NOTE: Article updated 10/7/22 to reflect my newfound experiences with traumatized physicians.
I recently spoke with an emergency doc at a busy understaffed hospital. He had just dealt with a mass shooting and is now in the midst of a divorce. Clearly distressed, he wants to retire. Here’s the shocker: He told me that he did NOT feel traumatized.
Physicians are suffering with PTSD. Whether we want to admit it or not, many of us developed medical student PTSD. Even premedical students at the very earliest stages in their careers may be carrying childhood trauma and a hidden diagnosis of PTSD.
Physicians who save lives are losing their own to untreated trauma.
Shells of their former selves, most doctors are unable to relax or feel joy. Trapped in assembly-line medicine—immersed in misery and suffering—doctors are often disconnected from their bodies, their hopes and dreams—their own humanity.
I’m Dr. Pamela Wible and I run a doctor suicide helpline. I’ve spoken to thousands of suicidal doctors. Most have PTSD.
What’s the solution to physician PTSD?
First, state the obvious—tell the truth. Stop denying that doctors have PTSD. Let’s not blame physicians for occupationally induced mental health conditions.
You received no informed consent of the mental health impacts of a medical career. You are not to blame.
We have an epidemic of doctor suicide and physician PTSD. “Burnout” covers up the real violations to our humanity in medical education and practice. Burnout is a victim-blaming and shaming term that does not address the true reason doctors are suffering.
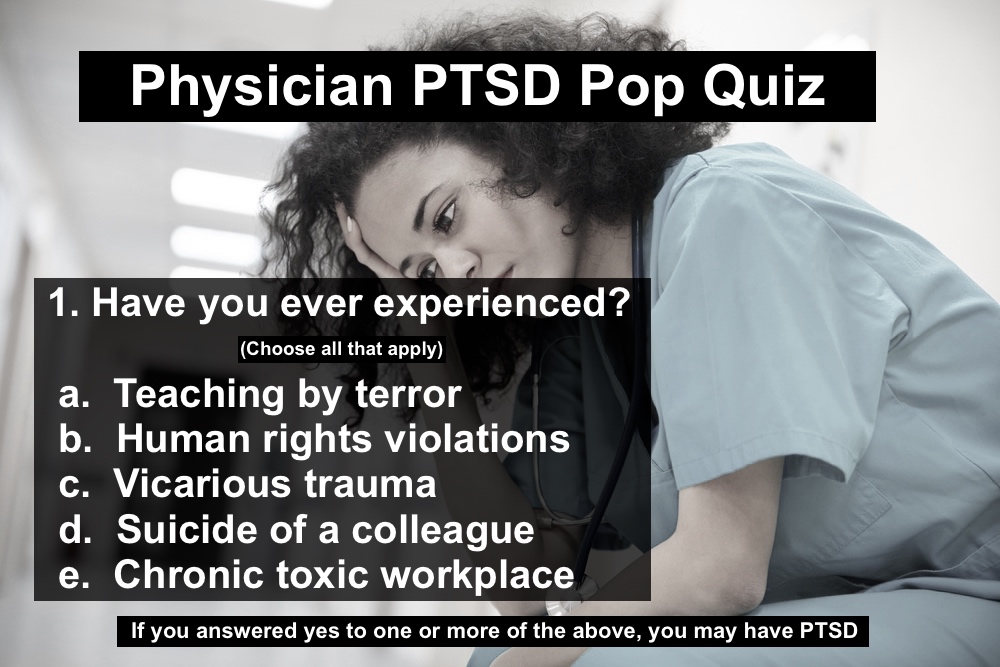
Top five things that lead to physician PTSD
1. MEDICAL TRAINING
We have a fear-driven medical education model that teaches us by terror. A retired surgical subspecialist wrote me:
“I was happy, secure and mostly unafraid until med school. I recall in vivid detail the first orientation day. Our anatomy professor stood before an auditorium filled with 125 eager, nervous, idealistic would-be healers and said these words. ‘If you decide to commit suicide, do it right so you do not become a burden to society.’ He then described in anatomical detail how to commit suicide. I have often wondered how many auditoriums full of new students heard these words from him. I am sure someone stood in front of us and told us what a wonderful and rewarding profession we had chosen. I do not remember those words, but I do remember how to successfully commit suicide with a gun.”
She goes on to share her first panic attack and how the trauma from her medical school orientation remains with her—even in retirement!
“One month later on the eve of our first monthly round of six exams in one day, I had my first full-blown panic attack. I had no idea what was happening. I thought I was losing my mind. I took a leave of absence and made up excuses. I returned untreated with maladaptive compulsive behavior, completed med school and survived the public pimp sessions and all the rest. No one ever suggested that the process was brutal or the responsibility frightening and no one offered us help. I have maintained contact with only one colleague from med school so I do not know how the others fared.”
Teaching by terror is common in medical school. Terrorized students suffer in isolation with chronic hypervigilance—even full-blown panic attacks. No wonder she felt like she was losing her mind.
Reacting vs. Responding to Trauma
When we are stressed and under the influence of high adrenaline—in a fight-or-flight state—we lose ability to respond in a thoughtful and calm manner. Medical trainees and physicians are often in chronic high reactivity states and can be easily triggered by traumatized patients.
All physicians suffer from intergenerational trauma (mostly untreated and even unrecognized). Traumatized doctors pass on their unresolved trauma to new trainees through emotional violence such as bullying.
Our attendings—mistreated themselves during training—without the teaching skills or mental health care that they required—simply pass on their pain to the next generation, as this surgeon reports:
“I began my residency in California and during that time was very depressed, abused within my training program. My depression impacted my performance and I was eventually fired. I was lucky enough to find another position and continue my training, however, some days I feel my depression and despair returning primarily when I feel my career has been irreparably damaged by my departure from my first residency program. Those feelings were initially tied to hazing and bullying that are an integral part of the educational program there.”
Many times we feel that if we can leave the trauma behind geographically (by moving to a new hospital, residency, state), we will suddenly be better. Yet our trauma follows us for a lifetime as the above surgeon shares:
“Sometimes, I can still hear those attendings in my head saying things like, ‘Watching you operate is like watching a retarded monkey.’ Or, ‘Do they ever teach anatomy at your medical school? Our students know more than you.’ It’s paralyzing. I am reaching out to you for two reasons. I’m interested in eradicating the abuse in medical education. I’d like to have a career in academics and to influence policy regarding the treatment of trainees. More importantly, can you help me make the flashbacks stop? Can you help me not worry so much about my future? Can you help me with my depression related to my change in career trajectory?”
To help with flashbacks—a sign of full-blown physician PTSD—we must revisit the original place of our trauma and move from reactivity to responsiveness. Here are 5 tips for disrupting the trauma cycle.
2. HUMAN RIGHTS VIOLATIONS
Violations to our humanity are sadly commonplace in medicine: Hazing, bullying, racism, sexism—women belittled and told they should have gone into social work instead of neurosurgery because they cried after the death of a patient. Sleep deprivation—a torture technique used in war—can even cause seizures, hallucination, and psychosis in medical trainees. One doctor reports:
“I had married the year before residency, and for the first two years, I was either at work or asleep, so I didn’t see my wife. It was the start of the erosion of the relationship that led to divorce years later. I also suffered permanent health problems, some extreme sleep deprivation. Prior to residency, I slept fine eight hours a night and had regular bowel movements. Since my internship, I developed lifelong severe insomnia and went for decades on four to five hours of sleep per night as well as severe constipation using the toilet about every five days.”
A psychiatry intern told me she had only seen her newborn for six waking hours during the first six months of her residency. Children of physicians may be neglected—and maternal deprivation may cause lifelong problems in kids.
I know several medical students who had psychotic breaks due to sleep deprivation. Some docs work more than 100 hours per week. Two physicians explain their experiences:
“I did my internship in internal medicine and residency in neurology before laws existed to regulate resident hours, which are sadly not enforced and these people are then told to lie on their timecards. The law doesn’t necessarily help. My first two years were extremely brutal working a 110 to 120 hours per week.”
“I got to witness colleagues collapse unconscious in the hallway during rounds and I recall once falling asleep in the bed of an elderly comatose woman while trying to start an IV on her in the wee hours of the morning.”
These stories are not uncommon.
We cease to behave as humans when we’re treated with such inhumanity. We go numb. Disconnected to our own bodies, we objectify ourselves and others. We don’t notice when we’re hungry or sleepy or have to pee or need to cry. Physicians have told me they’ve lost the ability to cry.
The solution to human rights violations is not another burnout book or a resiliency module. In this survival guide, I outline the top 40 human rights violations in medical training (and practice)—with solutions.
3. VICARIOUS TRAUMA
All of us—especially surgeons, emergency docs, obstetricians, neonatologists—have experienced vicarious trauma. A neonatology fellow recently called me wondering if it was normal for her to have panic attacks and start crying in the middle of the her shift. I asked her what she’s doing at work. Well she’s flying around in a helicopter, picking up half-dead babies, preemies all over the county—and is the only one responsible at night for 40+ high-acuity NICU patients.
In that scenario, she is experiencing emotional flooding. She’s overwhelmed by her work hours, caring for way too many patients, all very sick—a set up for a medical mistake. She may be losing connection with her own body and in this state she is flooded by grief, sorrow, fear, and phobia. In a reactive mindset, she may even transiently lose some cognition and be unable to recall proper dosing. Amid a panic attack she may falter when intubating or inserting a central line.
When we dissociate, we are no longer in the present moment. We are performing suboptimally and are at risk of harming a patient—or ourselves. We may be accused of patient abandonment if we run to the bathroom or need to take a break to recover. Some doctors may need to take a leave of absence and get intensive treatment. Many fear license repercussions if they ask for help. Here are 13 tips for confidential mental health help.
Physicians should be alert to sensations of stress, tachycardia, feeling faint. You may even feel “shocky.” Ask yourself, “Can I feel my body? Am I in a cold sweat? Do I feel triggered?”
Notice if you are numb or so flooded by such strong emotions all you can feel is a desire to fight or flee.
I just spoke to an emergency doctor—a new residency grad. Highly skilled, she works in level one trauma centers with the highest acuity emergency cases because she doesn’t want to lose her hard-earned skills.
In the aftermath of fatal car accidents, she’s had to work on so many mangled patients that she is unable to drive a car herself without having panic attacks. Last year she spent more than $13,000 on Uber rides.
Both women docs above have occupationally-induced PTSD from vicarious trauma—and there’s no easy way to get 100% guaranteed confidential help. Where would they go? If they asked for help, they risk referral to a punitive Physician Health Program (PHP). They both felt they could not go to a psychiatrist—without fear of career repercussions.
So when a doctor is crying on the phone with me at midnight wondering what to do next, here’s what I say: You’re normal. You are having a normal reaction to trauma. You are having panic attacks. You are human. You are still a good doctor. You just need safe, confidential help to heal.
If you are a doctor and you have found yourself hiding in your car or in a bathroom stall at your hospital just shaking, crying, feeling totally out of control, feeling panic and impending doom, and you don’t know what to do next—you have been traumatized. You can heal. Read best tips to disrupt the cycle of physician PTSD.
In both these cases—the neonatologist and emergency doc—women in their mid 30s who have their eggs frozen—they haven’t been able to date, yet still want to have families of their own. How can one date when flooded with scenes of dead preemies and mangled car accident victims?
4. DOCTOR SUICIDES
Most physicians have lost a colleague by suicide. Nearly all of us have not been able to properly grieve these doctor suicides. We are going back to work each day feeling at risk ourselves.
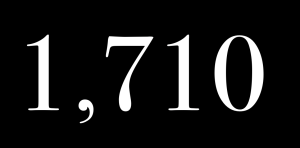
Doctors have the highest suicide rate of any profession. In the aftermath of a doctor suicide, we have no time to grieve. We have to get back to work.
Here’s what I learned from investigating 757 doctor suicides.
Anesthesiologists have the highest risk of suicide among all physicians. Anesthesiologists who die by suicide may be found dead in hospital call rooms and closets. Google “doctor found dead in hospital.” You will probably discover a male anesthesiologist. Here’s a letter I received:
“In anesthesiology, it seems we have a higher percentage of death by suicide than other medical specialties. My colleague took his own life over a year ago. I was basically okay until then, but it’s how everyone reacted that really got to me, the show must go on. We diverted patients the first night probably because the ER had to see Joe when he came in. The next day, all of us were back at work in the operating room. There was no time to grieve and we and the department were so stunned. We didn’t know what we needed and what to ask for. It felt like abuse not to honor him or his colleagues with some rescheduling of operations. I will never be the same. I no longer see medicine as a force for good. It seems like it is a way for other people to make money off our talent, intelligence, education or determination. He was my friend.”
Without suicide postvention, grief-stricken doctors can misdirect and displace their anger and sadness. Abandoned by the suicide victim, by administration, by our peers who head back to work—we live with survivor guilt and confusion—and very likely our own passive suicidal fantasies to escape the horror of our pain.
Doctors develop (and hide) these maladaptive coping behaviors—drinking, taking excess prescriptions (or illicit) drugs, smoking marijuana, having affairs, and the list goes on . . .
Suicide secrecy just perpetuates the pain—and isolation.
Hospital administration will often blame the victim, label the dead doctor as mentally ill to cover the whole thing up. To clamp down any conversation or investigation of the suicide, institutions threaten grieving colleagues with professional reprimand, forced psychiatric referrals, or termination.
5. HAZARDOUS WORKING CONDITIONS
Chronically underappreciated and overworked, physicians feel trapped in assembly-line medicine—in big-box clinics forced to see patients every seven minutes.
How do you know if you’re in a toxic workplace? You experience an excessive amount of control—control of processes, of people, of time. You notice a lack of communication. People aren’t talking to each other. When they do talk, they are passive aggressive (as a reaction to being over-controlled). People isolate, withdraw, stonewall. Finally, communication stops altogether.
Without open communication, you can’t provide safe medical care. You may feel angry with a coworker. Any outburst and you risk being written up as a disruptive doctor, an unprofessional physician—terms that have been weaponized against doctors who may be reported to the medical board—even when advocating for patient safety!
No matter how beautiful your house, what a great car you drive, you will continue to suffer from a chronic toxic workplace or physician PTSD—unless you make a change.
Nonphysicians may say, “What do you have to be complaining about? You’re a doctor!” Having your feelings dismissed or minimized is not helpful.
If you’ve suffered from any of these five common pathways to physician PTSD—you absolutely need to talk to somebody so you won’t internalize your pain.
When you internalize your pain, you feel like something is wrong with you. When you look around others appear to be okay—even happy. You start to believe you are the problem.
You are having a normal reaction to an occupation that has violated your humanity. If you find yourself in a chronically toxic workplace, please know it is not your fault. You can heal. You have options.
It is not too late. You are not too damaged. You can heal from your trauma—and you can begin to actually experience what it’s like to be human.
I was once a suicidal doctor. I’ve had PTSD (even before medical school). I almost gave up my career—and my life. I know how it feels to be terribly misunderstood, lonely, isolated, traumatized—and at your wit’s end.

The #1 reason doctors don’t reach out for help is fear of being reported. Please know that in ten years of running a free doctor suicide helpline, I have never reported a doctor to anyone. I’ve never turned a doctor over to the board, law enforcement, a PHP, or another entity. I don’t type what you tell me in an EMR. I’m just like you. I’m a peer who gets it because I’ve been through hell and back myself.
You can definitely bounce back—even after having an addiction, diverting drugs, or having a suspended license. I just got off the phone with a doctor who is healing after a felony for insurance fraud. I’ve heard it all. I still have empathy & tons of resources to share. As long as you are breathing, it’s never too late to heal.
All quotes published with permission, many in Physician Suicide Letters—Answered, available as a free audiobook.










Thank you for a (very) thorough overview of this dilemma facing physicians and our health care delivery systems collectively—PTSD & depression, sprouting to a large extent from an abusive medical system—whether in the US, Canada, UK, Europe or Australia.
In essence, we are caught up in this broken reality of (what a misnomer) “healthcare” due to the fact we (MDs, Licensing bodies, HMOs, Hospitals, Health Authorities, Health ministries etc) have long discontinued practicing ETHICAL MEDICINE.
We don’t even teach ethical medicine.
Oh, we talk about it. It sounds nice and honorable.
Medicine has become a business.
I’m not talking about getting paid at the end of each month.
Chemotherapy, to name but one is a MULTIBILLION dollar business & industry.
Also, we don’t provide “healthcare,” we provide “sick care.”
I have two requests.
1. Can you make a shorter version of this article? More people will read it.
2. How do we “FIX” the problem?
For many of us, due to the nature of our training & practice, cannot step away on our own and practice independently. (e.g Anesthesiologists)
But, I will keep spreading the word, and keep practicing ETHICAL medicine.
Thanks for sharing
So much to say. Had some trouble keeping this long overdue conversation short. Will try to be more concise in the future. Really will! 🙂
Thank you for your efforts in addressing this issue.
It takes COURAGE to humble oneself and ask for help.
The person who reaches out for and receives help becomes a stronger and more authentic caregiver.
This is the message we need to hear to further remove the stigma of seeing a therapist or attending a support group.
I would rather be cared for by physicians or nurses/other ancillary medical personnel who have received help with their own struggles in life then someone who tries to manage it alone.
I have found it very helpful ti listen to the Trauma series offered often by NICBM.
The Webinars, given by world renown leaders in the field of psychology/psychiatry have given me a wealth of information on PTSD…the bidy’s response to Trauma and how to recognize its affects and better manage the affects of Trauma (which includes vicarious Trauma and bullying). It was very helpful, both for my patients and for myself. ( CEUs are offered.)
The contact person for these excellent offerings is Ruth Buczynski.
I will never regret “seeking help”.
Dear Dr. Wible,
Thank you so much for your writing.
I was raised by people who are very in touch with their feelings so I have weathered medical education well. I developed rituals when I get home to shake off the stresses of the day. I am so compartmentalized that it borders on multiple personality disorder! I read your articles with sympathy but feel bad speaking up as I have never been subject to much of the maltreatment you describe. On the contrary, most of the people I am around on a daily basis are an inspiration! But the system is malignant and toxic, and I didn’t realize how badly I was affected until I was staring at your Physician PTSD Pop Quiz and crying on a rare day off.
A. Teaching by terror – YES and even when I think they mean well. Maybe I have Stockholm Syndrome but… I don’t think anyone wants it to be this way. However, I’ve seen students and residents harshly disciplined for minor issues, so I am a silent little mouse and terrified to accidentally step out of line. I have panic attacks about it. I have seen people mocked for asking for minor accommodations that honestly affect no one, so I would never dare. In my first week of medical school, I was randomly assigned to an anatomy cadaver that died of the same rare disease as one of my parents. I was afraid to ask to be moved as my professors so emphasized that being tough is part of being a good physician. I stared at the physical effects of this disease from the inside out for months and had nightmares about my dead, naked parent on that table for a year afterward. Somehow that is nothing much compared to the daily trauma of being given conflicting instructions and being terrified I will get in trouble no matter what I do. After all, it wouldn’t be the first time.
B. Human rights violations – Due to a large emergency expense, I couldn’t afford to buy food at the hospital on an inpatient internal medicine rotation. I also was given no place to store anything so I would fill my pockets with dollar store granola bars and pray they kept my stomach from growling. One day I forgot them and got so hungry after a long day that I “stole” cold leftover rice from a meal left for attendings in the physician’s lounge. I was so afraid I would be caught and have to explain. I lost almost ten pounds off an already small frame during that rotation.
C. Vicarious trauma – In many ways this is unavoidable, just the nature of medicine, but I wish we had a space where we could show our feelings to others. No one outside the field can understand but no one inside the field wants to debrief. Or perhaps they do and we are all just afraid to ask each other.
D. Suicide of a colleague – a physician near me killed themself recently and it was hushed up. People are uncomfortable if you even mention them. We weren’t close but it’s a lot to process.
E. Chronic toxic workplace – So many examples but this one still bothers me: I had a preceptor in medical school who pressured me to pray with him. We are not the same religion. When I finally told him I was not the same religion, he gave me a written testimony of how his religion saved him from a sex addiction. With a LOT of details that made it very difficult to work with him. It was brought up repeatedly for the rest of my rotation. Even worse, he also made fun of transgender people in front of me, laughed with his staff at a patient and made derogatory statements. I cried angry tears on the way home that day and felt ashamed that I didn’t speak up for what is right. What is wrong with me? Why didn’t I stand up for that patient? I still am so angry at myself because I should have done what was right. My patients need people like me to be good allies and I failed. I was even afraid to tell my school or complain, as I didn’t want my grade or transcript affected.
I don’t know when a strong outspoken woman became such a coward. I revised this email repeatedly to remove identifying information even though that means leaving out the real horrors. I made a dummy email so you won’t know my school and residency because I am just too afraid. No one can ever know any of this. I might get in trouble. I might be viewed as a troublemaker or unprofessional. I feel guilty when I have done no wrong. That’s the most malignant part of this system, being shamed into silence.
Anyway, thank you. I am a believer in the occasional good cry and I needed this one. We’ll make it better together, and this is the first step.
Wow. I’m so glad you made it through the podcast & blog and that you found it so therapeutic. We all need a good cry in medicine. Please do reach out to me anytime (confidentially here): https://www.idealmedicalcare.org/blog/contact/ and I would be very happy to talk to you.
You are NOT a coward. You are very wisely self-protecting during the last leg of your journey in residency. I’m sorry you are afraid and I understand that you need to do what you can to stay safe. It is important that you allow yourself the secret place deep inside where you know the truth about yourself and your situation. Guard that place. Remind yourself daily that you are doing what you need to to reach the end goal. Someday soon you will be free to practice medicine the way you see fit and Pamela and I will still be here to help you realize that dream. Thank you for writing.
Way too long to read it all.
Remember that the body of knowledge turns over every 10 years. Education must keep up. Take no longer than two years to teach the basics in medicine, and then show different pathways to be taken by those who so desire.
Yep Jacob. Modern teaching method needed. We don’t have to terrorize the gifted to help them learn. Counterproductive. Learning should be a joy if done properly.
Thank you very much for the wealth of information which provides some insight into the unfortunate event which has directly or indirectly touched the lives of many of us.
Apart from the suicides, significant psychological issues are frequent among medicos.
One aspect from personal experience is that the field of medicine is so competitive, we spend every spare minute in our life from school age getting into medical college & after that enhancing our career prospects in a super-competitive field, with the resultant lack of time for socialisation which is the distraction/relief we all need to keep sane/balanced. As a result we have limited coping mechanisms when things go wrong. It happens to all humans, however, we the ill-prepared lot can not deal with them properly i.e. there is lack of resilience. Also because a majority of medicos are high achievers, they handle the imperfections of life less well than general population.
Somehow we need to make ourselves more resilient.
It’s not about being more resilient. We must be more resistant to abuse. https://www.idealmedicalcare.org/blog/tired-after-200-patients-you-need-resiliency-training/
Could not agree more about resisting abuse. In fact, we should prevent abuse in the first place.
Hello Dr. Wible; I just wanted to say that I experienced the same thing in my pathology residency in Puerto Rico. My confidence as a physician hasn’t been great since I have struggled with the USMLE’s. I’ve had multiple retakes and I thought that I would never be accepted in a pathology residency program until I was finally called. It has been my dream to become a pathologist ever since I started to do research in medical school and I have experience as a lab tech and a research director in a private pathology lab. I thought that I would be able to make it but it all came crashing down on my first year. I was constantly screamed that by my attendings for not remembering the basics of med school, I was constantly treated as a dumb and belittled because I didn’t receive any lectures to actually help me know what I was looking at through the microscope. When I got my diagnosis right I was questioned if those answers were provided by myself or I asked a senior resident for the answers which made me feel even more incompetent and dumb. I was prohibited to ask or express any questions or doubts concerning cases to my senior residents. I was asked to lie on autopsy reports to protect surgeons from malpractice lawsuits (which I didn’t), and all of that caused me to fall into major depression, have constant panic attacks, an intervention from my husband and my mother to get help, which resulted in a medical leave to be able to study for step 3 out of this environment (I’ve failed 2 times since being in the residency) and ending with me quitting before they fired me because the program director began to spread lies about me being disrespectful to her because I wasn’t going to lie in the reports and because she was also trying to make me lie on my ACGME survey about the program and I didn’t. Right now I am being medicated for my depression and seeing my doctor once a month. Still I haven’t been able to shake away the fear that once I apply again for another program, the program director will destroy me in the letter of recommendation that I need to apply for another program and I tend to have nightmares about it. I’ve been working at the pathology lab I used to work at and I am also studying once again for step 3, but my morale and confidence are completely shut down and I feel like I am not good enough for any pathology program. I never thought that I would start losing the love and passion I have for pathology to the point that if I only think about working on an autopsy or working on the biopsy I become anxious. Thank you for letting me know I am not alone and that there is hope to overcome this.
I’ll email you now. I have some great ideas for you Alexandra.
Analysis of remorse
One of the devastating news to a cardiologist is reading the obituary or hearing of the demise of a patient who had been to his clinic a few days or weeks earlier for a medical consultation during which he had reassured him. The impact of the news could be tremendously reduced should he further hear that the said patient had died in a car or swimming accident, only to rise again to previous levels when the coroner’s report states that the victim had had a cardiac arrest just before the accident.
So it is not what has happened to the patient that upsets his cardiologist but the way it has happened!
Boghos L. Artinian MD