
Dear Leigh,
Within days of your suicide, your friends reached out to me for help in sharing the truth of your life—and death. Then came this letter from your aunt:
My niece is a physician who died by suicide on 4/14/20 from a self-inflicted gunshot wound. She mentioned in her suicide note that we contact you & gave permission to pass her information on to you as you are the leading authority on physician suicide.
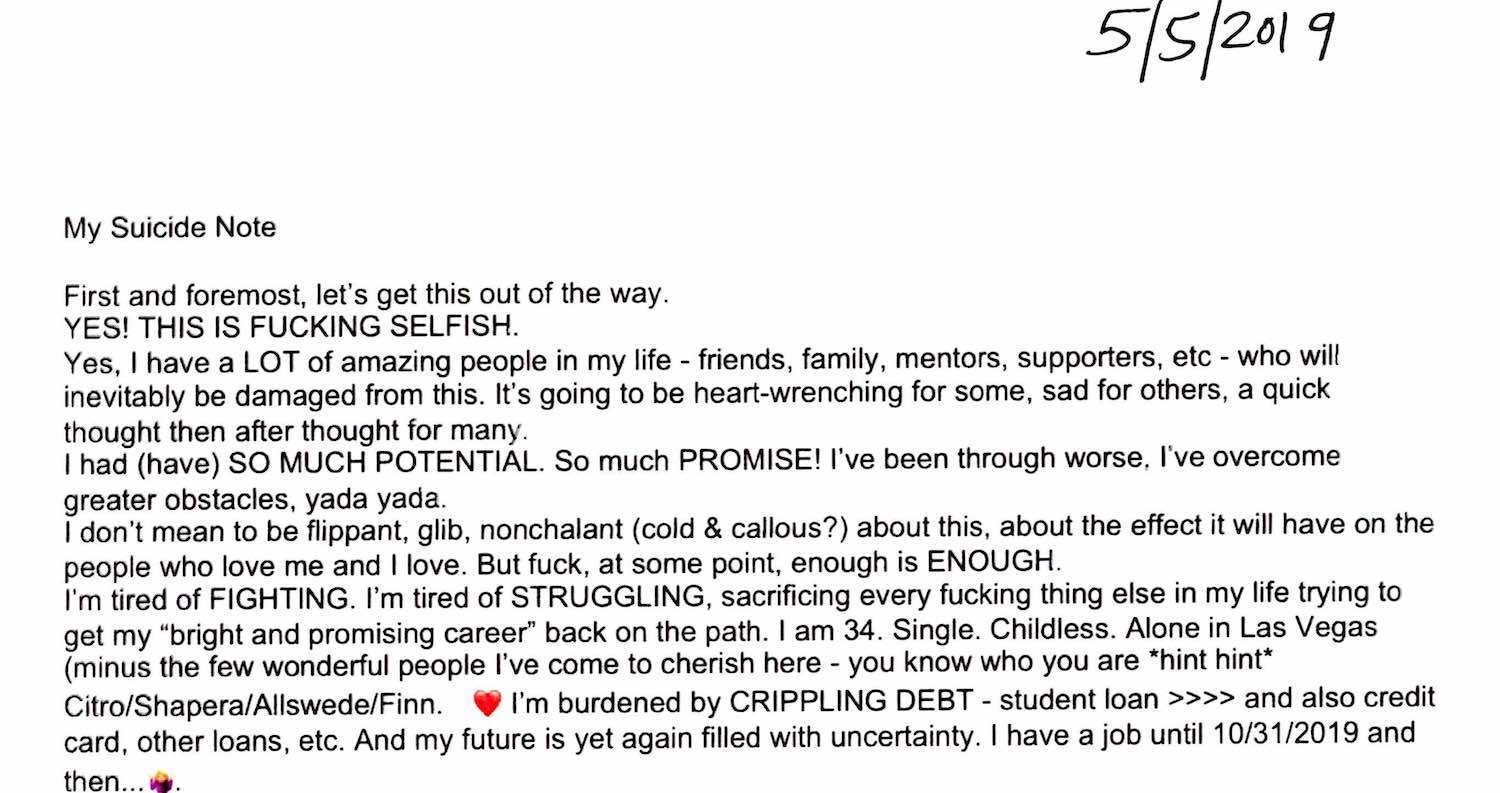
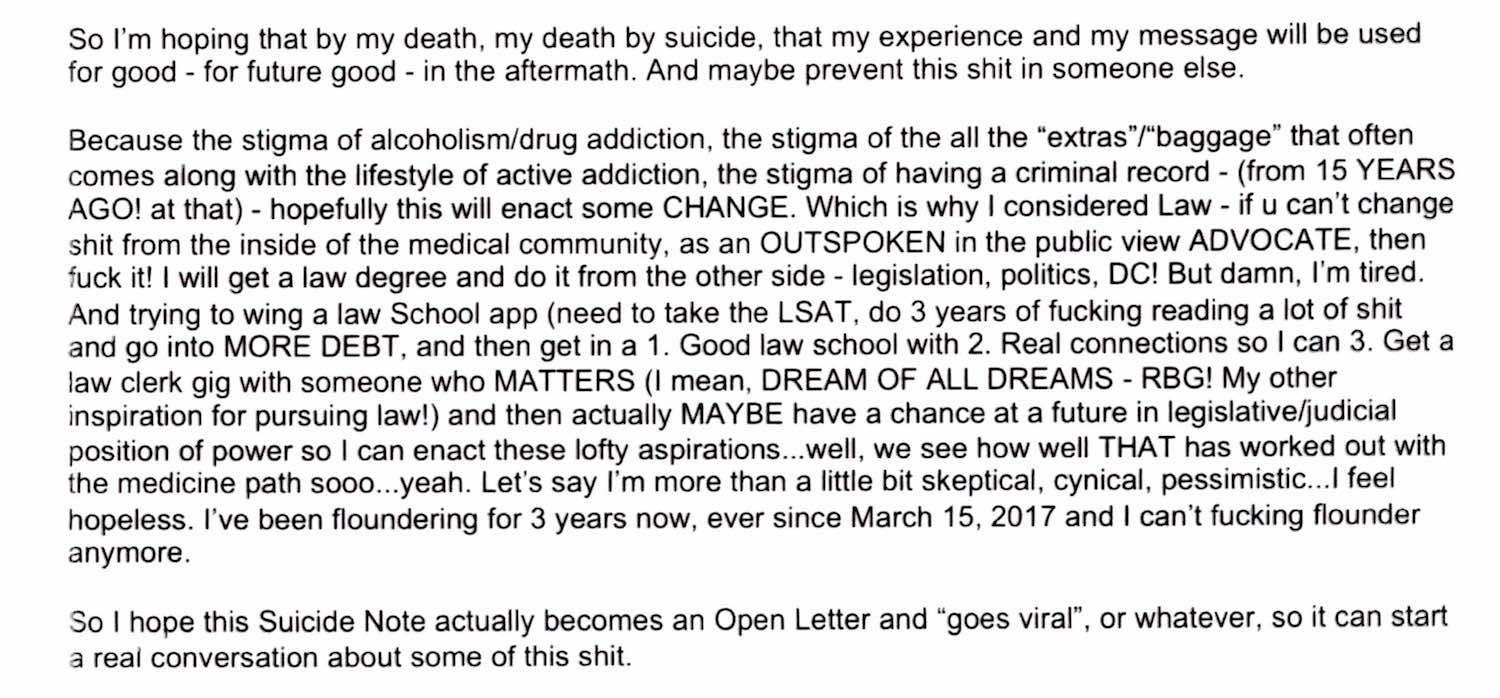
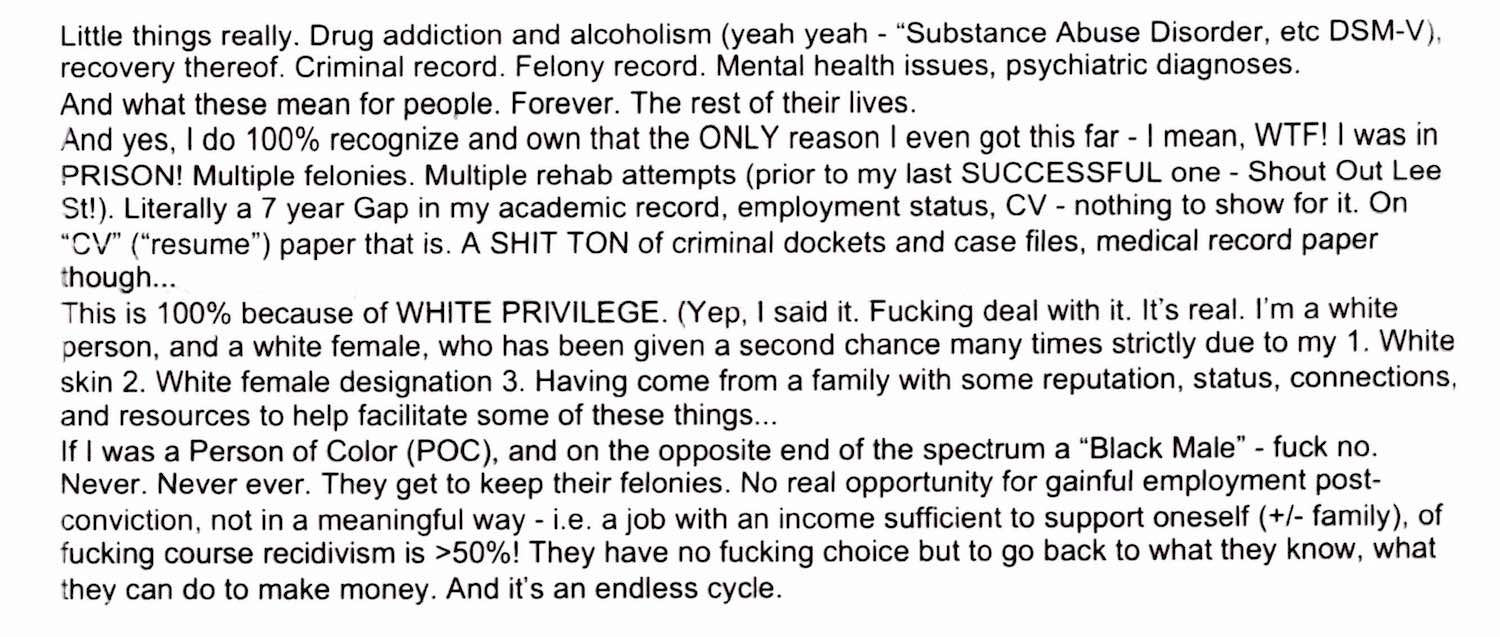
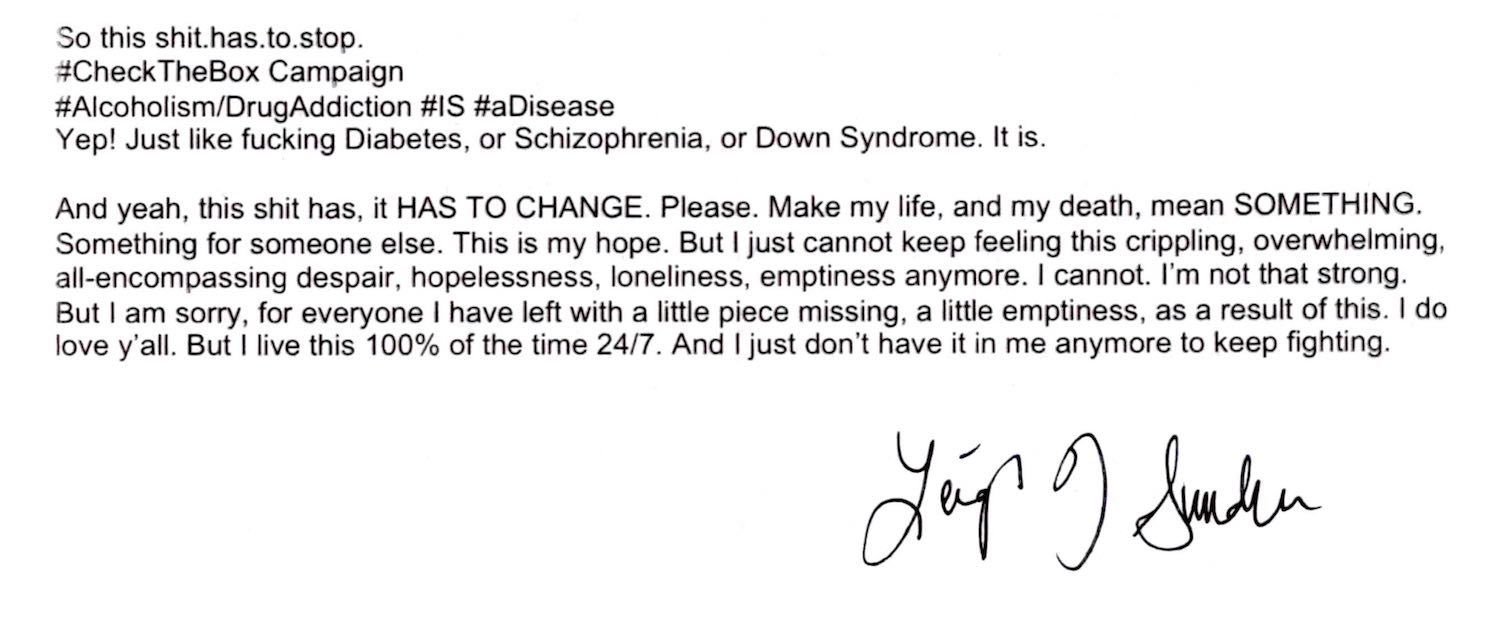
I’ve spoken to your aunt almost daily. Then your mom and dad. I’ve read your suicide note(s)—the original and all 3 addenda—multiple times. In your final request you stated:
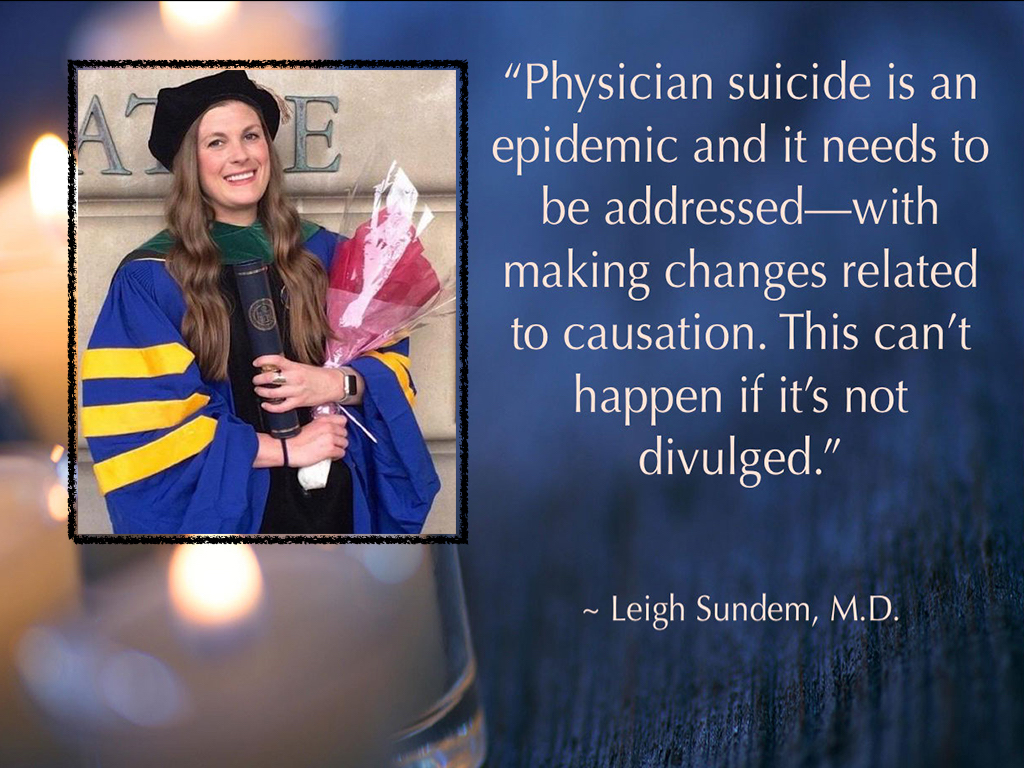
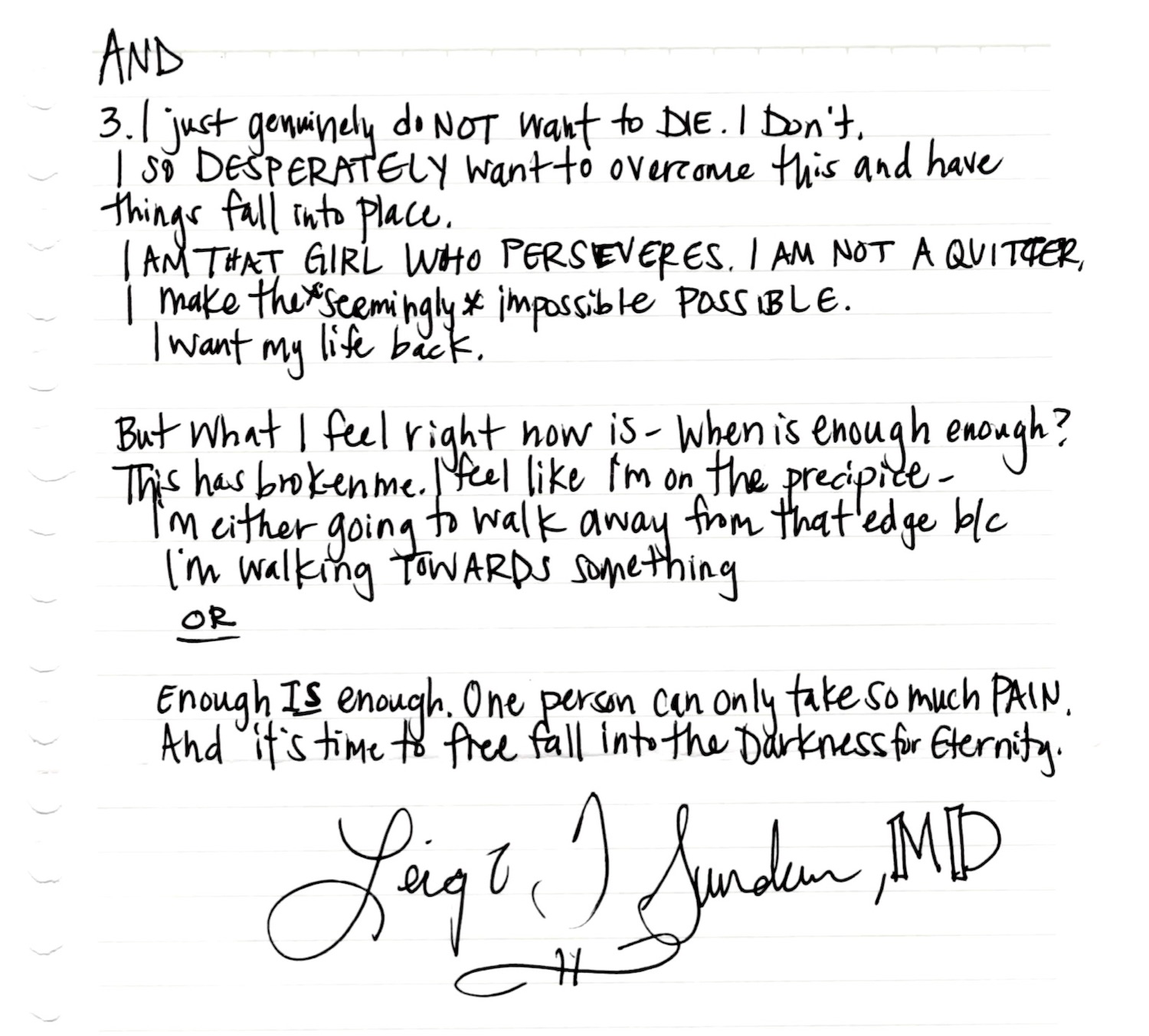
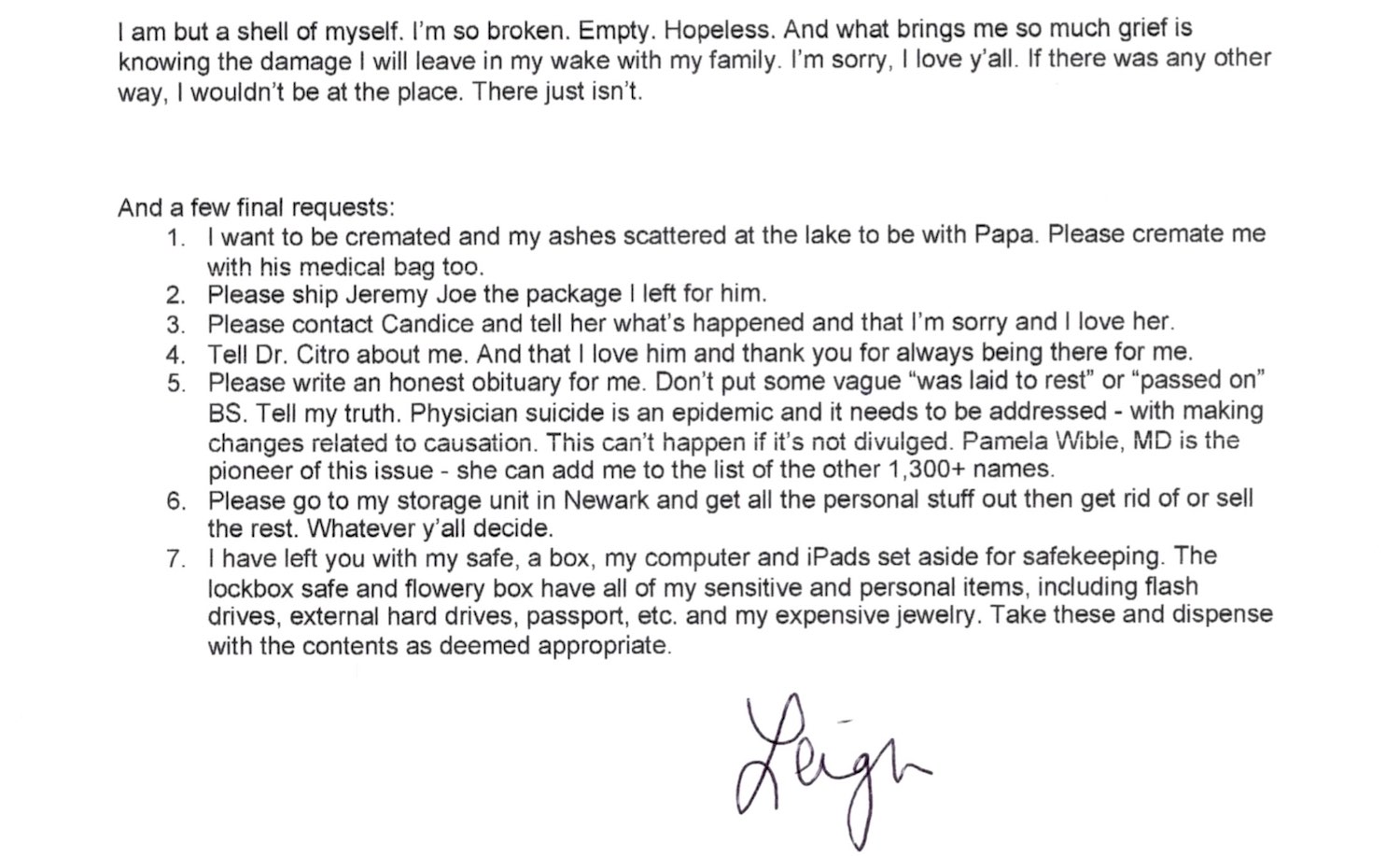
Please write an honest obituary for me. Don’t put some vague ‘was laid to rest’ or ‘passed on’ BS. Tell my truth. Physician suicide is an epidemic and it needs to be addressed—with making changes related to causation. This can’t happen if it’s not divulged. Pamela Wible, MD, is the pioneer of this issue—she can add me to the list of 1,300+ names.
You are a truthspeaker. I admire that. Censorship won’t prevent physician suicide nor will it end the stigma and discrimination within medicine that fueled your decision to end your life. I so wish you had reached out to me earlier. I would have loved to help you see how you could practice medicine—even launch your own nonprofit clinic in South Carolina this summer (maybe to serve patients in recovery—your lifelong passion).
But I never heard from you—until after your death.
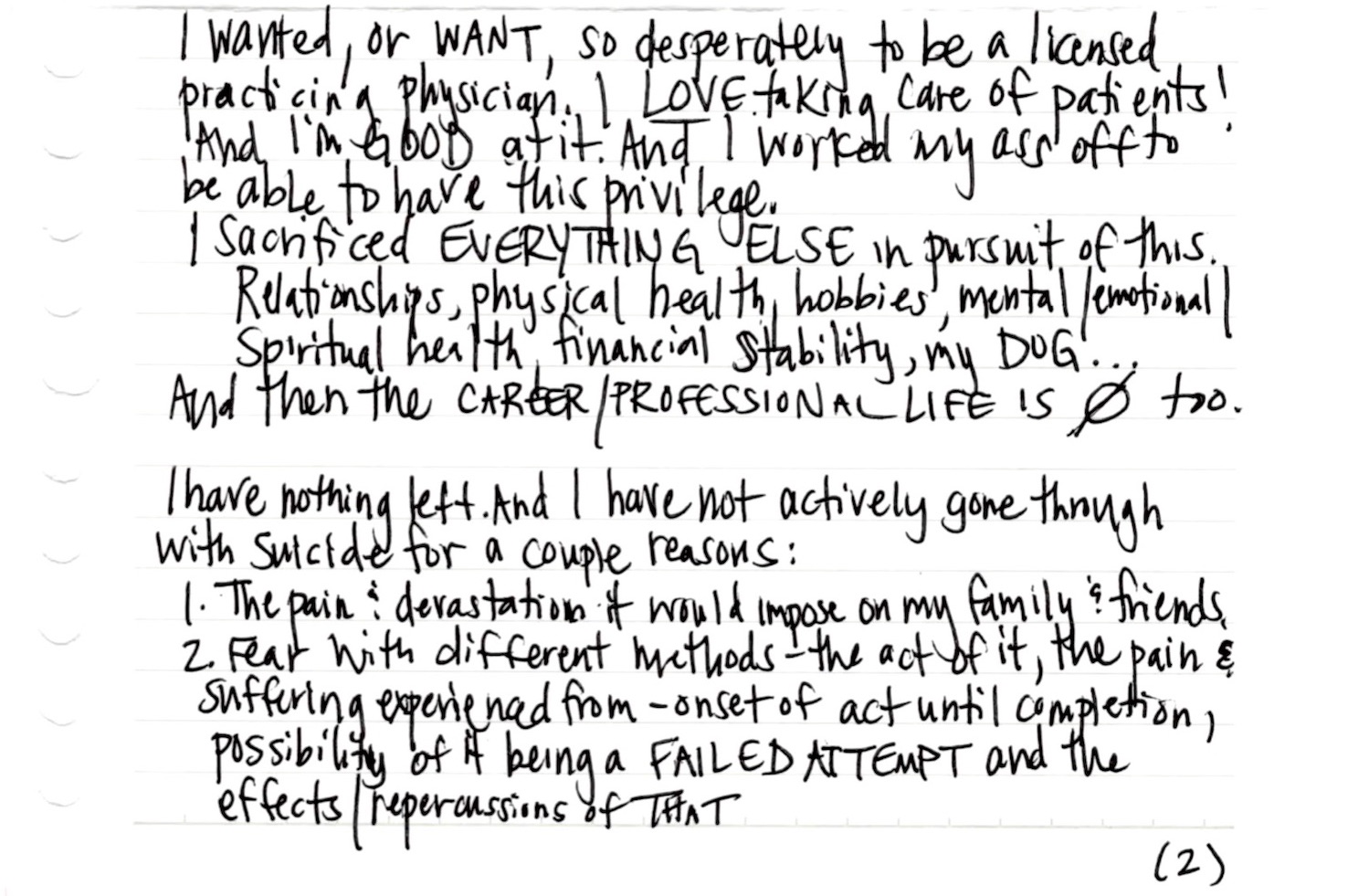
So now I’m following the instructions you’ve left for us by publishing your suicide note on the one-month anniversary of your death (with permission from your family). My loyalty is to you. To amplify your voice, to share your words so we may learn from your experiences. You’ve asked that your original note “go viral” to start a real conversation about why you died so your death can prevent others from suffering the same fate. I agree with your philosophy. To prevent doctor suicides, we must analyze the causes clearly identified in doctors’ suicide notes. Years ago I published Physician Suicide Letters—Answered (free audiobook here) to break the silence, shame, and stigma of our doctor suicide crisis. We must take action based on the root cause analysis of each suicide—to prevent the loss of any more doctors. You are 100% correct.
I’ll address all of the issues you raise in your notes at the end—with actionable solutions for those who are still suffering.
(For readers like me who never had the opportunity to meet Dr. Leigh Sundem while she was alive, please read the beautiful tribute to her life and spirit on her GoFundMe page where you may support the Leigh Sundem Memorial Scholarship Fund)
Read rest of the Suicide Notes below. . .
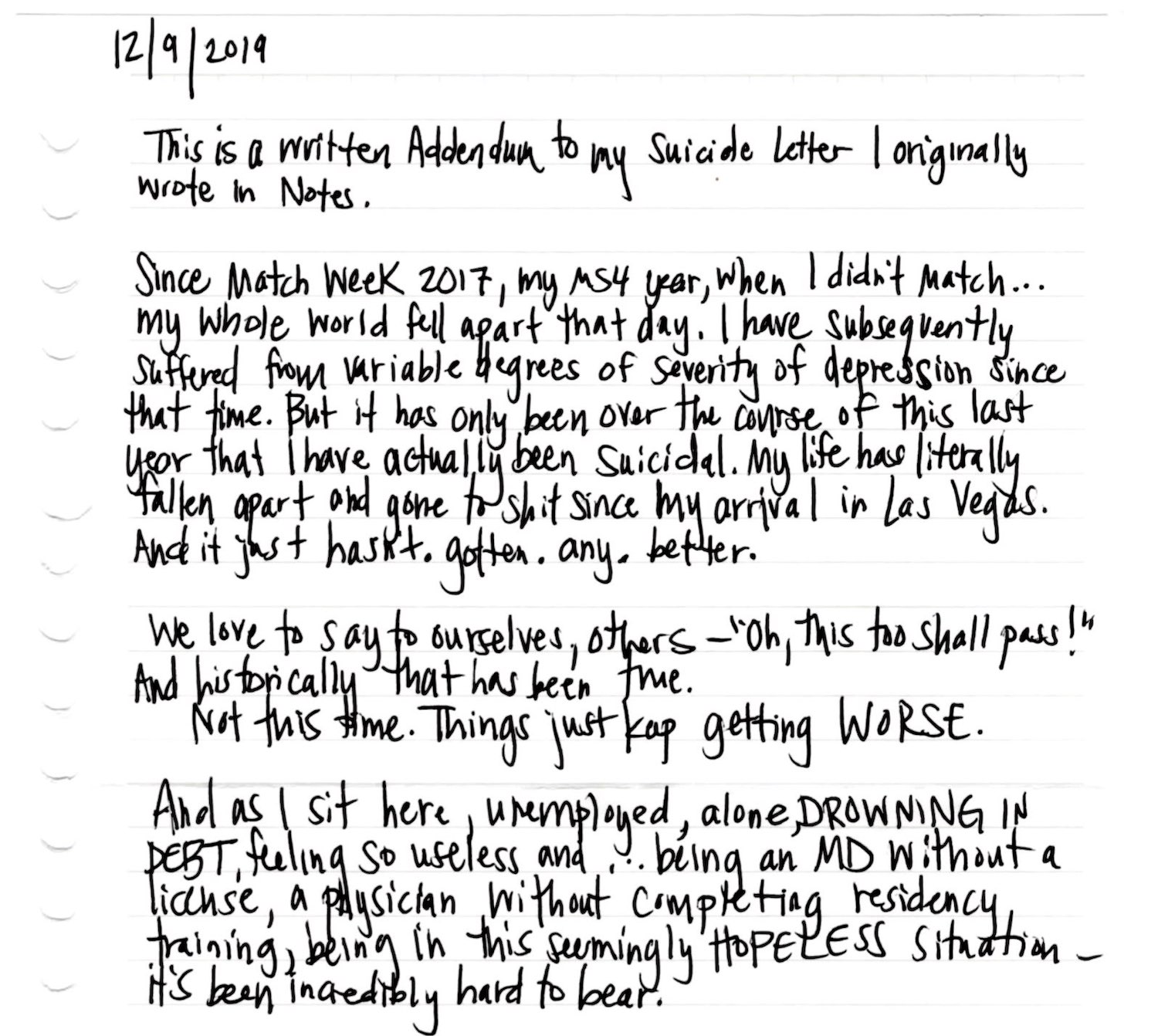
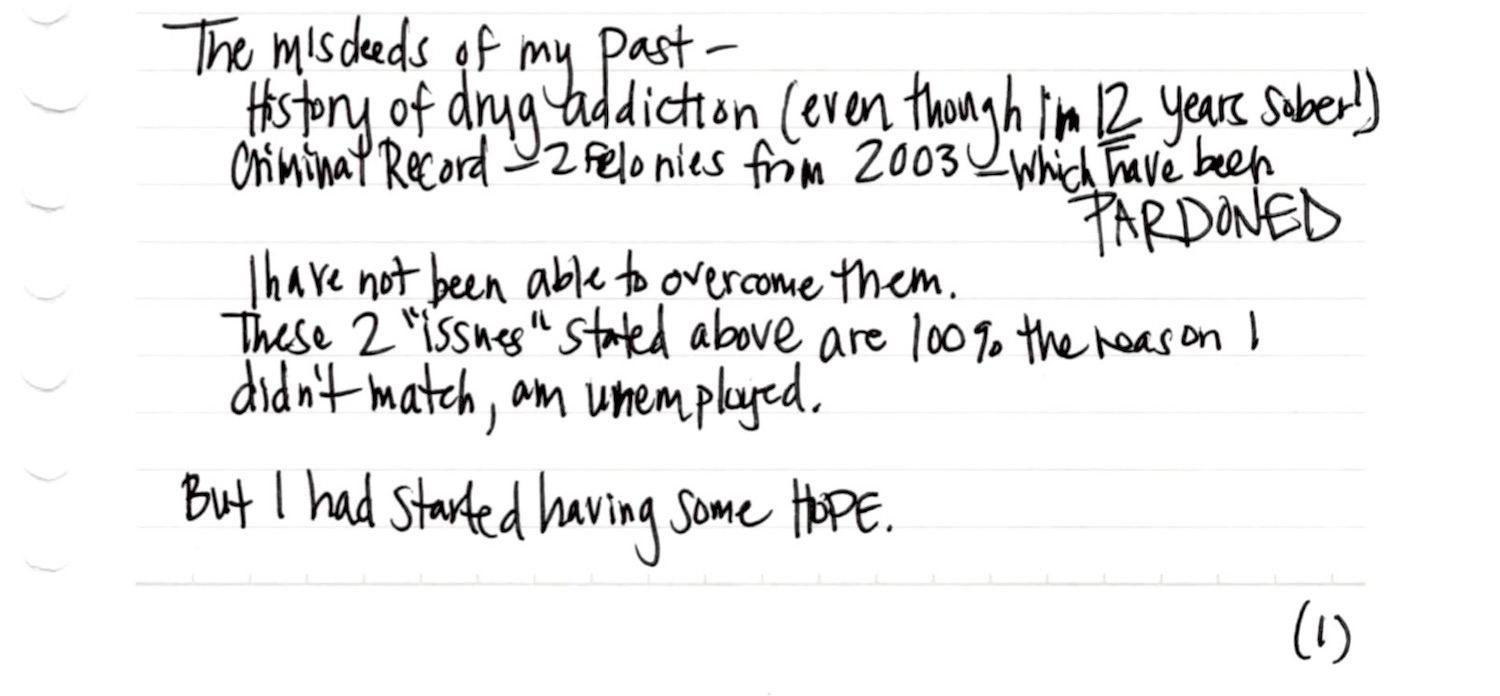
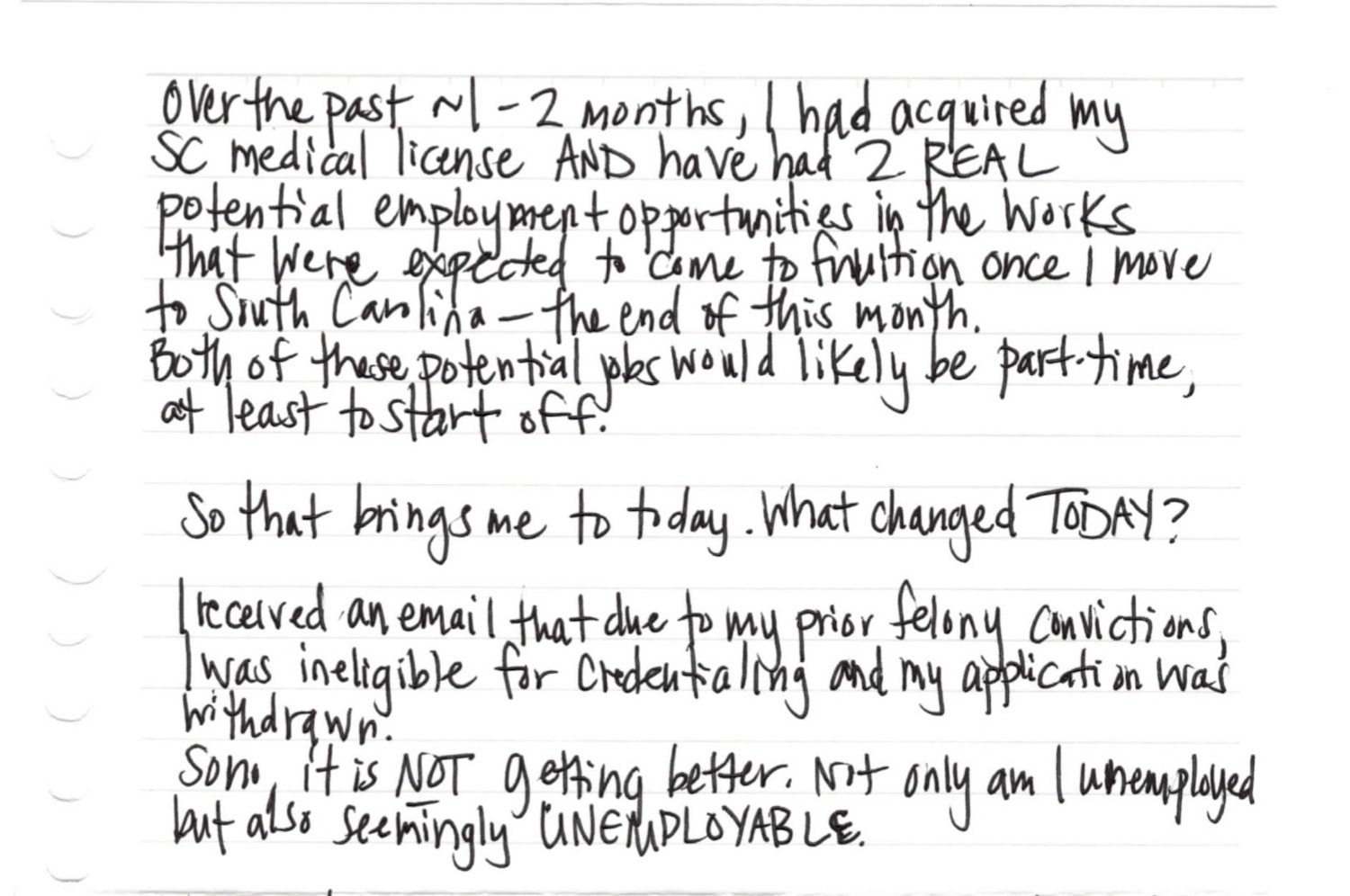
12/9/19 Addendum to Suicide Note—Part 2:
3/16/20 Addendum to Suicide Note—Part 3 (for her parents, unpublished).
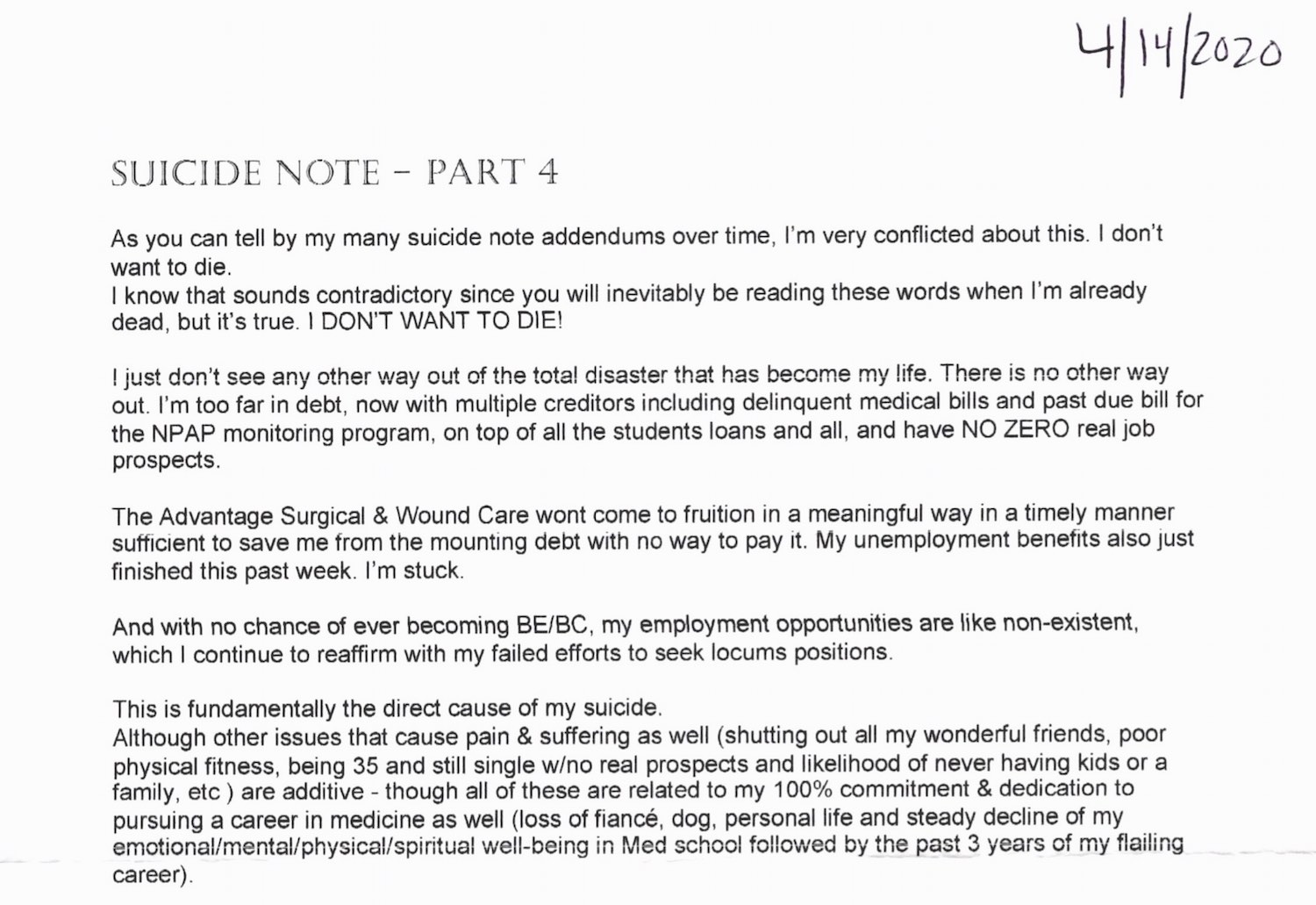
4/14/20 Addendum to Suicide Note—Part 4:
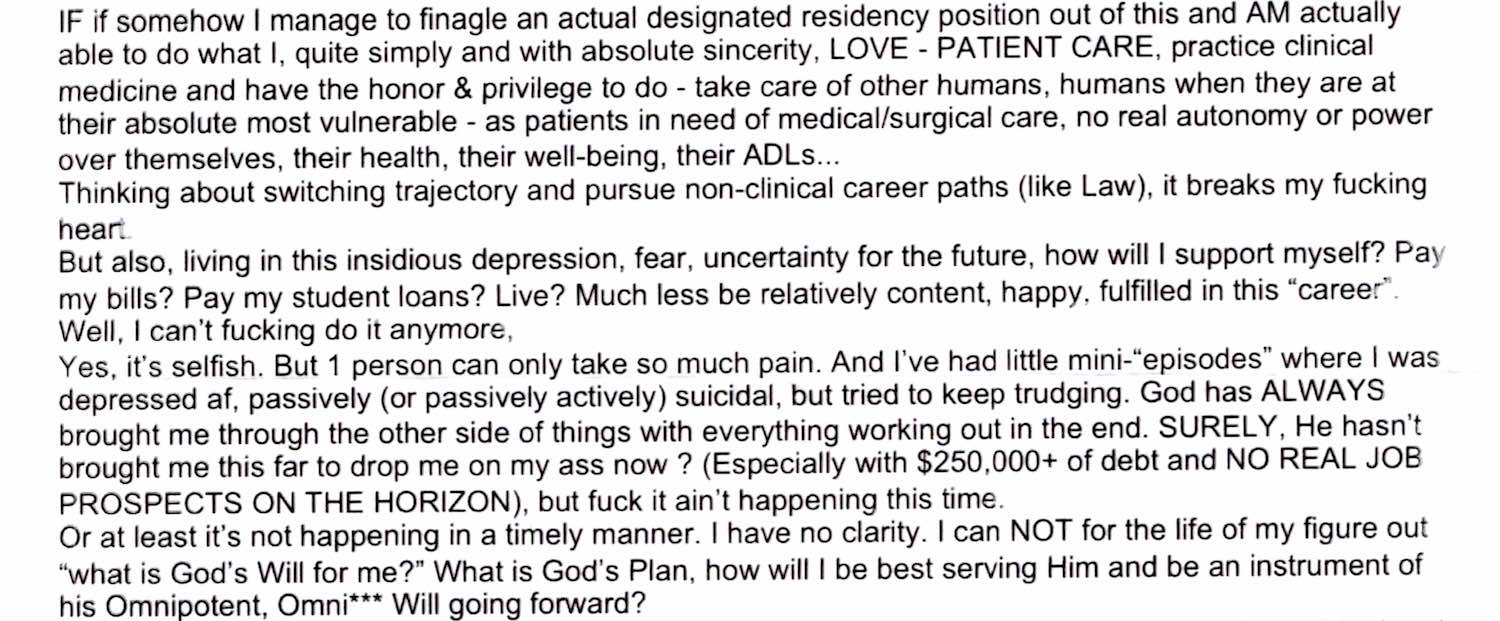
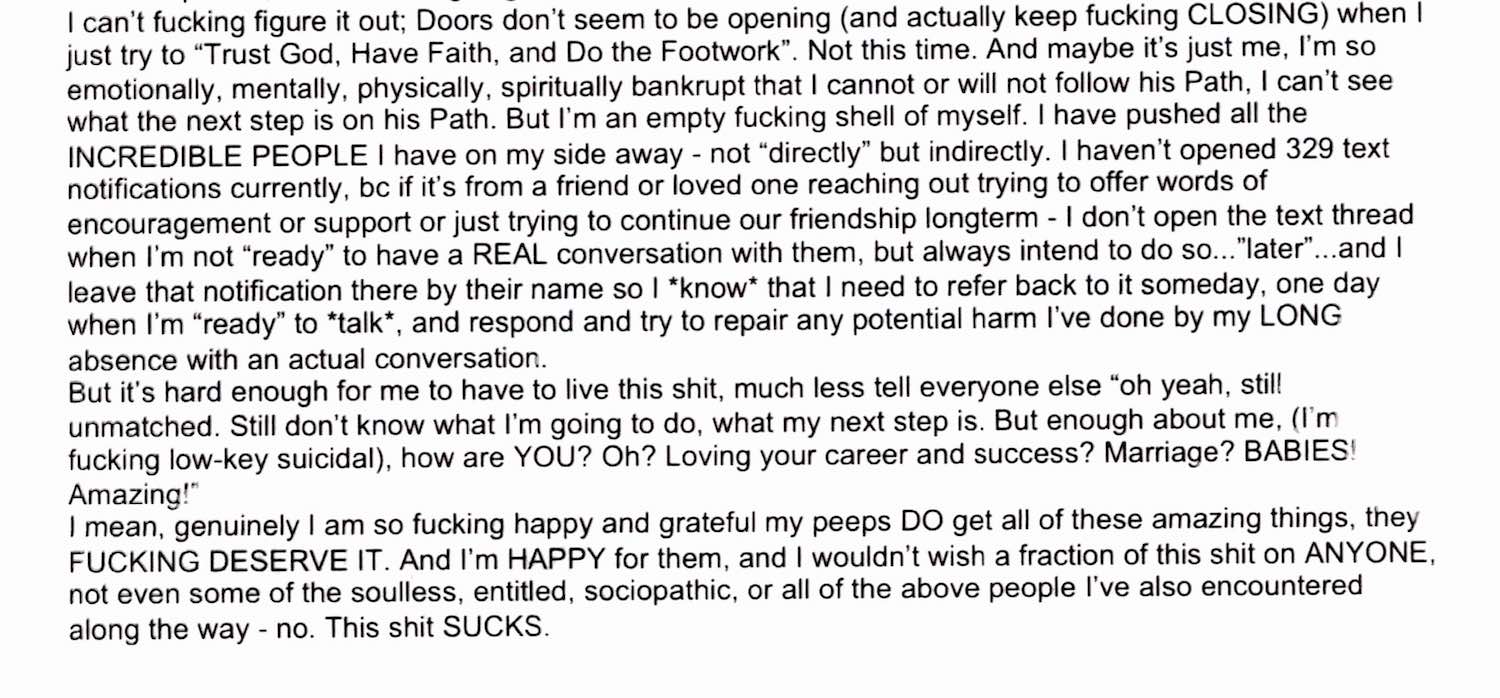
Leigh, my heart breaks for you every time I read your letters. You had a glimmer of hope that suddenly ended amid COVID-19 when your one potential job doing wound care at nursing homes fell through (as they stopped allowing anyone into nursing homes). You gave medicine your heart and soul—turned your entire life around in the most exemplary fashion. To then end up in such a state of hopelessness is tragic.
The issues leading to your suicide as you outlined are threefold—#1) being unmatched to residency as a result of #2) stigma/discrimination due to past addiction (though recovered) and your #3) unrelenting debt.
Secondary issues relate to isolation we all face in medical training—the loss of time for friends, family, pets, lovers, childbearing— as we dedicate nearly every waking moment to the study of medicine so that we may have the honor of caring for others at their most vulnerable.
What is so challenging for us all to see as physicians is that we are all so vulnerable—to isolation, anxiety, depression, and suicide. Isolation leads to more despair as we lose our grip on reality—all the choices we still have. We feel stuck. Trapped. Hopeless. I was there. Unable to get out of bed for 6 weeks. I was suicidal—100% related to career disillusionment. I get it.
Now I’ll address the specific issues that led to your suicide:
#1) The Match (or “Mismatch”)—Each year more than 1000 US medical school graduates do not “match” into residency—a requirement to practice medicine. Limited residency slots create a bottleneck in which new doctors are unemployable as physicians—while interest on student debt grows and job prospects wane. Many try unsuccessfully to match year after year. Applying for competitive specialties like orthopaedics is risky even for stellar applicants with pristine academic records. Each failed match is another red flag on one’s professional file. As new US medical schools open—more doctors compete for limited residency slots (including international medical school graduates). Medical schools happily accept tuition (some 80K/year!), yet continue to graduate doctors with no guarantee they’ll ever be employable. More on the plight of the unmatched from a woman who wrote me: I’m a doctor. I’m on Medicaid. I work as a waitress.
What’s the solution? The mismatch of the number of medical school graduates to residency slots is not unique to the US. In 2016, Robert Chu, MD wrote letters to medical officials and government leaders calling out the flawed match system in Canada— the lack of residency slots that undermined his career prior to his suicide. Some countries like Australia accept their own nation’s graduates first before filling spots with international graduates. Should US doctors be matched with residency positions first (prior to opening up positions to non-US graduates)? Should med schools that accept a student’s tuition be required to offer a residency slot so as not to leave their own graduates unemployable? Leigh, I wonder if your advisor ever warned you of the potential discrimination you would face based on your history? With your criminal record, I’m concerned that you would risk never being credentialed at a hospital (even if you landed an orthopaedic residency). You strike me as a feisty, determined entrepreneur. My kind of woman. Did you ever consider launching your own practice back home to care for the underserved as you originally desired? You absolutely would have been super-successful in your own clinic with no additional residency beyond your year at Rutgers. I would have loved to help you.
#2) Discrimination. Leigh, your perseverance against all odds in pursuit of a career in medicine is absolutely inspiring. Yet the stigma and discrimination within medicine related to past substance use/abuse/mental health is so ingrained. Did anyone warn you of the prejudice you would face in medical training—especially in residency? Given the volume of applicants for limited residency slots, programs often discard physicians with a blemished past. While your addiction recovery/mental health advocacy is truly commendable, your transparency may have limited your ability to match into your top specialty choices. Your incredible recovery may not have been interpreted as a strength, only a liability, by medical institutions—and that is so unfair.
What’s the solution? Addiction/mental health stigma in medicine needs to end. It’s happening—ever so slowly. Finally some states are removing ADA-non-compliant questions from their licensing applications. So are hospital credentialing committees. Focus should be on current competence, not distant history of substance use or mental health issues. Yet many medical liability carriers, health plans, hospitals, and states medical boards continue to require applicants to answer “have-you-ever” questions about remote substance use and mental health conditions that are clearly out of compliance with the Americans with Disabilities Act. See special edition of Qualitative Research in Medicine & Healthcare devoted to ending physician mental health discrimination.
#3) Debt. Many medical trainees lack informed consent of the emotional, physical, and financial risks of a medical education. Amassing 300K in debt with compoundable interest creates so much distress for all graduates—especially for physicians unmatched into residency. Medical students and physicians often cite debt as a factor leading to their suicides.
What’s the solution? Avoid medical schools with exorbitant tuition. State schools can be much cheaper. Choose your career path in health care with finances in mind. Many training programs (PA, NP, RN, MSW) are far less expensive, require fewer years of training—and do NOT have a hidden residency bottleneck—so you WILL be able to actually use your degree. At minimum all states should follow the Missouri law that allows unmatched doctors to practice as “assistant physicians” so they can at least earn a living while applying to match in subsequent cycles. If you do graduate medical training with large debt, consider income-based loan repayment and work for a nonprofit (or start your own) to qualify for loan forgiveness.
Leigh, I so wished I could have had the chance to talk to you. I would have moved mountains to help you find your way. I’m filled with grief that it is too late. I feel like I know you after speaking to so many of your friends and family. We had a beautiful dedication to your life at the Do No Harm film screening on May 3. Your Memorial Scholarship has raised nearly $60,000. So many people love you! You were a phenomenal physician. I hope that my letter (and your words that you so courageously demanded be published) will finally create this culture change in medicine we so desperately need—in your honor . . .
~ Pamela Wible, MD
P.S. Losing one’s dream in medicine doesn’t have to end in losing one’s life.
PLEASE HELP us change medical culture, Punishing people for a disease is not health care. Dr. Leigh Sundem’s parting wish is to end the stigma of drug addition & mental illness within medicine. Contact the following organizations to voice your concerns:
National Resident Matching Program (NRMP) Board of Directors
American Accreditation Council for Graduate Medical Education (ACGME) Executive Committee
If you feel thwarted in living your dream in medicine, please read Secrets to loving your life in healthcare. Answer the 7 self-reflective questions at the end. You have many choices. Contact me for help. View award-winning documentary that exposes the physician suicide crisis.















You say that you wish you would have known her sooner and that is a generous thought, but it doesn’t matter. I know because I am a physician without a future just like Leigh. Like her I have sacrificed to study medicine and I know I would be a great benefit to my community, but for lack of a Residency after 3 years trying and I cannot afford to keep at it. I am in a deep dark place and each day is a struggle to go on. I know eventually I will break and there is nothing anyone can do. I hear there is a doctor shortage but I guess some people aren’t good enough.
Marisa, I am so glad you left a comment and I would love to speak with you today. 100% confidential (and also have free confidential support calls every weekend for doctors and med students so PLEASE DO join us). I would be so happy to help you and YES there are options even without residency so my best advice is to just PLEASE contact me here. (if you get a chance to answer the 7 questions at the end of this keynote that would also be helpful for me to guide you).
Marisa, please message me.
Marissa
I am an ER doctor in a Houston Texas. Please contact me.
You’ll figure out the next steps. Talk with someone. You can do it!
Oh Pamela, her words break my heart. Leigh sounds partly so much like Ben. Their agonies are universal and soooo preventable. I too soooo wish they had both reached out and….. isn’t that the wail of all of us who have lost our best and most beloved. This feels so utterly overwhelming. So it’s gotta be one change at a time. One battle to win, then the next…I’m committing, forever, to be in this fight. For Ben. For Leigh. And for all the others still in pain, but still alive. It’s the most crucial human obligation. You have my solemn word.
There are enough residency spots for Americans to match. This should have never occurred. The issue at hand is competition (foreign citizens) and program directors allowing this to happen. The combination of American and Foreign doctors competing for federally funded positions has cause program directors to use absurd filtering during ERAS/residency application season. This results in thousands of qualified American medical graduates get discarded like trash even though they’ve passed their medical boards. Good job PROGRAM DIRECTORS. Trash the American citizens for foreign citizens. American citizens get FEDERAL loans and want to achieve FEDERALLY funded residency positions. Many Foreign citizens attend medical school in government funded medical schools, which means they are debt free all while Americans are oozing with medical school debt.
Either way, this is sad that this young lady worked her tail off and couldn’t secure a categorical residency position, but tons of India, Pakistan, African citizens obtain these positions. FIX THIS ISSUE AT HAND!!!!
So many medical school graduates treated as medical waste. No PPE. No secure residency position. Expendable. A sick system that profits off the hearts and souls of some wonderful trainees. When they begin training they do NOT have informed consent of: 1) The mental health impact of medical training/practice; 2) The residency bottleneck (they they may be unemployable as a doctor after everything—dedicating their entire lives (or most opf their youth) to medical training; 3) Financial implications of compounded interest on 300K debt (medical school loans for a school that does not guarantee them a residency position as a graduate is infuriating and so unfair). This is how the medical profession treats its trainees.
Those who make it through al of this are still dealing with the long-term impact of human rights violations in medicine. Both my parents are physicians and I was NEVER warned about any of this. Collateral damage. Like its normal to discard > 1000 US graduates each year just to the “Mismatch.”
I am a physician at an academic medical center who trained overseas. There is no doubt the system is broken. However, “they are taking our jobs” is an oversimplification. It is not a black and white issue. I have interviewed at a dozen hospitals including those that exclusively serve communities of color as well as the biggest names in academia. I have also been advising peer IMGs for over 10 years.
In most cases, IMGs are the last choice for Program Directors. We fill residency spots in areas where no US grad will set foot. Hospitals in areas like Bronx, Harlem and mlst rural America hire IMGs as workforce because they have no other option.
There is no doubt that there may be some program directors who would take an IMG who graduated with honors over a US grad who has done poorly in med school. It is debatable whether hiring a potentially dangerous intern is preferable over sponsoring a visa.
The system is also broken in that step scores or poor performance in clinical rotations may not be reflective of actual potential as a doctor. I personally know four doctors who graduated from Ivy League med schools and matched into prestigious residency who were plain dangerous physicians – three dropped out of residency or were fired. One completed training and is in private practice. The system works for most people and some inevitably fall through the cracks. By the way, thousands of IMGs and FMGs are US citizens by birth who desperately wanted to go to medical school and didn’t make it to US MD or DO school and chose to go to school outside of the US. Their failure to match is far higher than US MD and DO grads. There are plenty of stories of anguish there as well.
Hospitals are corporations. They are in the business of making money and mitigating risk. They will try and do the least risky thing possible. In case of the unfortunate author her criminal record was a bar to being credentialled. I wish the victim had a chance to speak to you. There are many non clinical careers open to doctors. Yes, one doesn’t get their share from the well oiled rent-seeking machine that US medical practice is, but if one can get through undergrad and med school, then most other problems are a matter of time and perseverence. We need better advising resources for non-clinical careers for doctors who are not cut for medical practice or are forced out of it. You are providing a valuable resource by highlighting some of these issues.
*Comment typed on a phone. Please ignore typos*
What do you suggest is the solution? I do not think allowing 1000 US doctors to fall through the cracks is something we should permit. Just curious your thoughts and I hear ya with your comments above. How would you fix this?
I’d hate to start an argument here, but some things need to be made clear.
Foreign/International Medical Graduates are not stealing jobs. On the contrary, the vast majority are working in areas and specialties that US graduates wouldn’t even consider going to. These are highly trained foreign professionals that more than meet US regulation standards who didn’t cost the US a single penny, but come support the most undeserved of communities. I urge anyone who thinks FMGs are a problem to read the NRMP match data, and look up the list of residents at University or non Internal Medicine residency programs and see how silly it is to think of FMG/IMGs as competition.
Regarding residency or the job market in general, US graduates are already prioritized, and rightfully so. Those who didn’t match likely either applied to (highly) competitive specialties without foolprooth backup residencies and got beat out by their American peers, or had red flags in their records and were selectively filtered out. Whether this process is fair… is illustrated by this tragedy.
As for finding positions for the 1000 (5-8%) US graduates who didn’t match. This can easily be remedied if they applied like IMG/FMGs. Thats to say if they “JUST WANT A JOB”, then apply to “ALL” of the least competitive posts (Internal Medicine 587 programs 8,697 positions 373 unfilled; Family Medicine 706 programs, 4,662 positions 349 unfilled; Pediatrics 222 programs 2,864 positions 52 unfilled). Obviously most people don’t want to settle for “just a job”, hence the number of unfilled positions and openings for IMG/FMGs. However, if those who advocate for a 100% match rate are actually proposing that competitive spots become less competitive and everybody gets to be the orthopedist/ ophthalmologist/ neurosurgeon/ plastic surgeon/ dermatologist they dream of becoming, then it’s a completely different story.
AMP, Love to hear ALL thoughts so no need to worry about starting an argument. I’m more concerned about a lack of discourse. I have to say I was fortunate back in 1993 when I graduated from med school with only 22K debt (Thank YOU UTMB/Galveston) that I paid off DURING my residency in family medicine which I LOVED. I only applied to TWO residencies and got my first choice. Now I hear people spend thousands applying to like 80 programs!!
The only reason I am so familiar with the plight of the unmatched is due to the volume of calls on my suicide helpline from graduates who are unmatched and unemployed or underemployed and absolutely discouraged to the point of contemplating ending their lives. My impression is:
1) These unmatched US grads would be thrilled to take residency positions in the worst areas (if offered to them).
2) I would recommend that we avoid INFIGHTING (us-versus-them victim infighting merely allows the status quo “mismatch” to prevail). This should not be an IMG vs. US grads fight. Ideally.
3) US grads (and any medical student/doctor) must be given INFORMED CONSENT about the emotional and financial impacts of not matching BEFORE med school and be given resources to make the best decisions for themselves because having 300K debt with compounding interest and suicidality is not a sustainable situation for a young person starting their career. SO . . . in my opinion . . . if a med school accepts an applicant there is a duty to support that trainee and help them acquire a residency. Leaving them unemployable is a breach of contract and some accountability should be placed with the educational institution to help their own students after they paid 300K for their education. A refund? An apology? Some career counseling? Help getting into a PA/NP program. Something. . . (I also feel that some young people are so rigid about their plans/goals that the may not hear and accept the mentoring that comes their way–another topic I could go on about).
4) Your second paragraph makes total sense to me and is absolutely tragic. These trainees need informed consent and mentoring/advising so they have realistic plans that do not leave them completely lost and unemployable.I don’t think many grasp the tragedy until they are in the midst of it without support and emotionally vulnerable, alone, with bills due.
5) I do believe that these unmatched US grads actually apply to as many residencies as they can (just like IMG/FMGs – at least that is my impression.
6) I am not suggesting that competitive spots become less competitive.
Caveat: I am no expert. I am coming from the vantage point of someone who has spoken to thousands of suicidal med students/doctors and I absolutely believe there must be a solution to this other than waiting for people to break down, give up all hope, and die in the prime of their lives.
Can we put our heads together and come up with a solution? I am certain we can so I am pleading with everyone who reads this and has any ideas to please chime in. We are bright and resourceful and I know there are some untapped great minds out there. So join in this conversation. . .
Unmatched American citizens would do anything if they can get a residency spot.
I believe the key word here is unmatched. That means they have already failed to match. That in itself is a red flags hen you apply again. This is amplified if you suddenly switch specialties. A FM program for instance would have second thoughts of taking a failed dermatology applicant knowing that they were not interested in FM. Having residents leave after matching makes programs less desirable for applicants. The solution is medical schools must have a discussion with the student when applying to residency that they are unlikely to get that dermatology position should reconsider. Choosing the right specialty the first time prevents being unmatched.
Regarding Leigh, it’s sad. Prior remote addiction issues should not be a factor especially when the applicant proves it’s not a current issue. It is a problem with this country that criminalizes drug use. The government has no business worrying about someone doing meth, cocaine, heroin unless it endangers the public. I’m dumbfounded that state boards would refuse a license because of remote convictions given the following. There is (maybe retired now) a California doctor that practices GI for 20+ years after serving time for killing both his parents during a camping trip.
“There is (maybe retired now) a California doctor that practices GI for 20+ years after serving time for killing both his parents during a camping trip.”
Do you have a link?
Okay. Listen here you FOB lover…let me see things straight for you. You quote match statistics but those statistics dont account for application fever caused by FMGs and the result of sexual intercourse between the AMA and ECFMG. Dr. Pinsky love his towels to come here and overapply such that most applications do not get a thorough and holistic process. You are lucky to have a job but not for the unmatched. Before you claim that you know your shit, read up on application fever and see how it affects everyone who applies to the MATCH.
Listen here you FOB lover. You exhibit “FOB privilege” and it needs to be checked. Have you ever heard of “application fever?” [https://thesheriffofsodium.com/2019/03/02/the-etiology-of-application-fever/] If not, look it up and educate yourself on it. Application fever is caused by FOBs who overapply and program directors who are too f__king lazy to thoroughly evaluate medical students. They let a computer do the sorting and place a limit on how long a person can apply. You have a job because you met criteria at a specific moment in time. The unmatched cant apply because of selection criteria and application fever. Application fever is being promoted by sexual intercourse between the ECFMG and AMA. Before you cite “I have these things…” learn about the other side before you start dismissing their claims. You are so ignorant…why not help the country in which you originated?
I am an UNMATCHED American citizen there are over 4700 of us who are unmatchec. And yes I applied for Family Medicine.
I am an UMMATCHED IMG American Citizen. Yes NON US citizen IMGS are taking our JOBS.
I am an UMMATCHED IMG American Citizen. Yes NON US citizen IMGS are taking our JOBS.
AMP, Thank you for articulating my thoughts and experience. I am one of those IMG/FMG who fought tooth and nail for a Residency spot that was so evasive. It took me over a decade graduating from medical school to landing a Residency spot. Yes! numerous “dark years”, during the process, heartbreaking years, working odd jobs to survive. But with Family’s love and support that you must value more than your own pride, and most of all trust in the living God who brought you to this point for a PURPOSE, finally after a long circuitous road that at times seemed endless, The Ohio State University casted my Lifeline. I will forever be thankful for the Department of Psychiatry Residency Selection Committee for taking a chance on me. I am one, forever grateful Physician, who gives my all in my practice, continuing to balance quality Patient care amidst all the clerical, unnecessary and non-medical demands of Medical practice. My motto is Quality Patient Care FIRST, to accomplish that, I devote most of my personal time doing Charts. Is it sustainable? Time will tell. What sustains me is seeing grateful Patients get well and continuing to do well, I would like to think results from TAKING TIME to LISTEN, UNDERSTAND, regard and Quality time given to Patients while practicing Evidence Based Medicine. How long will this dinosaur ? last? only time will tell, hopefully for as long as I see Patients life turn around for the better.
Over a decade! Wow. How many cycles did you apply? How many denials before you found a spot?
Listen here you FOB lover. You exhibit “FOB privilege” and it needs to be checked. Have you ever heard of “application fever?” [https://thesheriffofsodium.com/2019/03/02/the-etiology-of-application-fever/] If not, look it up and educate yourself on it. Application fever is caused by FOBs who overapply and program directors who are too f__king lazy to thoroughly evaluate medical students. They let a computer do the sorting and place a limit on how long a person can apply. You have a job because you met criteria at a specific moment in time. The unmatched cant apply because of selection criteria and application fever. Application fever is being promoted by sexual intercourse between the ECFMG and AMA. Before you cite “I have these things…” learn about the other side before you start dismissing their claims.
Anyone can be a good doctor with the right teachers.
“In most cases, IMGs are the last choice for Program Directors. We fill residency spots in areas where no US grad will set foot. Hospitals in areas like Bronx, Harlem and mlst rural America hire IMGs as workforce because they have no other option.”
Why not help the unmatched AMGs as well?
You, Mark and AMP, both exhibit “FOB privilege” You don’t know the experiences of the unmatched and you give fake pity for their plight. You are a part of the problem and you should be removed from your positions as you don’t exhibit compassionate behavior that of how a true physician should be. Go back to your own countries and help with the COVID response. #TowelsforPinsky, #FOBfactorysupporter, #FreezetheFOBfactories
So what I would like to ask is that discourse be meaningful and cordial. Please do not discredit others just because they have opposing viewpoints. Thank you in advance.
This made me feel physically ill to read. 🙁 I hope she rests in peace. Reading her notes I just want to reach out and comfort her but she’s gone…
YES! I so agree. I wish she were here instead of spread in ashes in the lake. I can not believe (still) that the medical system can be so cruel. She is so deserving. Why perpetually punish people who prove that they are worthy. She was the poster child for recovery. Clean & sober until her last breath.
Terrifically sad case of an ill person. She may have not been using but she didn’t seem “sober” by recovery definitions, and clearly needed outside mental-health help. Perhaps she was getting that help. Hope so. Yet, for those who need to get and stayed recovered from alcohol and drug addiction, it’s frustrating to not only read this but to know other people who need recovery are reading it and thinking “why bother?” While she has every right to ask to be “widely published,” for the medical part, the addiction part is dragged into the fray. Sick and sad people claiming but not exemplifying “sobriety” that results in suicide are examples of un-sober, dry addicts. I am not criticizing this poor woman but I would ask that someone clarify that true sobriety as learned and practiced in recovery fellowships does not result in angry suicide.
I agree with you that from her comments it seems like she needed help she wasn’t getting, but how could we really expect her to as we have demonstrated that she will be punished for seeking help?
Leigh Taylor Sundem, MD, indeed was clean and sober, focused her life in the direction to help herself and to help others. The medical education system in this country is brutal; the stressors and pressures incessant; the acknowledgement not present. Lies are rampant. Leigh knew what and where she wanted yet had no idea copious **** abounding and poring down the chain of hierarchy with too few reach out and offer encouragement. The eddy for Leigh was fierce, and sadly she was not able to get the help and kindness she needed.
Laura Lee, I am afraid people reading your comments will be mystified by most of it.
What is a “recovery” definition of sobriety please? Is it different from a medical definition? If so, why would that be? Is “sobriety” only awarded when it is “happy?”
You seem confident that Leigh needed “outside mental-health help”. What is that, exactly? She was paying the NPAP, in fact that was part of her insurmountable financial burden. Why wouldn’t a physician who is paying a physician health program (pushing her further into financial jeopardy) while unemployed, qualify in your book as adequate mental-health help seeking? And is your psychiatric assessment (“sick and sad person claiming but not exemplifying “sobriety” that results in suicide”) based on your expertise as a “recovering”? If you were a psychiatrist, or even a non psychiatrist physician you should know it is not ethical to make a diagnosis on a patient you have not examined.
Why do you feel she does not have “the right to be published”, regardless of your presumptive diagnosis?
What do mean “for the medical part”? This makes little sense.
What do you mean, “the addiction part is dragged into the fray”?
It was well established that this woman was sober for 15 years. She was nothing short of exemplary in her recovery, and her goal was to help keep other young people out of addiction.
Are you suggesting that because she had surmounted an addiction problem in her youth, that she had no right to suicide 15 years later, because it might reflect poorly on “recovery”?
Can you clarify what you believe points to this woman being an “un-sober, dry addict?” And what exactly you mean by an “un-sober, dry addict”?
This makes no sense whatsoever to the average person. It sounds like propaganda.
Or “sick and sad people claiming but not exemplifying “sobriety” that results in suicide?
You seem to imply in your last statement that “angry suicide” does not happen in people with “true sobriety as learned and practiced in recovery fellowships”. Yet you want someone else to clarify your own strange contention. Again, it sounds as if someone has convinced you that the only true recovered person is a happy recovered person.
I personally believe that for you to label Leigh’s as an “angry suicide” is first, presumptuous, second, demeaning, and third unmerited. What do you think YOU might sound like while writing your last words when you felt that systematic and unfair employment discrimination by a system you had spent half of your life preparing to help, had left you no options with which to address the resultant, crippling debt? Peaceful, blissfully happy, because “truly sober”?
Finally, to imply that somehow this might NOT have been so had she only had “true sobriety as learned and practiced in recovery fellowships”, along with your very strange use of the English language, suggests that you have yourself been brainwashed by such a system. So now, it must be time to “help” others by dispensing such drivel?
I believe we should let unmatched doctors work as PAs. This would help so many people. I also believe unmatched doctors should get debt forgiveness until they match. As someone who matched with a blemish on my application I know how hard it is to succeed even with one flaw there. I am so thankful every day for my happy ending. But I know others who had heartbreaking endings a person who committed suicide after a bad evaluation which that person knew would preclude their dream of Dermatology.
I feel medical students should have informed consent explaining the financial and health risks they are taking, and also be more informed that a single flaw in their performance could cause them so much agony and even make it difficult or impossible fo match. Before I started medical school I never imagined how unforgiving it would be. I tell people now to strongly consider PA school.
So, I am a physician who was dismissed during my prelim surgery internship. The first time I matched, I received plenty of interviews and matched at my #1 choice. With this dismissal on my record, I applied to 3 times the number of programs and hardly had interviews and didn’t match or SOAP into any specialty. It’s been a humbling experience to say the least, but I still carry on knowing it’s only a matter of time before something falls into place. When over 5K people don’t match per year, it make sense a program director doesn’t have to bother when there are red flags on the application.
I am so sorry Michael. Given Nancy’s comment, I wonder what your Plan B is . . .
This is happening to me as well. Due to previous training record, no one takes me.
Indeed, we need to end discrimination.In South Africa is worse and people areunderplaying it. College of Medicine South Africa together with their cahoots are destroying the lives of Black doctors especially females. I am their victim who needs a pro bono lawyer to take this matter to the constitutional or equality court before we loose more of our colleagues. International human rights please help.
I am so sorry Molatlhwa to hear this, Human rights violations in medicine are real and the culprit for so much pain and agony in young trainees. It is unconscionable that we allow our own young doctors to suffer under such unsafe and hazardous educational and workplace conditions. WE all need mental health care due to intergenerational wounding from the unmet mental health needs in those who are now training us through terror, bullying, hazing etc. The genesis of so much of our problems in medicine is due to lack of mental health care (among persecutors and victims). I choose to believe most of us enter the field with noble humanitarian intentions and then we are injured. “Hurt people hurt people” as they say. More JD/MDs will help advocate for the changes that we need.
Tragic on multiple levels. Solution: I think every applicant to medical school needs to have a realistic plan B, for both non acceptance in to medical school or not matching for residency. I think this would have a two-fold effect: it would show medical schools that the applicant is capable of thinking through options, and the it allows an applicant to broaden their focus. Obviously, that someone has a well considered plan B is not an indication they are less committed to medicine when it is a universal question.
One of the themes that resonated through her suicide notes, was “unfairness”.
There is a lot of unfairness and it happens to good applicants who are turned away due to reverse racism, perceived values, etc. There is a movement away from a merit system, and this will come at considerable cost, too. In fact, if you make things less objective, there is more dependence on subjective means of evaluation which can be very damaging—just general thoughts from someone who taught medical students on clinical rotation for a long time. In the end, I think what got this doctor most was her criminal record. I didn’t pick up on the nature of the felony, only the substance abuse history. From a legal standpoint, I think acquired “good points” over time could be used to have such a history potentially erased when someone has created a productive life for themselves particularly when a number of years have passed. Medical records should be as protected as the general public’s.
It’s such a shame. This physician was in the pit of despair. Thank you for the work you are doing.
“If you make things less objective, there is more dependence on subjective means of evaluation which can be very damaging.” Excellent point! Thank you for your wise words Nancy.
As for her criminal record it was related to the drug issue and being at the wrong place at the wrong time kind of thing. She had these felonies pardoned though not expunged (she had advocates in the legal system in Georgia – including judges – who were trying to get her record expunged—-would have been potentially been lifesaving could that have happened before her residency application cycles and job credentialing process).
“Reverse racism?” Is there an acceptance that is a real thing? Can we attribute suicides to a person not matching due to “reverse racism?” People aren’t being systematically turned away because they’re white. That’s absurd, irresponsible language.
Leigh was my friend and supported me through college. Without her, I wouldn’t have done as well as I did. She was loyal, courageous, and never let her past prevent her from achieving all of her goals. She was extraordinarily bright and funny. Everyone that knew Leigh personally is absolutely devastated by her loss. Reading her actual suicide note was crippling, but true to Leigh fashion, it was eloquent, honest, and blunt. Her memory will live forever in the hearts of those who knew her and even in her death, she will enact change… just as she did in her life.
Oh Megan, my heart breaks for you and the loss of your amazing friend.
Dr. Wible,
I truly appreciate what you are trying to do, and admire your work. But it is truly dangerous to publish this in this form. Please consider these guidelines. Publishing a suicide note is highly suicidogenic, and may inspire others in her position to commit suicide. At least remove mention of her chosen method of suicide- again something that is likely to cause further suicides.
-A Concerned Physician
A Concerned Physician, Thank you for writing me and I appreciate your concerns though I disagree with you.
Suicide is not the problem. Censorship is the problem.
I strongly disagree with censorship. Method, age, circumstances matter. Censorship has hindered our ability to deal squarely with the issue as adults (and as scientists in medicine we need to know these details—-see Washington Post article with my findings here): (a few data points)
Physician suicide methods vary by region and gender. Women prefer to overdose and men choose firearms. Gunshot wounds prevail out West. Jumping is popular in New York City. In India, doctors have been found hanging from ceiling fans.
Male anesthesiologists are at highest risk. My registry (now with close to 1,500 cases) also shows that most of these doctors kill themselves by overdose. Many have been found dead in hospital call rooms where they are supposed to be resting between cases.
Without data we can not move forward with understanding and preventing these deaths.
Newspapers are filled with gun violence, kidnappings, rapes, and reporting on all kinds of tragic events (often sensationalized without solutions attached). My writing is very solution focused. Many doctors write very rational suicide notes explaining the very specific reasons why they chose to die and with instructions that could HELP us prevent future suicides. These notes must be read. In India (btw) they read suicide notes on the evening news and actually arrest people named in suicide notes as there is an abetment to suicide law.
I’ve published a book of physician suicide letters. (Free audiobook here) I can’t tell you how many doctors have contacted me to tell me the book helped them feel validated, comforted, and saved their lives.
I am available 24/7 (while awake) to speak to anyone in medicine who needs to talk and peer support calls.
I feel so related with some of Leigh’s words. I’ve stopped answering friend’s messages, I feel that I’m stuck jobless (though I completed my specialty! I’m not american BTW). Sometimes I feel that is just a depression flare, now I realize I’ve been depressed this whole time. Yes I’ve felt suicidal, but I always think it’s just a bad day and it will pass.
Feeling hopeless is hard when everyone expect you to be successfull.
Sorry for my english.
Please contact me here so you can join our support calls this weekend. Also please view the documentary on Sunday. I will be on the panel helping doctors with depression, trauma, and how to heal from our occupationally-induced mental health crisis (so many of us are suffering so please know you are not alone).
I’m so saddened to read this. What a beautiful young woman with so much potential who persevered to ensure her past didn’t define her future. Yet, others couldn’t afford her that privilege. It’s particularly poignant that she recognised that even with her ‘white privilege’ she was afforded some grace in places were POC would not have been.
I recognise that the Match system is designed to exploit us- from USMLE exams through to ERAS application fees. We are recompensed with a meager salary in residency and 80 hour weeks with little opportinity to see our friends/family and (for us women), have to put our plans to have children on hold. The system has to change- we need to lobby the government, we need to unionise. Her death, and the untimely deaths of many other physicians can’t be in vain.
Yes Sarah. really important to recognize that these working conditions are hazardous and actually violate our human rights. See this book that outlines solutions (many through agencies that already exist to protect workers).
(call me Spyder) How shall I describe myself? I am a USFMG, having been in practice in public psychiatry for 28 years. I don’t know how to keep suicide from happening, but in terms of addressing some of the risk factors: I developed a clinical depression after the death of a family member, have been in outpatient treatment almost as long as I’ve been a psychiatrist, without relapse since 1997 but afraid to stop the medication altogether. I wish I had the key to end stigma. I was badly treated early in my career by two psychiatrists who were self-treating their own depressions. Disclosure versus hypocrisy.
You speaking out openly and posting this helps destigmatize the topic. I’ve been in counseling weekly x decades as maintenance for my mental health (much like flossing & brushing for dental health). I don’t want to lose my mind any more than I want to lose my teeth. Every person in a high-risk profession (doctor, police, firefighter) needs routine at minimum weekly check-ins with a mental health professional of their choosing. Nonpunitive and 100% confidential. Your thoughts?
It’s not that long ago that psychiatry trainees were invited to undergo personal therapy (at our program the cost was shared, so reduced). Best thing I ever ventured into unknowingly. The psychoanalysts have us beat: they “require” that each candidate spend significant time as an analysand. 4 of our 9 residency candidates in my year experienced therapy. The other 5 laughed at us derisively. My initial fears were unfounded as I am grateful that what was uncovered became a source of strength. No one talks of the preventive potential of personal psychotherapy because the hypocritical ones want to keep their issues covert. I am lucky that my psychiatrist does not charge extra for each 1/2 hour that incorporates psychotherapy, in fact, I would not meet with a med checker, since I myself am not that kind of doctor. I seek and do psychotherapy. Am better for it. It’s hazardous to think any one factor will effectively reduce suicide risk but how about starting here? Thank you Doctor. Keep up your work and “call” any time. S
We all so desperately need therapy in medicine. Routine peer support at minimum.
Psycho-pathology runs rampant. There is NO ONE who could not benefit from insight into their emotions and the issues done and not done in their lives. And I refer to Freudian psycho-analysis from a true professional. It is not drugs but insight into one’s own life and altering years/decades of negative comfort zones to establish new and positive routines that become comfortable.
Dr. Wible, Thank YOU for publishing Dr. Sundem’s suicide note. Her words have helped me understand my son’s suffering for the first time. He is unmatched two cycles and this is due to his hospitalization in medical school for depression. He is fine now. A wonderful physician, yet he is unemployed due to the same stigma and discrimination that Leigh faced. The medical profession needs to stop punishing their own.
I am here for your son (and for you). If you or he would like to talk, please let me know.
I wrote similar words in my training. I’m still alive by the grace of God. Thank you so much for publishing Leigh’s letters. I find them oddly comforting and they validate how I felt in my surgical residency and how so many must continue to feel. Bringing this conversation out of the shadows is so healing for so many of us in medicine. I’m thankful I survived.
I strongly feel censorship has driven this conversation (and so many lives) underground. My loyalty is with Leigh and with those who are suffering in silence. I am so glad you are here with us and did not give up your precious life.
This makes me both sad and angry. Her medical school needs to accept some responsibility for this. They must have known she would never receive a license or residency spot. Did they offer her a spot? They had no problem taking $200,000 from her. I graduated from the same medical school as Leigh.
What do you think the school should do? Just curious. . .
A few options if a student does not match:
1) Guarantee a spot at a residency at the home school.
2) Find a permanent residency slot elsewhere.
3) Refund tuition.
4) Formal ongoing career counseling (until settled into another career or training program)
5) ____________________?
Love to hear your thoughts fellow alum.
I think we should be given the opportunity to sit for PA boards and lisencing. You don’t need a residency to get a 6 figure salary in patient care as a PA and you are required to be under the supervision of an attending. A PA job would allow you to pay back your loans, slowly but better than what you can make as a doctor without a residency or lisence. Also I know some who would make the decision to take a break after medical school and work some regular hours for decent money before driving into the abyss that is residency. I understand where she is coming from, I have spent every night since I got fired from my residency in my 4th year convincing myself to not put my scalpel to good use one last time.
Please join our support calls if you like. Having another one on Saturday at 5 pm PT (8 pm EST). We are here for you. I have some ideas for you.
This doctor is onto something worthwhile. From our medical school, maybe 40% of the ones who immigrated work as nurses, laboratory workers and so on. During one of our reunions they explained: do not pity us. We chose to immigrate for our families, we have no regrets. When we meet, I know my classmates to be good doctors and great people, they just have nonphysician jobs. A graduate deserves a shot at a health care career. Someone said elsewhere we ought not to allow “those people” into medical school… The true value of our education is in the development of a useful way to view and experience our world. Even those who might not pass a licensing exam or match to residency have an important contribution to make, if only someone would give them a break.
I think we should be allowed to sit for PA boards. Often medical students and PA students rotate together. I have yet to meet a PA student who didn’t get a job after graduating. Medical students who don’t match have no less of an education than a graduating PA student. This would allow them to earn a 6 figure salary and still continue patient care and clinical work. It would also allow those that are burned out after medical school the ability to work a relatively regular 40 hrs a week and make decent money to start paying off loans before diving into the abyss that is residency.
I completely sympathize with Dr. Sundem, I have contemplated ending my life every day since I was fired from my residency. I wish I had her courage, and it takes an immense amount of courage and strength to make that choice, it was not selfish.
Dr. Sundem and I had much in common. Her suicide notes brought me back to those I wrote in med school when I was her age. I made it, and she didn’t.
I don’t know why or how I was so fortunate to secure healing and recovery from the pain that drove me to being suicidal with a plan. I don’t know why I was able to navigate those same challenges and now thrive in my calling as a physician. I beat staggering odds with a lot of help and quite a few miracles along the way, that I do know.
If I can now be part of the solution and help destigmatize addiction/mental health issues among physicians, I’d like to help.
Thank you for the work you do.
Please join us this Sunday for the award-winning Do No Harm documentary by Emmy-winning filmmaker who has exposed the suicide crisis within the medical profession. After the film we have a live online expert panel discussing solutions. YOU are part of the solution. So glad you survived to share your story Kristen.
Listen here you FOB lover. You exhibit “FOB privilege” and it needs to be checked. Have you ever heard of “application fever?” If not, look it up and educate yourself on it. Application fever is caused by FOBs who overapply and program directors who are too f__king lazy to thoroughly evaluate medical students. They let a computer do the sorting and place a limit on how long a person can apply. You have a job because you met criteria at a specific moment in time. The unmatched cant apply because of selection criteria and application fever. Application fever is being promoted by sexual intercourse between the ECFMG and AMA. Before you cite “I have these things…” learn about the other side before you start dismissing their claims.
Anyone can be a good doctor with the right teachers.
“In most cases, IMGs are the last choice for Program Directors. We fill residency spots in areas where no US grad will set foot. Hospitals in areas like Bronx, Harlem and mlst rural America hire IMGs as workforce because they have no other option.”
Why not help the unmatched AMGs as well?
Dr. Wible – thank you so much for not only honoring Dr. Sundem’s wishes by sharing her suicide notes but also for the way you bravely advocate for us all. As someone who has experienced suicidal thoughts related to my job as a physician reading Leigh’s note was important for me, possibly even life saving for me. It is vital that notes like these are shared – when sharing is in alignment with the author’s wishes, such as in this case – not only as a witness and tribute to their personal struggles but also as evidence for the collective struggle that underlies physician suicides. Thank you again
A few things that I believe are important ways to frame this conversation:
1) Suicide (especially doctor suicide) has been so hidden/taboo. Taboo subjects that we refuse to speak about perpetuate the underlying issues of secrecy and shame. Talking about sex abuse diminishes its power, gives other hope, educates and empowers others. The same can be said on the topic of suicide. Shrouded in secrecy and shame, suicides increase and the isolation of depression is fueled.
2) My call to action is to help create the change that Leigh Sundem would like to see in medicine— contacting the NRMP and ACGME is essential. Please do not just read the letter, act on Leigh’s request for change. May Leigh’s desperation/plight evoke REAL change. That is her wish. It can only happen if we act on her instructions.
3) I struggled with the decision to publish her letter. I would never just publish a suicide note arbitrarily. I generally include family members, friends, those closest to the person. The benefits HAVE to outweigh the risks or I would never publish it. There are many things I have decided not to publish if the risks are too great, benefits minimal. I truly believe that Leigh’s last wishes can be made manifest by the action steps outlined in the solution section.
Thank you all for caring so deeply about this lovely woman and may she live on in each of us.
Dr. Sundem’s suicide is a tragedy, and clearly she was in a tremendous amount of emotional pain. Her suicide note along with her postscripts are evidence of her pain along with many distortions of thought process. It is truly sad that she was unable to get the right help that would have averted her suicide. Nonetheless, it is a tremendous oversimplification to assert that her suicide was caused by not “matching” for a residency slot and even worse implying that the problem is a systemic one predicated on discrimination against her for her past drug use and felony convictions. While that may have been a significant stressor for her, augmented by discrimination that was real with intent, that still does not confer causality nor excuse the fact that Dr. Sundem must still own her own choices. Suicide is always tragic and it should be a lesson to all of us the the human condition is frail. None is us succeeds in life without help from others. But suicide is not the evidence that allows one to blame systems regardless of how flawed they really are. The issue here is the not the process of residency match and whether US graduates versus foreign graduates are treated differently. The issue here is that a person – who happened to be a physician – was struggling with her life’s circumstances and felt completely alone and without any other options available other that suicide. This would be sad for anyone in any profession. And we should be motivated to consider how we might help anyone, and everyone, in similar circumstances – regardless of profession.
Appreciate your thoughts and certainly suicides are complex. Suicide notes are helpful in understanding what the person was experiencing and it appears that if Leigh had an employed position as a doctor she would have been able to generate an income, pay her mounting debt, and begin to live her life (hopefully date, have a family, and achieve personal goals). However, being unmatched limited her ability to do any of this and so we lost a wonderful physician (I’ve spoken to several of her colleagues who were very impressed with her). She saw no way out and became more desperate and departed this planet far too soon. Given the number of unmatched doctors who have felt similarly (passively suicidal) it is imperative that we act now to correct a system that leaves > 1000 new doctors each year without employment. The “mismatch” IS a systemic problem and must be addressed. Discrimination/stigma within medicine IS a systemic issue as well given the ADA non-compliant mental health questions on medical board licensing applications. Minimizing these systemic factors that obstructed Dr. Leigh Sundem from practicing medicine does nothing to solve the underlying issues that lead to many, many desperate doctors (I know because I run a suicide helpline and get an earful of despair from many regarding these system-wide issues).
Just curious what you think is the modifiable central issue that could have been addressed before her tragic ending?
So loved, she deserved better. She gave it her all. The system sucks. Such a young and loving person who gave her all to everyone above herself. Love you and will be missed forever.
The situation in this country with the match and the lack of options for one who fails to match are horrible, I agree. I have friends who failed to get in to US medical schools, went to Caribbean schools without being well educated about how difficult it would be to match, and are now several years out of med school with no job, horrific debts, etc. It’s a problem.
I also have incredible sympathy for Leigh and her family. As someone who has been depressed and suicidal while in medical school as well as at the start of residency I know how hopeless things can feel .
But – I don’t think she is a good illustration of the problem with the match. I think she’s a good illustration of high-achieving students who are not honest with themselves and don’t listen to the advice they are given by their mentors. Obviously, I don’t know what Leigh’s school did or did not tell her. But I do know that initially applying to match in orthopedics with these red flags on her application and no back-up specialty was a mistake. She then matched into a surgical prelim year and tried the match for a second time – applying for EM, another incredibly competitive residency.
You say here her lifelong passion was helping patients in recovery – why then was she not applying for psychiatry, a field that would have likely been incredibly sympathetic to her unique background and deals often with patients in recovery? Or family medicine, or IM?
This is not to blame her for her suicide – I think she committed suicide because she had clinical depression and was at the end of her rope. But I’m not sure the match and prejudice are really to blame either. I think we need to be honest about what goes on with some of these applicants who don’t match, because if we aren’t it dilutes the message.
Agree. Complex situation. Multifactorial issues predating the tragic end to what could have been a fulfilling career in medicine. Regarding her interests in medicine, she over the years expressed a desire (early on in her CSPAN speech I believe) to pursue infectious disease, help the underserved, and then eventually settled on ortho as her primary interest. I wonder if she applied for FM/IM initially whether this could have been prevented.
I’m just wondering if anyone is willing to address the portion of her letter where she discusses her knowledge of her white female priviledge during parts of her training? Racial discrimination in all aspects of the US medical education, training, and corporate structure is rampant and careers are ruined very often in POC with spotless records and strong academic profile due to technicalities or being disliked by a particular attending.( I have many examples of this in friends and family members) Discrimination in medicine comes in many forms but it seems like she also wanted to bring this issue to light. In addition are there any suicide statistics for physicians by race? AA are the most oppressed group in this country and Im just wondering if there is a baseline of increased coping mechanisms in this group due to higher need for resiliency? Thanks
I can relate to Leigh in so many ways, I’m in my 30’s with no hope of ever getting married or having a family, stopped communication with all my friends and family because of embarrassment of talking about my failures and listening to their perfect lives, everyone had such high expectations of me and now I have nothing to show for, I have sacrificed my life to follow my dream of becoming a physician, yet I have been struggling with taking my USMLEs. I am an American that went to med school outside of the US and they never trained us for USMLE, now I’m 3 years after graduation, still studying for them, and I’ve had so many moments of hopelessness and just wanting to give up in life…like her I don’t want to die but becoming a doctor has always been my dream that any other path is not an option, I know I will not be happy with any other career, medicine is my passion. Today I came across this post and I think it’s a sign because I’ve spent all day sitting on my couch crying, unable to move or get up to even eat. I totally get mental illness, have been taking antidepressants for years that I actually don’t think have worked but now I’m too scared to stop taking them. I don’t know who to reach for help, like I said I’m too embarassed to talk to anyone and have zero friends, my parents have been very supportive but they don’t know what im going through and I don’t want them to worry about me so talking to them about my feelings is not possible. knowing that im not the only one going thru this is a little comforting but I’m scared I’m going to end up like Leigh because even though I don’t have a criminal record I see we relate in a lot of things. I guess I feel a little better and might be able to get some sleep, but how will I get through tomorrow? hopefully I’ll have the willingness to open my books and study for those damn tests. Thank you for sharing her story, rest in peace beautiful Leigh.
I’d love to help you. Please contact me here with the answers to these 7 self-reflective questions at the end of this post: Secrets to loving your life in healthcare. You have more choices than you know. Often it just helps to take a step back and look at the big picture with the help of some mentors who understand. Please don’t give up your precious life.
A-Contact Pamela asap/pdq and listen and learn and talk and teach. I, too, can respond as possible. See my recent post. Medicine is not the toughest but one of the toughest professions. Numbers are but the start. Stand out and above the crowd. Platitudes but what it is. Number 1 is you must take care of yourself before you can take care of anyone else. Consider options as there are many options in the allied health care field with less sacrifice of self and of sanity. Thousands of US/Canadians study abroad and have for many decades. Many of those schools are going nowhere, especially not here. Take that in mind as you explore alternatives. We all are alone in ourselves but not outside, so be aware and reach out to find someone capable of responding and initiating. As my grandfather used to say, you can learn from anyone even the elevator operator, and he was right on. Learning and teaching is a daily joy. Cheers.
Thank you so much for the work you do. I knew Leigh very well, loved her and was there in the undergrad years when she was applying to med schools. She helped us so much with our collegiate recovery program and used her story to change the admissions process. Please let me know if there is any way to support your work in her name.
I was young and foolish at that time: the first time I took the FLEX (shows my age) I didn’t study. Missed passing by 1% – you’d assume I learned my lesson. My first taking of the Psychiatry written boards the same scenario took place. Then I got disgusted with myself such that once I was invited to take the Oral Board I trained very hard with a kind Doctor, practically memorizing the Diagnostic & statistical manual. For many of us this is a calling. I have been in dark places and am no cheerleader. But for what it’s worth, checkered as my own career is, Doctor I wish you the best. Believe in yourself (this from a fellow with poor self image! haha)
I’m in the middle of a meeting now that includes the APA medical director and President. I raised the question about long range ideas to help unmatched and other disenfranchised docs & the response was: working toward loan forgiveness, and also to try and match applicants to those Psychiatry programs that have trouble filling residency training positions. We MDs/DOs must help each other out! Hope
Seems like a Band-Aid maneuver. Though I do think anything helps.
Why are her notes dated 2019? If her death was exasperated by COVID, wouldn’t that be 2020?
She lost her last potential job as a result of the pandemic. Wound care in nursing homes. Nursing homes closed down to all visitors. Her student loans were coming due. Often passive suicidal thoughts can persist for some time. An inciting event can create the “perfect storm” and lead someone to the tragic impulsive decision.
05/16/2020@0851h-g’morn Pamela, I did read Leigh’s letter/notes
a couple days ago, screaming for awareness for legitimacy for sanity for reality, and
their core struck me hard. Meeting Leigh and conducting her interview, all it took was
my innate sentient nature to recognize who and what was responding and initiating with me…
05/17/2020@1123h-Pamela, after reading Leigh’s notes, again, a couple of points of note for me are ‘enough is enough’, NO, emphatically NO, by that moment of acheivement enough is TOO much, and Leigh was her own sacrificial object as no one, apparently, taught her to take care of Number 1 FIRST in order to be able to take of the rest. One of my frequent truisms is We have to grow up; we do not have to finish; do not finish; play every day; go to Never Land and return to reality. When the going gets tough the tough … NO, before the tough get going, Stop Breathe Think Act. Gather information and make the best move knowing it may alter with more knowledge. Leigh wasted away needlessly due to system pathology, as well you know. Leigh had Leader all over herself for others. In my career I am pressed hard to think of a male physician who could stand next to Leigh. A hard loss.
Thank you for posting… I am deeply disturbed by the situations medical school graduates find themselves in. Although the Match was never a particular concern for me, I have helped many who were unmatched work on a match strategy and on their applications. The distress they are in is palpable. We need to do something about this issue. There must be action, and I’m here to help… Please contact me to conference, strategize, etc. I see there is a problem, and I’d like to be part of the solution.
Write to the NRMP/ACGME and would recommend a broad discussion among medical trainees. There must be a better way.
saddened by this, but being an intern in medicine in a rural area I can tell you I have two fellow interns in my class that have felonies and both pardoned, so it is possible to land a residency in less desirable area though it can unfortunately take years and resources. It took 5 and 3 years from medical school graduation while one had a narcotic abuse issue at his previous residency and he had a harder time landing a residency, since he has a ding on his residency and medical license. He has to be spot drug screened often, and other monthly reporting to the state medical licensing board. So it is possible but very hard.
My concern Dr. Wible is that as an intern that was involved in many codes with covid patients already, is the act of bringing med students in earlier will increase their stressors, and will those who did not match find medical institutions less open to hiring people, like most graduating residents are telling me that hospitals are instituting hiring freezes. I am worried about incoming interns, as my class of interns were put though the caldron and we can say that we were the ones taking care of covid patients many times with inadequate PPE, yet some how we made it, thanks to our support networks. But it is these interns with their selflessness, that must, as I came to understand, that a modicum of self-centric thinking is required to survive intern year: weather it be duty hour abuses, bullying, or difficulty finding PPE to see covid patients. I am worried that covid will affect primary care providers the most as I can tell you with complete respect to other providers and residents we were running the hospital when many if not most sub-specialists and surgeons whether they were attendings or residents were not. This country has a shortage of primary care providers and I would not like to see residency burnout during the covid pandemic affect those numbers any further. I am hopeful I can support the incoming class of interns as a PGY2 with their work to decrease burn out. I agree with most and believe that programs should interview in waves and any seat remaining in each subsequent wave not filled should move to the next wave. First wave should be all MD’s, second DO’s, US FMG/IMG, and finaly non-US FMG/IMG. Other may disagree but our medical education was set up for Americans, and specifically those that got MD’s. Also I believe that we need to have NRMP and ERAS provide the data of those who failed match be brought in to help with the state of emergency that we have, I can tell you my abs were cramping from doing so many compressions. These would be emergency residency slots that all hospitals would be open to accepting, as each residency slot is supported by medicare/medicaid to the tune of 150-200k and they only pay a fraction of that back to the residents. Instead of asking medical students and interns to start early, IMMEDIATELY provide residency slots to all those that are match capable in ERAS but have not matched. I also leave the caveat, I know that this is my wishful thinking, thus we must still know all these unmatched individuals and reach out to them as they will be further stressed by being on the sidelines, when they are calling health care workers hero’s, personally I would rather have more support in terms of more primary care residents and ppe.
Thank you Old Red—EXTREMELY Helpful information!
What a wonderful piece, Pamela. Medicine has turned into the “profession that just keeps abusing.” Despite that, I love it, although I feel that is more because of a Stockholm syndrome than anything rational.
I’ve been open on the net about my failure to match in Neurosurgery, and I could have just as easily ended up in a similar situation as Leigh. Fortunately, I found a happy home and wonderful career in interventional radiology.
The lack of accountability of medical schools for their graduates’ welfare, particularly when saddled with this degree of debt is egregious, and when 4th year is devoted to interviews and applications with little educational value is disgusting. Failure to match should not be a career death sentence.
In a sense, I hold 1) medical schools accountable. NO medical student truly understands what failure to match means until they go through it. Also, 2) the largesse GME has shown to “educating the world’s doctors” makes sense – only if your own citizens have been accounted for, like the Australian example. I know that this is a hot topic and a bit of a litmus test. But its killing people – proof positive – read the letter.
I feel terrible for Leigh. This one could and should have been saved.
Just off the phone with a mom who has a son unmatched after a dream to pursue neurosurgery. 400K debt. Must be addressed. We can’ just allow these wonderful skilled people to sit at home unemployed when we have a doctor shortage. Thank you for your insight. Leigh has helped us start a long overdue conversation.
I just found this, while trying to figure out if I had any hope. It’s clear that I’m not alone and something needs to change, but the system is the system. How could I ever change it? Maybe one day it will change but right now medical regulatory bodies even overseas don’t care about us, particularly us medical students but also practitioners. They don’t see us as humans. The next class will come. We are a number.
I mean I’ve tried to fight, look for hope but it sometimes gets too much. When is enough, enough?
I know I sound hopeless (I mean I am) but I am glad I read this. It gave me peace with where my mind is racing. It makes me so happy that at least there are a few people in medicine recognizing a need for this to change. I hope it will, but I am certain that it won’t for me.
I honestly wish nothing but the very best, happiness and success for all future medical students/doctors. I am sure you will all be incredible, just please make sure not to make a legal mistake. You’ll forever hate yourself if you screw this up, particularly when you really truly know it was the only thing you ever wanted to do with your life and even more when you know you would have been amazing at it because patient care is what drives you.
Finally, thank you Leigh for allowing your letters to be published and giving a fellow medical student some peace that this fight will be fought whether he is around or not. You have more strength sharing your story through your letters than I do, as my shame makes it impossible for me to even tell family or friends. I know they will find out through someone else but I am done trying to control the narrative. I am not being heard anyway.
I could keep going, who knows, but if not I’ll see you on the other side. I don’t even know why I’m writing this. I guess I just found a place I could be accepted for what I feel and could do so anonymously. Maybe I feel like I’m speaking to you (Leigh) by writing this and am assuring you I feel your pain. However, the last thing I want people to think is that this is a cry for a help. It’s not. It’s my job to deal with the consequences of my life. I should’ve known better I just wish there was another path.
Anyhow I’ll shut up. If anyone sees this comment please know that, I am finally ok. I finally feel peace. if you read this just fight for your peers don’t try and competitively tear them down and treat medical students and doctors like humans who make mistakes. Look at all doctors and medical students as people who care and love what they do no matter how they’ve screwed up. Med school was so grueling I would never have kept fighting if I didn’t truly love every second of being with patients. It’s the thought of not ever being able to do that which will kill me. Only I’m to blame but carry on with love in your hearts and fight for your peers.
Please reach out for help as there are many many pathways forward and I have helped med students & doctors launch successful health practices (with or without a medical license). I actually “retired” mine and I am more effective in my healing arts practice that ever. Never give up your precious life and dream for “perceived insurmountable obstacles.”
Ahhh and you can always reach me here. Happy to call you.