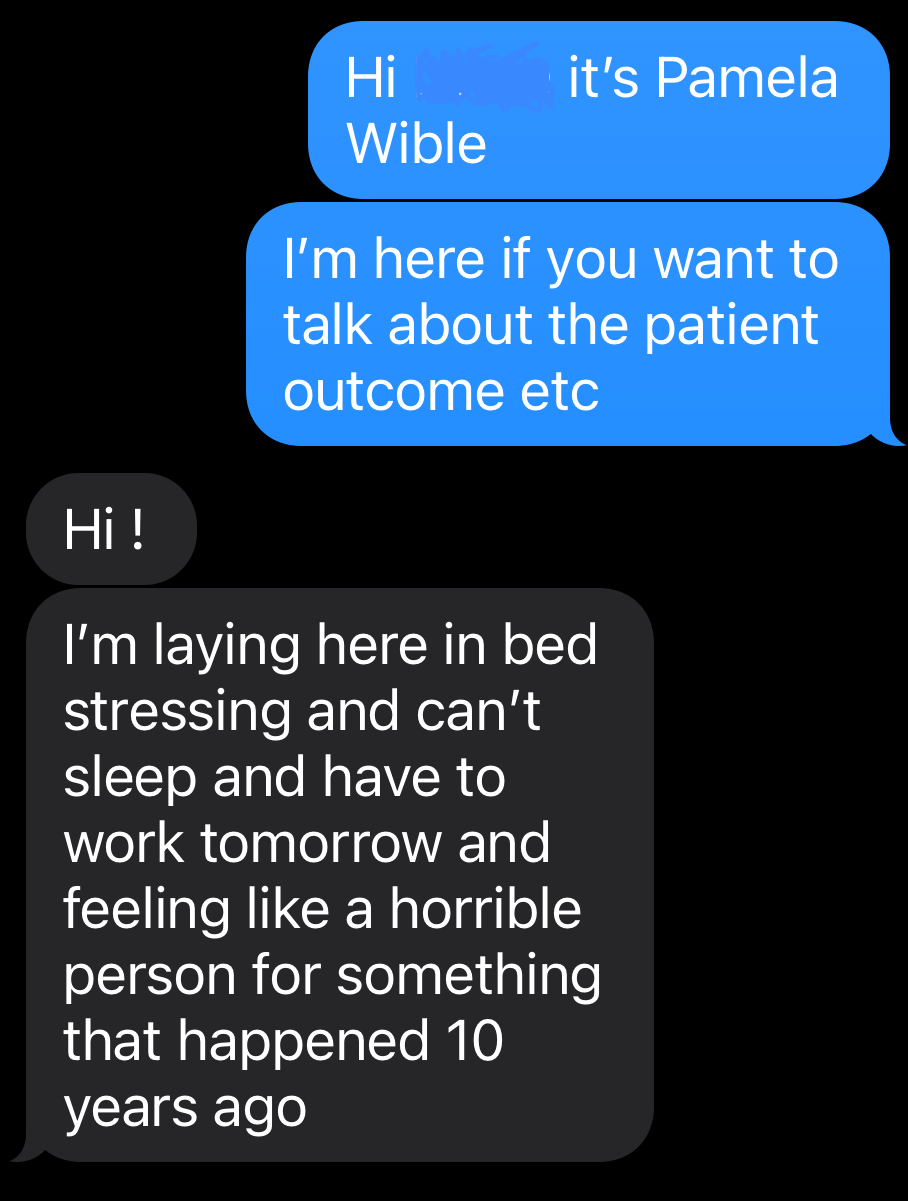
I called her just after midnight.
I asked how she found me. She said I was the only one offering support groups for medical mistakes. She gave me permission to publish this in hopes of helping others.
Three years into her nursing career working in a busy US urban hospital, she had just come on shift when one man who had been up in bed eating breakfast and speaking with her 30 minutes prior suddenly died. His code was a dramatic, gruesome scene.
Afterwards, the doctor told her she did nothing wrong. Yet ten years later she still blames herself for his death.
“Did I kill him?”
“Is it my fault?”
“Should I contact the hospital CEO?”
She still has so many questions.
Why?
All unexpected deaths require debriefing ideally within 24 hours.
Without peer support, we’re left in professional confusion and emotional isolation.
Knowing the cause of his death would have allowed her to (1) make sense of the situation; (2) learn how to help similar patients in the future; and (3) prevent a decade of intrusive thoughts.
This nurse needs closure.
Like a movie ending in a “cliffhanger,” the viewer leaves with unresolved questions. Without a sequel, viewers feel forever frustrated.
Suppressing feelings and sensations (subconsciously gnawing away at her) does not resolve suffering as buried memories continue to resurface.
Patient death PTSD happens when the visceral experience of witnessing a death is stored in your body. Sights, smells, and sensations take you back to the death scene instantly without warning.
Who is to blame?
Not the nurse.
Hazardous hospital conditions with understaffing lead to overwork, poor supervision, communication breakdown, and medical mistakes.
Unexpected patient deaths are not always caused by mistakes.
This nurse couldn’t have averted his death. She just happened be on shift as a witness.
Without a confirmed cause of death, perfectionists default into self-doubt, self-blame, and self-harm that may end in suicide.
Perfectionist people pleasers with savior complex often develop in childhood as parentified children trying to help parents with health issues. As a child, this nurse desperately tried to help her parents’ mental health issues. Her career motivation began with the desire to save her loved ones. Being unable to save this patient may trigger her deep-seated pain of being unable to save her parents as a child.
On a spiritual note . . .
Survivors of near-death-experiences report a state of bliss on the other side. Most don’t want to return to the pain of human life. So this man is now a free spirit.
“The most generous thing you can do now is to allow him to be free by not using him to punish yourself.”
“Doesn’t he want revenge?” she asked.
“No. He wants you to be free of your suffering.”
We spoke for one hour and 25 minutes.
By the end of our call, she felt she could finally sleep.
After ten years of dark thoughts, she can now rest in peace—without dying.