
Physician-Friendly States for Mental Health: A Review of Medical Boards
Research Project by Pamela Wible, M.D., and Arianna Palermini, OMS2
© Copyright 2019
Read updated version of article (& download PDF) in peer-review journal dedicated to physician mental health.
Addendum: Updated mental health questions by state are listed at the end of this article.
OBJECTIVE
Do medical boards undermine physician mental health by breaching physician confidentiality and privacy? We analyze the initial medical licensing process in each state to determine if qualified applicants who report mental illness experience discrimination. We then identify the most favorable states for physician mental health.
INTRODUCTION
Could a pediatrician in marriage counseling 10 years ago be mandated to disclose her therapy records to the state board? Yes. Could a dermatologist with postpartum depression 3 years ago be required to defend her competence before the board? Yes. Should a medical student worry that a licensing board might read his psychological evaluation for test anxiety? Yes.
State medical boards may access applicants’ confidential health records and require that all three individuals defend their competence to practice medicine. Are medical boards injuring physicians by violating their rights? Many say yes.
“Why are mental health questions still allowed to be on there?” asks a physician. “I have had postpartum anxiety/depression three times now and I feel like it is none of their damn business. So I have lied about it on my applications. Also, I feel these questions could contribute to doctors not seeking help, especially for serious problems that could require a mental health hospitalization. Do these questions have an adverse effect on doctors and medical students presenting (or not) for care they may desperately need?”
We all desire competent, healthy doctors who deliver excellent patient care. State medical boards exist to protect the health, safety, and welfare of patients through licensing, investigating, and disciplining physicians. Their mission is to protect the public from impaired physicians, yet medical boards may be impairing physicians’ access to confidential compassionate health care by subjecting doctors to mental health questions that violate United States law.
“After reading an article about one woman’s journey through hell after being honest on those application questions, I sought care an hour away. I drove an hour in another direction to nervously fill prescriptions for antidepressants,” reports a physician. “I required several meds to stop thinking of suicide all day every day. My suicidal thoughts were 100% work-related.”
BACKGROUND
Suicide is an occupational hazard of the medical profession. (1) Though students enter medicine with their mental health on par with or better than their peers, they are three times more likely to kill themselves, according to the American Medical Student Association. In some residency programs 75% of interns meet criteria for major depression. (2) Suicide risk increases with untreated mental illness. Physicians who die by suicide are less likely to be receiving mental health care compared with nonphysician suicides. Physicians are more likely to self-medicate for anxiety, depression, and suicidality—with tragic outcomes.
Doctors are reported to have the highest suicide rate of any profession—even higher than the military—according to findings presented at the 2018 American Psychiatric Association annual meeting. (3)
What’s causing our physician mental health crisis?
Physicians are routinely exposed to tragedy and death resulting in occupationally induced anxiety, depression, and PTSD. Yet doctors receive no routine on-the-job support. Instead, they risk punishment when asking for help. State boards, hospitals, and insurance companies interrogate doctors about their mental health, read their confidential medical records, and then deny health plan participation, medical liability coverage, hospital privileges, and state licensure. Doctors with occupational distress may be referred to PHPs (Physician Health Programs) where they are required to participate in 12-step addiction recovery with witnessed random urine drug screens—even when they have never used drugs:
“I’m amazed at the punitive terms I’ve had to face in recovering professionally from a depressive episode for which I was hospitalized last year,” reports a psychiatrist. “One of my requirements is to be urine tested for substance abuse, despite multiple demeaning assessments that have rendered the clear verdict that I don’t have a substance use problem. I’ve had to attend costly treatments for ‘professionals’ in which I am the only female in a group of male physicians who have had sex with their patients or have become assaultive with staff. Any efforts on my part to point out that I don’t quite ‘fit’ are taken as further evidence of my pathology. I’m a single parent as well, so that each of these ‘treatments’ I’m required to attend takes me away from my two children for extended periods of time. Throughout all of this, nobody has told me how common my feelings are—that a large number of doctors feel depressed and suicidal at times. Rather, I’ve been told that my actions are unheard of for someone in mental health and may preclude me from ever providing therapy again since ‘we tell patients to never give up hope, but you did.’ Hopefully, in the near future this won’t be a taboo subject, and there will be places for those like me to seek responsible and confidential care.”
While PHPs have been effective for some physicians with substance abuse, physicians have also died by suicide under the care of these programs. (4) PHPs hold a monopoly in the provision of state-board-sanctioned physician assistance services in most states. To avoid punishment by PHPs and boards (that may restrict licensure and publish doctors’ mental health diagnoses online) physicians drive hundreds of miles out of town, use fake names, and pay cash for off-the-grid care.
“I’ve been in practice 20 years and have been on antidepressants and anxiolytics for all of that time,” explains one doctor. “I drive 300 miles to seek care and always pay cash. I am forced to lie on my state relicensing every year. There is no way in hell I would ever disclose this to the medical board—they are not our friends.”
Results from a 7-year investigation of 1,300 physician suicides reveal that doctors (and medical students) die by suicide due to fear of seeking care that would be disclosed on their applications for residency, hospital privileges, and state licensure. Fear of seeking treatment leads to delayed diagnoses thereby increasing anxiety, depression, substance abuse, and suicide. (5)
“Do you know what really hurts? The fact that anyone can look me up on the Internet and read my dirty laundry,” explains one doctor. “I’m publicly shamed [by my medical board], punished for being ill. I will only know peace when I am gone.”
The AMA Code of Medical Ethics upholds the right of confidentiality for all seeking health care. A therapeutic alliance requires trust to allow full disclosure of sensitive and personal information. Individuals receiving care believe their medical records will be safeguarded and only released with their consent. Physicians hold confidentiality sacred and take an oath to preserve it at all costs. Physicians are understandably shocked when their own personal health information is accessed by employers, hospitals, and medical boards under the pretense of “public safety.”
HIPAA (Health Insurance Portability and Accountability Act) provides data privacy and security provisions to safeguard medical information for all US citizens. Information about health status, provision of health care, or payment for health care that is collected by a covered entity (such as a doctor or health center) and can be linked to an individual is PHI (Protected Health Information) under federal law. Though physicians must uphold patient HIPAA rights or face harsh penalties, physicians are expected to waive their own HIPAA rights to medical institutions such as state boards.
The Americans with Disabilities Act of 1990 states: “No covered entity shall discriminate against a qualified individual on the basis of disability in regard to job application procedures, the hiring, advancement, or discharge of employees, employee compensation, job training, and other terms, conditions, and privileges of employment.” Yet competent physicians suffer repeated invasion of privacy and discrimination by medical institutions in violation of the ADA.
METHODS
We queried via social media and emailed 6,000 US physicians: “Have you ever faced discrimination, limitation of license, or delay/denial of your medical license due to mental health issues?” A selection of de-identified submissions are published with permission. We analyzed each medical board’s initial licensing application to evaluate mental health questions by state. Most applications were accessed online or by portable document format. When only available through a portal, a login was created. When an application was unavailable or no mental health question was identified, the board was contacted by email and/or phone to confirm the absence or presence of mental health questions and verify wording when present. All mental health and impairment questions were organized on a spreadsheet to compare quantity and quality of questions. Substance use queries were removed to focus on non-drug-related mental health questions. We italicized key mental health phrases for ease of reading and graded states based on invasiveness of mental health questions into five categories A through F.
Grade A: States with no mental health questions or one or two straightforward current impairment question(s) that do not mention mental health.
Grade B: States with progressive mental health question(s) linked to current impairment.
Grade C: States with mental health question(s) spanning the last 5 years.
Grade D: States with “have-you-ever” questions related to mental health, mental health questions beyond 5 years, or a requirement for peer reference on applicant’s mental health.
Grade F: States with highly invasive mental health questions unlinked to current impairment that contain confusing, punitive, or adversarial language.
RESULTS
GRADE A STATES
Grade A: States with no mental health questions or one or two straightforward current impairment question(s) that do not mention mental health.
13 States: Connecticut, Hawaii, Indiana, Kentucky, New Jersey, Maine, Maryland, Massachusetts, Michigan, Nevada, New York, Pennsylvania, Wyoming
Connecticut, Hawaii, Michigan and New York are the most physician-friendly of all states with no mental health or impairment questions.
Indiana asks: “Do you have any condition or impairment (including a history of alcohol or substance abuse) that currently interferes, or if left untreated may interfere, with your ability to practice medicine in a competent and professional manner?”
Kentucky asks: “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgement or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner?”
New Jersey and Maryland both ask the same impairment questions: “Do you have any reason to believe that you would pose a risk to the safety or well being of your patients? Are you able to perform the essential functions of a practitioner in your area of practice with or without reasonable accommodation?”
Maine asks: “Are you physically and mentally able to perform all the essential functions or services necessary to exercise the privileges or services applied for with or without reasonable accommodation? Are you able to perform these functions without significant risk or injury to yourself or others?”
Massachusetts has one straightforward question: “Do you have a medical or physical condition that currently impairs your ability to practice medicine?”
Nevada asks: “Do you currently have a medical condition which in any way impairs or limits your ability to practice medicine with reasonable safety and skill? If you currently have a medical condition which in any way impairs or limits your ability to practice medicine, is that impairment or limitation reduced or ameliorated because of the field of practice, the setting, the manner in which you have chosen to practice, or by any other reasonable accommodation?”
Pennsylvania asks only about drug-related impairment: “Do you currently engage in or have you ever engaged in the intemperate or habitual use or abuse of narcotics, hallucinogens, or other drugs or substances that may impair judgement or coordination?”
Wyoming has no direct mental health questions, though reference must answer: “Does the applicant’s health allow for the safe and competent practice of medicine?”
GRADE B STATES
Grade B: States with progressive mental health question(s) linked to current impairment.
12 States: Illinois, Iowa, Minnesota, Missouri, New Mexico, North Carolina, South Carolina, South Dakota, Tennessee, Vermont, Virginia, Wisconsin
Illinois asks: “Do you now have any disease or condition that presently limits your ability to perform the essential functions of your profession, including any disease or condition generally regarded as chronic by the medical community, i.e., (1) mental or emotional disease or condition; (2) alcohol or other substance abuse; (3) physical disease or condition? If yes, attach a detailed statement, including an explanation whether or not you are currently under treatment.”
Iowa asks: “Do you presently have a physical, mental or emotional condition (including alcohol or drug dependence), or do you presently engage in the use of illegal substances that affects or is reasonably likely to affect your ability to perform your professional duties appropriately or which could adversely affect the quality of care rendered by you to patients or jeopardize the safety of patients?”
Missouri asks the same questions as Illinois though adds sexual disorder: “Do you currently have any condition or impairment which in any way affects your ability to practice in a professional, competent and safe manner, including but not limited to: (1) a mental, emotional, nervous or sexual disorder, (2) an alcohol or substance abuse disorder or (3) a physical disease or condition?”
States such as Missouri have updated their questions to avoid stigmatizing physician mental health:
“I have experienced discrimination and delay in getting my Missouri medical license due to my mental illness,” reports a psychiatrist. “I have bipolar disorder in remission for years. Never affected my ability to practice (my only mental illness which has affected my ability to practice has been my PTSD secondary to being a physician, ha!). Years ago the Missouri application asked whether you were diagnosed with a ‘psychotic disorder?’ and it had schizophrenia and bipolar disorder in parenthesis. So of course I had to answer yes. As a result I had to undergo an additional yearly evaluation by my psychiatrist and he had to write a letter to the board saying that I was safe to practice medicine even though I have a ‘psychotic disorder.’ My license was always delayed and it was a nightmare renewing every year. Now the Missouri board has removed that question so they must have caught some heat. But I felt very violated and targeted with that question.”
Minnesota and New Mexico ask the same questions: “Do you have a physical or mental condition that would affect your ability, with or without reasonable accommodation, to provide appropriate care to patients and otherwise perform the essential functions of a practitioner in your area of practice without posing a health or safety risk to your patients? If yes, what accommodations would help you provide appropriate care to patients and perform other essential functions?”
North Carolina asks: “Do you currently have any medical, chemical dependency or psychiatric condition that might adversely affect your ability to practice medicine or surgery or to perform the essential functions of your position?”
“I was sued,” reports an emergency physician. “Overwhelmed with grief and fear, I took antidepressants and saw a psychiatrist. I paid cash and considered using a false name. I had already seen the North Carolina Medical Board send a physician to 6 weeks of inpatient alcohol treatment due to a complaint without any proof he was drinking. That saved his license but he owed an astronomical bill.”
South Carolina asks: “Are you currently being treated for any physical, mental or emotional condition that might interfere with your ability to competently and safely perform the essential functions of practice as a physician?”
South Dakota asks: “Do you have a physical or mental condition which would preclude you from performing the essential functions of your practice, job, or in the exercise of practice privileges, with or without reasonable accommodation? Regardless of how this question is answered, the application will be processed in the usual manner. If you have answered this question affirmatively and are found to be professionally qualified for licensure or medical staff privileges requested, you will be given an opportunity to meet with the appropriate entity to determine what accommodations are necessary or feasible to allow you to practice safely.”
Tennessee asks: “Do you currently have any physical or psychological limitations or impairments caused by an existing medical condition which are reduced or ameliorated by ongoing treatment or monitoring, or the field of practice, the setting or the manner in which you have chosen to practice? Tennessee also asks: “Have you ever been diagnosed as having or have you ever been treated for pedophilia, exhibitionism, voyeurism or other diagnosis of a predatory nature?” (Reference Grade B Section end note on predatory/criminal behaviors).
Vermont has a “Medical condition, treatment, use of chemicals or illegal substances” section that begins with definitions: “The ‘ability to practice medicine’ is a term that includes: 1. The cognitive capacity to make and exercise reasoned medical judgments, and to learn and keep abreast of medical developments; 2. The ability to communicate those judgments and medical information to patients and other health care providers, with or without the use of aids or devices, such as voice amplifiers; and 3. The physical capacity to perform medical tasks and procedures, with or without the use of devices, such as corrective lenses or hearing aids. ‘Medical conditions’ includes physiological, mental or psychological conditions with a non-comprehensive list that includes emotional and mental illnesses, learning disabilities, drug addiction, and alcoholism. ‘Currently’ means recently enough to have a real or perceived impact on one’s functioning as a medical professional. ‘Chemical substances’ means alcohol, drugs (legal and illegal), and prescribed medications.” This section has three main questions, each with a follow-up question and place to upload relevant documents. All focus on current impairment. Two relate to substance use and the other reads: “Do you have a medical condition that in any way impairs your ability to practice medicine in your field of practice with reasonable skill and safety?”
Virginia asks: “Do you currently have any mental health condition or impairment that affects or limits your ability to perform any of the obligations and responsibilities of professional practice in a safe and competent manner? ‘Currently’ means recently enough so that the condition could reasonably have an impact on your ability to function as a practicing physician.”
Wisconsin has five impairment questions: “Do you have a medical condition, which in any way impairs or limits your ability to practice medicine with reasonable skill and safety?” Follow-up questions are: “If yes, are the limitations or impairments caused by your medical condition reduced or ameliorated because you receive ongoing treatment (with or without medications) or participate in a monitoring programs?” and “If yes, are the limitations or impairments caused by your medical condition reduced or ameliorated because of the field of practice, the setting, or the manner in which you have chosen to practice?” The fourth question is related chemical substance impairment and final question: “Have you ever been diagnosed as having or have you ever been treated for pedophilia, exhibitionism, voyeurism?”
Note: Tennessee and Wisconsin have a similar question on criminal/predatory behavior (pedophilia, exhibitionism, voyeurism) as do Alabama, Ohio, Mississippi, and Washington. Medical boards must protect patients from criminal behavior and we do not penalize states for these questions.
GRADE C STATES
Grade C: States with mental health question(s) spanning the last 5 years
9 States: Arizona, Colorado, Idaho, North Dakota, Ohio, Oklahoma, Oregon, Texas, Utah
Arizona lists mental health questions in “Confidential Questions.” The primary question: “Have you received treatment within the last five years for use of alcohol or a controlled substance, prescription-only drug, or dangerous drug or narcotic or a physical, mental, emotional, or nervous disorder or condition that currently affects your ability to exercise the judgment and skills of a medical professional? If so, provide the following: A.) A detailed description of the use, disorder, or condition; and B.) An explanation of whether the use, disorder, or condition is reduced or ameliorated because you receive ongoing treatment and if so, the name and contact information for all current treatment providers and for all monitoring or support programs in which you are currently participating. C.) A copy of any public or confidential agreement or order relating to the use, disorder, or condition, issued by a licensing agency or health care institution within the last five years, if applicable.”
Colorado asks: “Within past 5 years, have you engaged in any conduct or exhibited any behaviors that resulted in an impairment in your ability to practice in a safe, competent, ethical and professional manner?”
Idaho asks three impairment questions. One relates to legal/illegal drug use during last five years. The others are: “Do you currently have or have you had any serious physical or mental condition in past 5 years which in any way may impair or limit your ability to practice medicine with reasonable skill and safety?” and “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgement or that would otherwise adversely affect your ability to practice medicine in a competent, ethical, and professional manner?”
North Dakota asks: “Within the last two years have you been treated for any physical, mental or emotional condition which impaired or could be said to impair your ability to practice medicine safely and competently?
Ohio asks four mental health questions. The first three are: “In the past five years, have you been diagnosed as having, or been hospitalized for a medical condition which in any way impairs or limits your ability to practice medicine with reasonable skill and safety? Are the limitations or impairments caused by your medical condition reduced or ameliorated because you receive ongoing treatment or received treatment in the past (with or without medication) or participate in a monitoring program? Are the limitations or impairments caused by your medical condition reduced or ameliorated because of the field of practice, the setting, or the manner in which you have chosen to practice? If you receive such ongoing treatment or participate in such monitoring program the board will make an individualized assessment of the nature, severity, and duration of the risk associated with an ongoing medical condition. Have each treating physician submit a letter detailing the dates of treatment, diagnosis, and prognosis.” A final question is: “Have you ever been diagnosed as having, or have been treated for, pedophilia, exhibitionism, or voyeurism?” (Reference end note Grade B section on predatory/criminal behaviors).
Oklahoma asks: “Do you currently have or have you had within the past two years any mental or physical disorder or condition, which, if untreated, could affect your ability to practice competently?”
Oregon has three mental health questions. The first: “Within the past two years, have you participated in a program other than the OHPSP for evaluation, monitoring, or treatment for ANY issue in lieu of or as a condition of resolving a matter before a health care program or facility or a regulatory or licensing board or has such action been pending or proposed? “Issue” includes, but is not limited to, substance use, communication, or boundary issues. (if “yes” provide full details and dates to include the name and location of the diversion program, regulatory Board, healthcare program or facility, and/or court, and reasons for and results of entering the program).”
The second: “Do you currently have, or have you had within the past two years, any physical, mental, or emotional condition which impaired or does impair your ability to practice your health care profession safely and competently? The final question: “Within the past two years, have you been admitted to any hospital or other treatment facility for any physical, mental or emotional condition or substance use disorder which impaired or does impair your ability to practice your health care profession safely and competently? (If yes to either, provide full details and name of healthcare professional providing treatment. Request the healthcare professional send directly to the Board a statement regarding the ability to safely practice medicine.)”
Texas has a “Mental and Physical Health” section with five questions with mandatory submission of another form for any affirmative answer. The first three relate to self-referral to the Texas Physicians Health Program, substance use within past five years, and physical/neurologic condition impairments within five years. The mental health question is: “Within the past five years, have you been diagnosed with or treated for any: psychotic disorder, delusional disorder, mood disorder, major depression, personality disorder, or any other mental health condition which impaired or does impair your behavior, judgment, or ability to function in school or work? If you answered ‘Yes’ are the limitations caused by your mental condition or substance abuse/dependency problem reduced or ameliorated because you receive ongoing treatment (with or without medication) or because you participate in a monitoring program?”
“I am applying for my Texas license and I feel my rights are being violated,” reports one internist. “I have well-managed depression. I was asked do you have a mental condition—yes, and then I was asked does it affect how you function at work—no. I thought that would be the end of it, but now I need a treating physician statement, a statement from my program director, and I need to justify why I said no to it not affecting how I function at work. I’m required to list all my medications from the past 5 years and all physicians who have treated me. How is this not a HIPAA violation? Why are they still allowed to do this? My application has been flagged as ‘impaired’ and needs to go before the board and people who have never met me will decide if I am a danger to my patients. I have no money for a lawyer. If I fight this it can delay my license and my being able to work. My friends with no medical issues were approved months ago and here I am still waiting.”
Utah asks: “If you are licensed in the occupation/profession for which you are applying, would you pose a direct threat to yourself, to your patients or clients, or to the public health, safety, or welfare because of any circumstance or condition? Have you ever been declared by any court or competent jurisdiction incompetent by reason of mental defect or disease and not restored? Utah’s one “have-you-ever” question is far less invasive than those in Grade D section.
GRADE D STATES
Grade D: States with “have-you-ever” questions related to mental health, mental health questions beyond 5 years, or a requirement for peer reference on applicant’s mental health.
9 States: Arkansas, California, Georgia, Kansas, Louisiana, Montana, Nebraska, New Hampshire, West Virginia
Arkansas asks: “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your ability to practice medicine or to perform professional or medical staff duties in a competent, ethical, and professional manner? If yes, explain. “Are you currently, or have you ever been monitored by a Physician Health Committee in any state? If yes, explain, and ask the Physician Health Committee to send documentation of your status.”
California has a “practice impairment or limitations” section with six questions related to substance use, addiction, and mental/physical health. Four are “have-you-ever” questions. Two relate to mental health: “Have you ever been diagnosed with an emotional, mental, or behavioral disorder that may impair your ability to practice medicine safely?” and “Have you ever been enrolled in, required to enter into, or participated in any drug, alcohol, or substance abuse recovery program or impaired practitioner program?”
Non-impaired physicians have been mandated to impaired practitioner programs as retaliation. These programs (PHPs), governed by the Federation of State Physician Health Programs, exist under private contracts in all states except California, Nebraska, and Wisconsin.
“PHPs remain largely non-compliant with ADA laws and regulatory guidelines in assessing medical and psychiatric fitness of physicians,” reports an occupational medicine specialist. They receive revenue from contracts with physician employers and residency programs plus referred medical students/physicians who pay costly out-of-pocket fees or risk career destruction. Physician employers liberally refer to PHPs for virtually any reason. PHPs even encourage third-party referrals. Aggrieved spouses, jilted lovers, market competitors have all successfully required PHP evaluations of physicians.”
Georgia has no impairment or mental health questions though requires three peer references to answer: “Does this physician have, or has this physician had in the past, any mental or physical illnesses or personal problems that interfere with his/her medical practice?” Unlike the single Wyoming (Grade A) peer reference, Georgia requires multiple colleagues to reveal any mental health issue at any time in the life of a physician peer including past personal problems.
Such questions pose barriers to seeking mental health care and create collegial distrust when physicians fear revealing their struggles with peers who may report them to boards.
“Isn’t it more appropriate to ask a reference about a physician’s knowledge, reliability, integrity—performance?” asks an internist. “Mental health questions have a chilling effect that I admit have kept me from seeking mental health support when it would have been wise to do so. Stigma is so severe that I have heard many physicians state that it would be better to die from suicide than be admitted to our hospital’s psychiatric unit.”
“My psychiatrist requested I report to the Georgia Medical Board my inpatient care for a major depressive disorder,” explains one physician. “They stamped a 5-year private consent order on me whereby I had to submit to random urines (though there was no history of substance abuse). If I knew what I would be subjected to over the next 5 years and the expense of hundreds of urines, I would not have fulfilled his request. The toughest challenge was getting through the red tape with hospital privileges when they found out I had been treated for depression. I know dozens of physicians under psychiatric care for depression. They dare not relay such to the Board secondary to what I endured.”
Kansas has four impairment questions. The first: “Within the last 2 years have you been diagnosed or treated for any physical, emotional or mental illness or disease, including drug addiction or alcohol dependency, which limited your ability to practice the healing arts with reasonable skill and safety?” The second on self-medicating: “Within the last 2 years have you used controlled substances, which were obtained illegally or which were not obtained pursuant to a valid prescription order or which were not taken following the directions of a licensed health care provider?” The third: “Have you ever practiced your profession while any physical or mental disability, loss of motor skill or use of drugs or alcohol impaired your ability to practice with reasonable safety?” Given residency widespread sleep-deprivation impairment (and use of stimulants) during residency, nearly all physicians (if responding honestly) would admit yes. The final question: “Do you presently have any physical or mental problems or disabilities which could affect your ability to competently practice your profession?”
“I used samples of Paxil and had my spouse write me prescriptions for Lexapro, Buspar, Paxil, and sleeping pills over the years,” reports one physician. “I did not trust other doctors. I did not want any of this stuff in my records as I did not want to be seen as ‘crazy’ (this is how many doctors refer to psychiatric patients).”
Louisiana asks: “In the last 10 years prior to this application have you had any physical injury or disease or mental illness or impairment, which could reasonably be expected to affect your ability to practice medicine or other health profession?
Montana asks: “Have you ever been diagnosed with a physical condition or mental health disorder involving potential health risk to the public? Have you any physical or mental condition(s) which may have or had adversely affected your ability to practice this profession, included but not limited to a contagious or infectious disease involving risk to the public? If yes, attach a detailed explanation.”
Nebraska asks “Do you currently, or have you had, any physical, mental, or emotional condition which impaired, or does impair your ability to practice your health care profession safely and competently? Within the last 5 years, has any licensing agency or credentialing organization initiated any inquiry into your physical, mental or emotional health?” As noted previously, inquiries can be retaliatory and the question posed by Nebraska would imply physician guilt for having psychological needs.
New Hampshire asks: “Have you ever had any physical, emotional, or mental illness which has impaired or would be likely to impair your ability to practice medicine? A physician with postpartum depression decades ago must answer yes leading to invasion of privacy unlinked to current impairment.
West Virginia asks: “Have you had any interruption in your practice of medicine which might reasonably be expected by an objective person to currently impair your ability to carry out the duties and responsibilities of the medical profession in a manner consistent with standards of conduct for the medical profession?” and “Have you ever had anything occur which might reasonably be expected by an objective person to currently impair your ability to carry out the duties and responsibilities of the medical profession in a manner consistent with standards of conduct for the medical profession?” Though West Virginia mental health questions focus on current impairment and are preferable to the wording of all other states graded D, we have placed West Virginia in this category due to “have-you-ever” questions.
GRADE F STATES
Grade F: States with highly invasive mental health questions unlinked to current impairment that contain confusing, punitive, or adversarial language.
7 States: Alabama, Alaska, Delaware, Florida, Mississippi, Rhode Island, Washington
Alabama asks three mental health questions. The first: “Within the past 5 years, have you ever raised the issue of consumption of drugs or alcohol or the issue of a mental, emotional, nervous, or behavioral disorder or condition as a defense, mitigation, or explanation for your actions in the course of any administrative or judicial proceedings or investigation; any inquiry or other proceeding; or any proposed termination by an educational institution; employer; government agency; professional organization; or licensing authority?” The second: “Have you ever been diagnosed as having or have you ever been treated for pedophilia, exhibitionism, or voyeurism?” and finally: “Are you currently engaged in the excessive use of alcohol, controlled substances, or the illegal use of drugs, or received any therapy or treatment for alcohol or drug use, sexual boundary issues or mental health issues?
The application explains: “The term ‘currently’ does not mean on the day of, or even in the weeks or months preceding the completion of this application. Rather it means recently enough so that the condition referred to may have an ongoing impact on one’s functioning as a physician within the past two years.” We wonder why the application did not instead read within the last two years.
The last question suggests that applicants must reveal if they have ever received any therapy for mental health issues regardless of impairment. For this reason, Alabama is graded F.
Alaska ranks worst of all states with 25 yes-or-no questions related to mental health, many invasive “have-you-ever-had” questions unlinked to current impairment. The first: “Has your ability to practice medicine in a competent and safe manner ever been impaired or limited by any condition, behavior, impairment, or limitation of a physical, mental, or emotional nature?” Alaska also asks: “Since completing your postgraduate training, have you ever been physically or mentally unable to practice medicine for a period of sixty (60) [days] or longer?” The most invasive mental health question we found on any application is: “Have you ever been diagnosed with, treated for, or do you currently have: followed by a list of 14 mental health conditions including depression, seasonal affective disorder, and “any condition requiring chronic medical or behavioral treatment.”
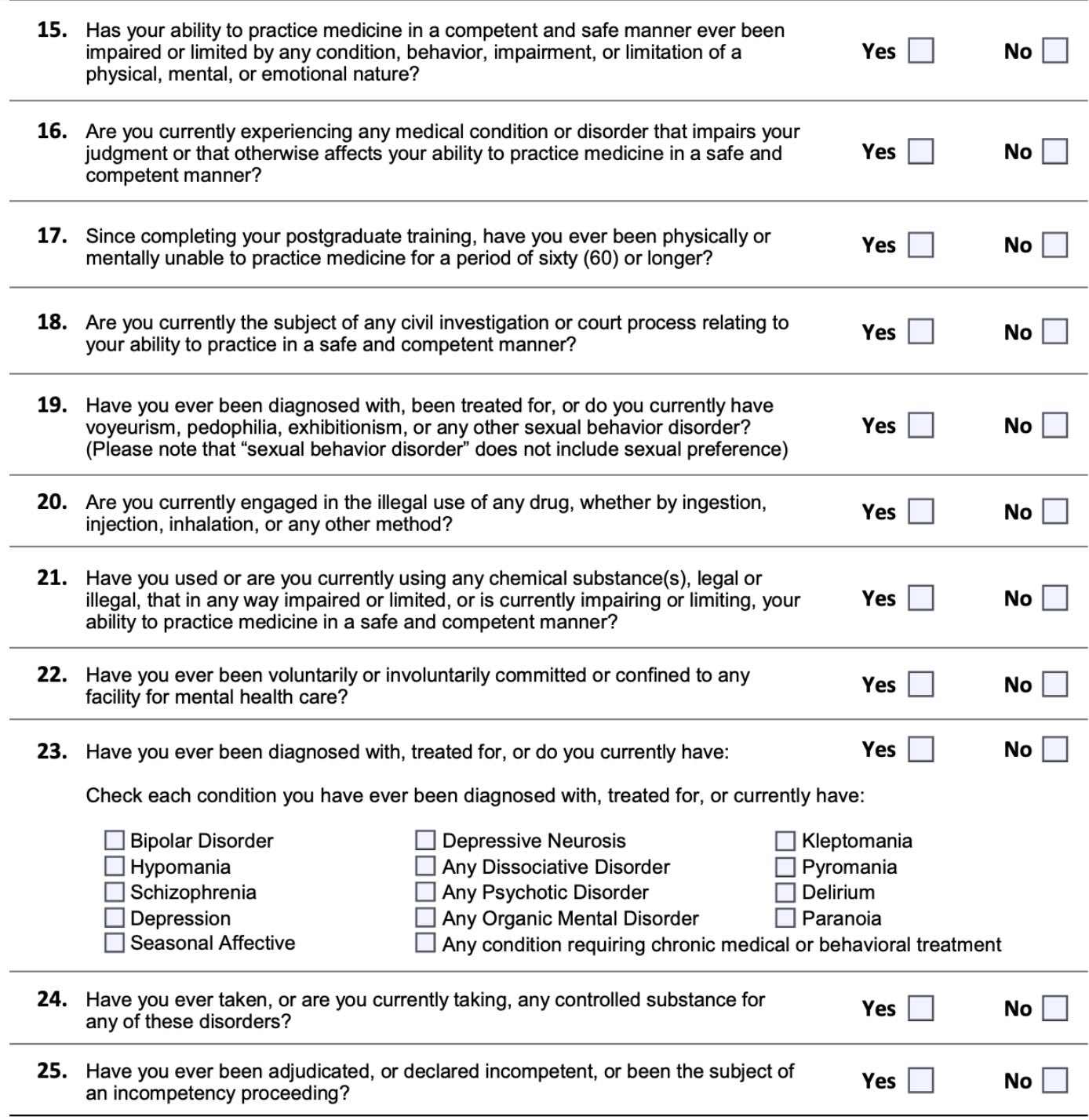
Alaska Medical Board Licensing Application 2019
“In residency I had to do a rotation in Alaska,” reports a hospitalist. “The application asked if I had ever been on psychotropic medications or in counseling. I had taken Zoloft 12.5 mg for 90 days due to anticipatory anxiety about starting intern year. Fortunately, my fears weren’t realized, so I stopped the medication when the prescription expired. I had also gone to counseling in my fourth year of medical school for a separate relationship issue. So, I answered both questions affirmatively. This resulted in my having to ‘defend’ myself to a panel of people on the Alaska medical board over the phone. They granted my license, but it was a humiliating experience—and definitely created barriers to my seeking care moving forward—both because I have not wanted to be in a position to have to answer those types of questions affirmatively, and due to financial barriers because I will not use insurance to defray costs of counseling since that may be ‘discoverable.’ What a horrible culture of shame those questions create!”
Delaware begins with the same question as Alabama: “Within the past 5 years, have you ever raised the issue of consumption of drugs or alcohol or the issue of a mental, emotional, nervous, or behavioral disorder or condition as a defense, mitigation, or explanation for your actions in the course of any administrative or judicial proceedings or investigation; any inquiry or other proceeding; or any proposed termination by an educational institution; employer; governmental agency; professional organization; or licensing authority?”
Two follow-up questions include: “Are such current conditions or impairments reduced or ameliorated because of ongoing treatment (with or without medication) or participation in a monitoring program or because of the field of practice, the setting, or the manner in which you have chosen to practice medicine?” and “Do you have a mental or physical disability that limits your ability to practice medicine in a fully competent and professional manner with safety to patients? If yes, are you willing to accept a conditional or limited license to practice medicine if it is possible to accommodate such disability?”
Final question: “Do you agree to submit to an examination at your own expense if the Executive Director of the Board of Medical Licensure and Discipline deems it necessary to determine whether your physical and/or mental impairment presents a significant risk to the health or safety of patients or otherwise causes you not to be fully qualified to practice medicine in a competent and professional manner with safety to patients without limitations or accommodations? If no, submit a signed, notarized statement fully explaining your answer.”
Delaware’s application makes an anticipatory request that physicians waive their confidentiality/HIPAA rights and submit to an impairment exam at their own expense before the board reviews the application or meets with the physician.
Florida has six questions. Three relate to substance use and one to physical impairment. Two mental health questions are: “In the last five years, have you been admitted or referred to a hospital, facility or impaired practitioner program for the treatment of a diagnosed mental disorder or impairment?” and “During the past five years, have you been treated for or had a recurrence of a diagnosed mental health disorder that has impaired your ability to practice medicine?” Neither focus on current impairment.
An affirmative answer to any question requires: “A self-explanation providing accurate details that include names of all physicians, therapists, counselors, hospitals, institutions, and/or clinics where you received treatment and dates of treatment. A report directed to the Florida Board of Medicine from each treatment provider about your treatment, medications, and dates of treatment. If applicable, include DSM III R/DSM IV/DSM IV-TR Axis I and II diagnosis(es) code(s), admission and discharge summary(s).”
“When I applied for my Florida license it was delayed by months,” reports a gynecologist. “I was required to have a psych evaluation by an ‘approved’ doctor due my history of depression which was treated and well managed. It fell under the ‘impaired physician’ program and definitely was stigmatizing. To this day I don’t answer those questions honestly anymore and am hesitant to seek treatment as needed.”
“After the unexpected death of a patient, I sought counseling. By a stroke of (bad) luck, I picked the only one in town in charge of impaired physician monitoring. He told the board (though stable) I should be ‘monitored.’ I had to defend myself in front of the Florida board. They laughed in my face and then posted in the local newspapers that I was sentenced to 5 yrs of monitoring. I had mandatory Wednesday group therapy. Though I was an exemplary physician, my employers had to be told why I was unavailable for call every Wednesday. Each time I (re)credential with hospitals, I must explain the whole thing again. HIPAA for me does not exist. I have never missed a single day of work for mental health.
Mississippi application forces physicians to waive all confidentiality and HIPAA rights plus consent to a mental exam at applicant’s expense:
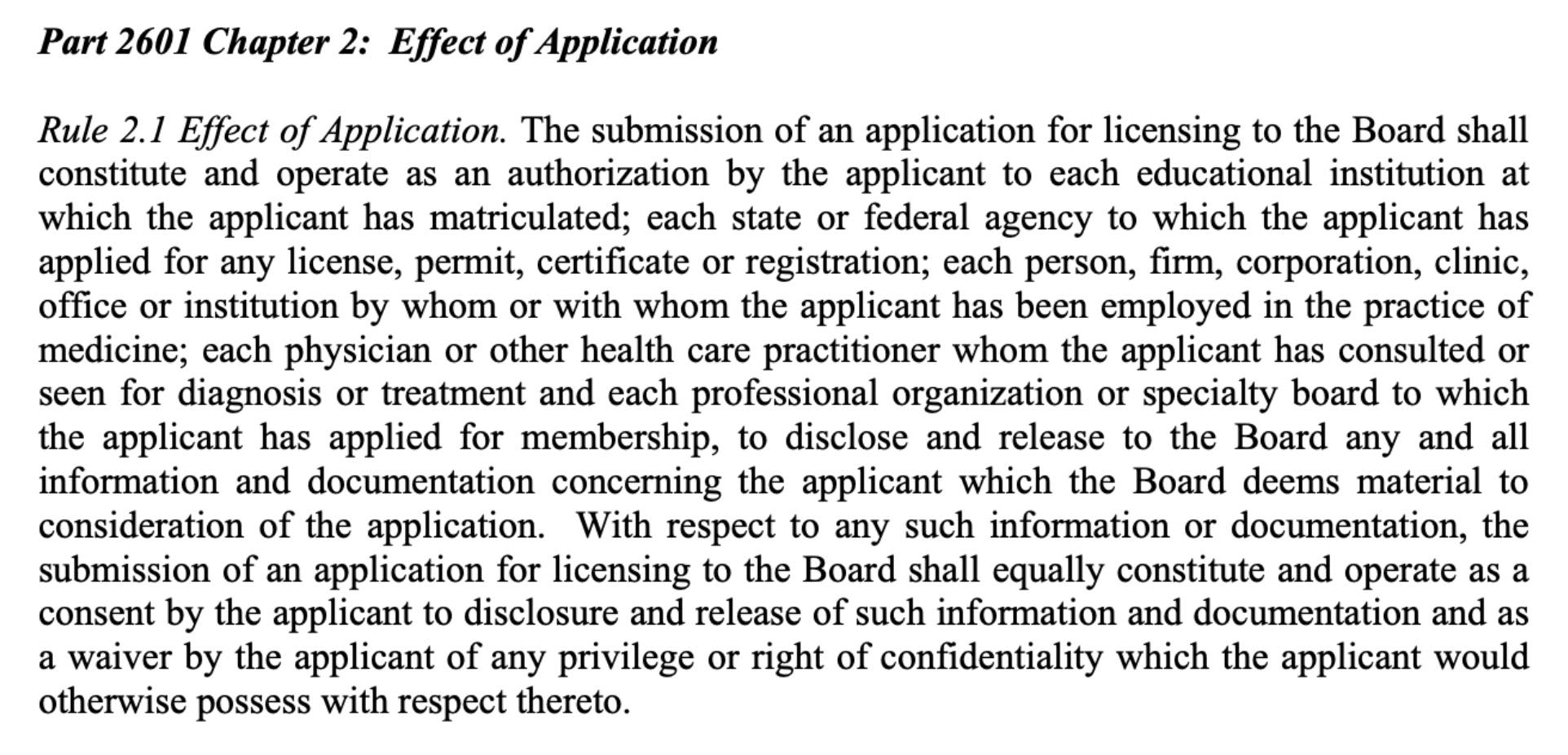
Mississippi Medical Board Licensing Application 2019
Similar to Delaware, Mississippi has this additional paragraph: “By submission of an application for licensing to the Board, an applicant shall be deemed to have given his or her consent to submit to physical or mental examinations if, when and in the manner so directed by the Board and to waive all objections as to the admissibility or disclosure of findings, reports or recommendations pertaining thereto on the grounds of privileges provided by law. The expense of such examination shall be borne by the applicant.”
Mississippi also asks: “Have you ever been diagnosed as having, or have you ever been treated for, pedophilia, exhibitionism, or voyeurism, bipolar disorder, sexual disorder, schizophrenia, paranoia or other psychiatric disorder?”
Given the forced breach of confidentiality, forced consent to exam, and have-you-ever been diagnosed with mental health conditions such as bipolar disorder unlinked to current impairment, Mississippi is graded F.
Rhode Island has no current impairment questions; however, there are two questions that may preclude a physician who suffered retaliation for a mental health condition during training from receiving a medical license. The first: “During any Professional/Medical Education were you ever dismissed, suspended, restricted, put on probation, or otherwise acted against or did you take a leave of absence for medical reasons?” The second: “During any Post Graduate Training, were you ever dismissed, suspended, restricted, put on probation, or otherwise acted against or did you take a leave of absence for medical reasons?” Having to defend a leave of absence for medical reasons that may have happened decades ago revictimizes physicians who have experienced punishment/retaliation for occupationally induced mental health conditions.
“When I became overwhelmed with abuse I was facing in residency, I begged my program director with tears running down my face for emergency mental health care,” reports an anesthesiologist. “I spent the next few days isolated, confused, exhausted on my couch. I saw a counselor. I started an antidepressant for the first time in my 30 years of existence. By the weekend I felt refreshed with a glimmer of hope. When my program asked to meet with me on Monday, I was sure it was to see if I was okay, to ensure I had no thoughts of self-harm or suicide. I was wrong. The meeting was to let me know I was placed on 6 months probation for being unprofessional. I was flabbergasted, my mouth literally fell open. I couldn’t believe I was sitting in front of the people I trusted with my education and they were able to look at me in my greatest time of need and anguish knowing I was now in counseling and on medication and respond only with punishment.”
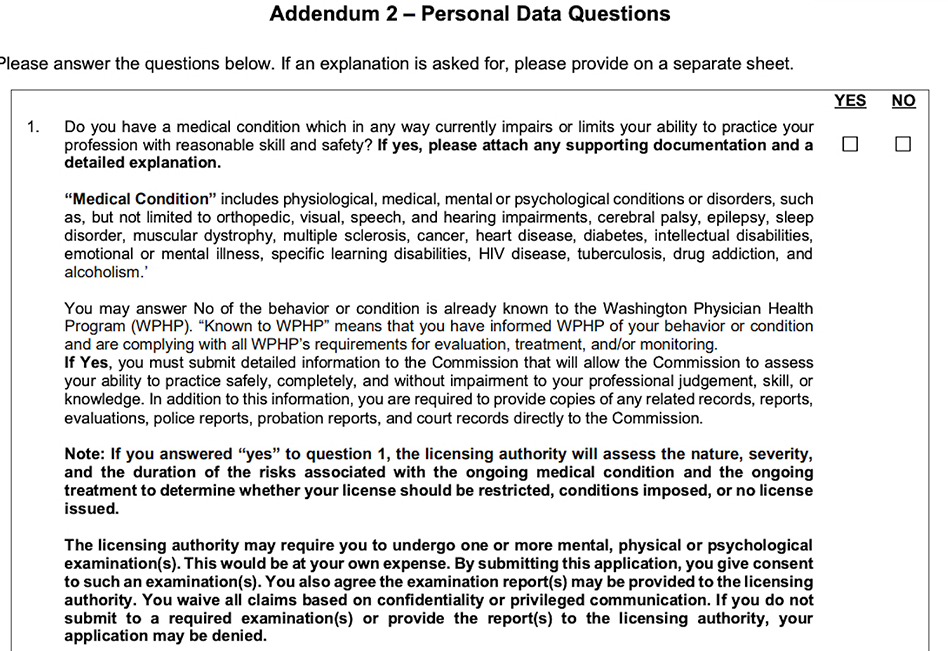
Washington has “Personal Data Questions” that cover mental health, substance use, and criminal/predatory behavior with a list of impairing medical conditions that match the Vermont application.
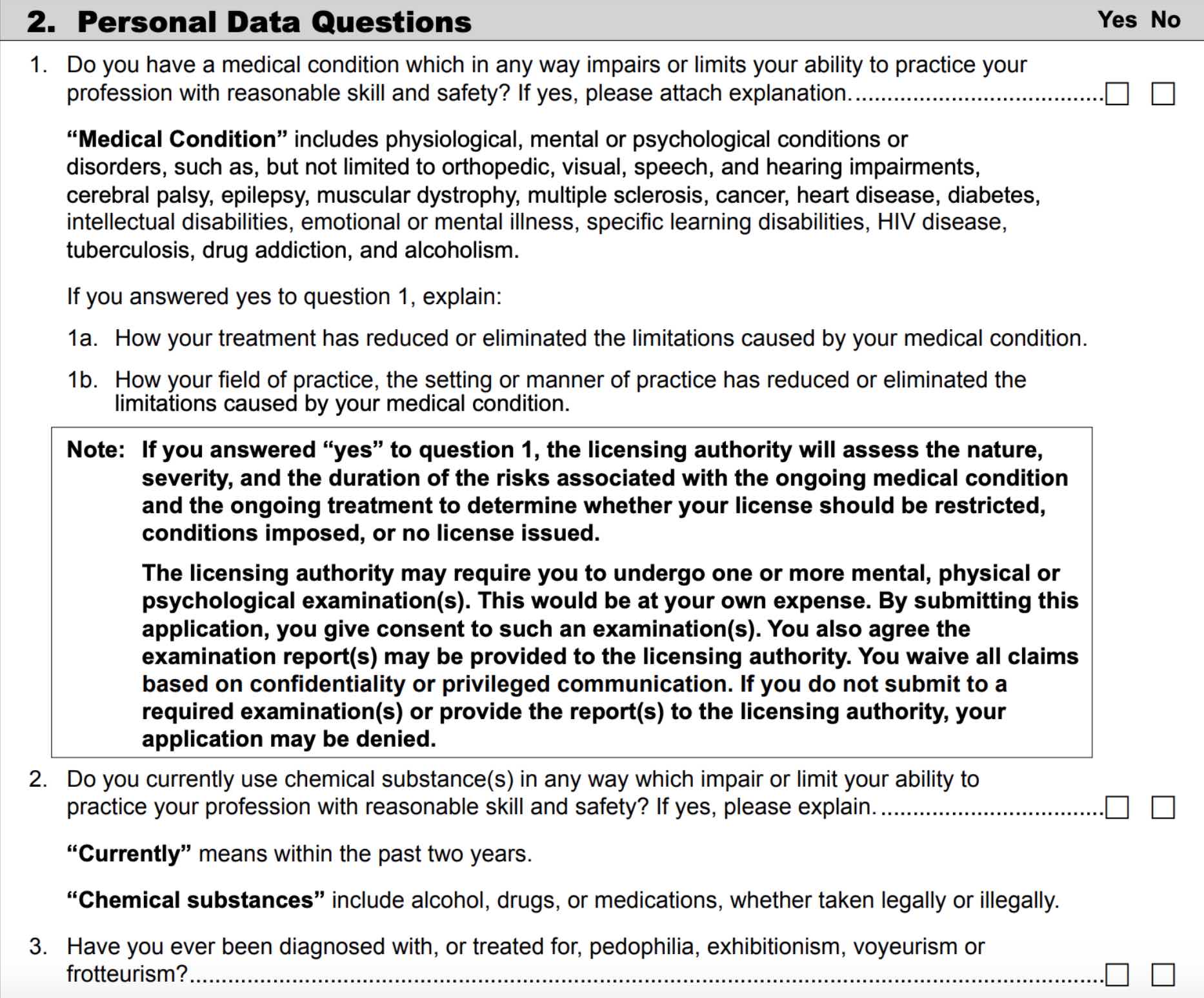
Washington Medical Board Licensing Application
Though Washington asks about medical conditions linked to current impairment and rightfully screens physicians for predatory/criminal behavior, we find the threatening language in the black box to be concerning including the forced breach of an applicant’s confidentiality and privacy.
DISCUSSION
The Federation of State Medical Boards (FSMB) defines impairment as a physical, mental, or substance-related disorder that interferes with a physician’s ability to undertake professional activities competently and safely. (6) The FSMB focus is the individual impaired physician. But what causes the impairment? Has the impairment been fixed?
“Taking medication for ADHD is analogous to wearing glasses for my nearsightedness,” reports a psychiatrist. “My state licensing question asks, ‘Do you have a condition that could impact your abilities?’ As long as I am wearing my glasses I can see. As long as I am taking my ADHD medicine I can keep fairly focused. What business is it of theirs? Normally I feel guilty for lying about the slightest thing. I was counseled behind closed doors by a faculty who knew of my struggles with ADHD to simply put “no” on the form and leave it at that. This proved to be good advice. I was raised to be extremely honest about everything. When it comes to completing these questions for licensing I believe I am being honest because I was instructed by my respected faculty member to look at the questions in this light: Are you impaired by your condition? No. Then the answer on the application is NO.”
Many states treat illness as impairment. According to the FSMB: “Some regulatory agencies equate “illness” (i.e., addiction or depression) as synonymous with “impairment.” Physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years. This is a critically important distinction. Illness is the existence of a disease. Impairment is a functional classification and implies the inability of the person affected by disease to perform specific activities.” (6)
FSMB believes illness precedes impairment and that physicians may at any point fall into the continuum of inability to practice medicine competently and safely.
Medical board intervention is always directed at the physician, not the system. But what if the system causes physician impairment? Case in point: Resident physicians are legally forced to work 28-hour shifts (or longer due to unenforced caps). (9) Working just 17 hours is equivalent to the cognitive and psychomotor impairment of a 0.05% blood alcohol content (illegal to drive in Utah and most Western European countries). Working beyond 24 hours is equivalent to a 0.10% blood alcohol content (exceeding the 0.08% legal limit to drive in 49 states). Impairment escalates along a continuum and is noted even at 10 hours. (8) Sleep-deprivation-related cognitive and psychomotor impairment leads to medical mistakes and fatal car accidents after long hospital shifts. (9)
Professional boards are tasked with protecting the public. To prevent pilot fatigue resulting in impairment-related plane crashes, the NTSB (National Transportation Safety Board) limits maximum flight time to 9 hours during the day or 8 hours at night. Why force physicians to work three times that amount?
As a guardian of public safety, medical boards (like transportation boards) must address work conditions that currently impair more than 130,000 US resident physicians. (7) Given our physician shortage, boards should protect physicians from sleep-deprivation-related seizures, hallucinations, psychosis and death inside our hospitals. We can’t afford to lose one more doctor.
Beyond sleep deprivation, physicians are injured by chronic violations of their human rights in hazardous workplaces due to overworking (an 80-100 hours work week is equivalent to 2 to 3 full-time jobs), food/water deprivation, bullying, harassment, discrimination, and punishment when sick (including lack of confidential mental health care). (5) Late-stage effects of these violations are substance abuse and mental illness.
Rather than address the systemic cause of physician impairment, medical boards too often revictimize victims.
Some board questions seem more voyeuristic and predatory than helpful, exploiting vulnerable physicians for profit. Fine-print warnings threaten hefty fines for “intentional or inadvertent non-disclosure” leading naively honest physicians to overshare intimate confidential information when they present no danger to patients. One affirmative answer creates a cascade effect in which non-impaired physicians may land in 5-year addiction recovery programs (even though they have never used drugs). When one state denies or limits licensure, others mirror the action. One positive response to a mental health question may follow an applicant for life.
CONCLUSION
Medical boards do undermine physician mental health by breaching physician confidentiality and privacy. Discrimination against qualified, competent applicants who report mental health conditions is a violation of the Americans with Disabilities Act. In their search for criminal behavior among physicians, medical boards must not become criminal in their own behavior. By breaking federal law and the AMA Code of Ethics, boards have weaponized mental health diagnoses against physicians. Recommendations for all state boards:
1) Remove mental health questions from medical licensing applications. Replace with current impairment questions such as: “Do you currently have a condition that impairs your ability to practice medicine safely?” Comply with federal law by following best practices of Grade A states. Move criminal/predatory behavior queries to the criminal section alongside felonies and DUIs.
2) Address impairment from hazardous working conditions. Rather than focus on individual victims, engage in high-yield activities that resolve hazardous conditions impairing physicians en masse. To truly protect patients, align with all other industries invested in public safety that have legislated (and enforced) maximum 16-hour shifts, 60-hour work weeks, with minimum 30-minute breaks every 8 hours.
3) Encourage nonpunitive 100% confidential mental health care. Physicians require safe, accessible mental health care to be well-adjusted human beings. Most physicians enter medicine as humanitarians with noble intentions. Help them be well. After all, how can physicians give patients the care they’ve never received?
“Physicians are treated as criminals and tracked more closely than Level III sex offenders,” reports a general surgeon. “Answering all these questions on applications, the subtle, unspoken lesson is ‘you had better be squeaky clean, mentally, morally and physically! If you step off the shining path, bad things will occur.’ I have known 7 male physicians who died by suicide. Most with a ‘happy’ exterior. Why? They cannot confide in colleagues for fear that their colleagues will turn them in to hospitals and boards—and there goes their privileges and livelihood. They cannot confide in their spouses because during rough patches mentally, their marriages are already in trouble. If they share psychological problems, they probably fear that the wife may use this as ammunition in any future divorce. So they keep on smiling—right up to the hour they die.”
Even until their last breath, physicians retain their work ethic. Some doctors are completing chart notes, returning lab results, and checking in on hospitalized patients in the hours before their suicides.(5)
By injuring physicians, we aren’t protecting the public.
Let’s end the physician mental health witch hunt.
© Copyright 2019 Pamela Wible, M.D.
For authorization to reprint, contact author.
___________________________________________
REFERENCES
(1) Vogel, L. CMAJ. 2018 Jun 18; 190(24): E752-E753 Has suicide become an occupational hazard of practicing medicine?
(2) Pereira-Lima, K. Academic Medicine: 2019 Jun; 94(6): 869-875 Residency Program Factors Associated With Depressive Symptoms in Internal Medicine Interns: A Prospective Cohort Study
(3) 2018 American Psychiatric Association annual meeting. Doctors’ Suicide Rate Highest of Any Profession
(4) Wible, P. Medscape. 2015 Aug 28. Do Physician Health Programs Increase Physician Suicides?
(5) Wible, P. 2019. Human Rights Violations in Medicine: A-to-Z Action Guide
(6) Federation of State Medical Boards, Policy on Physician Impairment. 2011
(7) AAMC Workforce Data Report. ACGME Residents and Fellows by Sex and Specialty, 2017
(8) Dawson D, Reid K. Nature. 1997;388(6639): 235. Fatigue, Alcohol and Performance Impairment
(9) Wible, P. 2017 Mar 10. Sleep-deprived doctors disclose hospital horrors
Addendum: Updated mental health questions by state are listed below.
Many states are updating mental health questions to reflect more progressive wording directed to current competence. On August 19, 2020, this addendum is added to alert readers of changes in medical licensing applications. Authors have found that often there is a delay between approval of updated wording and when new questions are actually in use on licensing applications. Relevant dates are noted below.
North Carolina replaced their mental health questions with an advisory statement on September, 17, 2018. At the time of publication, authors did not find this advisory statement. On August 3, 2020, authors were made aware that the new advisory statement was in use and this was confirmed on their website.
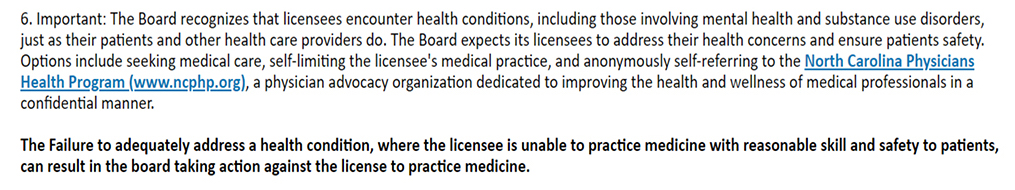
Washington has updated their mental health question to reflect current impairment. Current is defined as within the past six months. At the time of publication, the prior personal data questions were still in use. On August, 6. 2020, authors found the Washington Medical Commission addendum through the FSMB to reflect these new questions effective July, 2020.
Note from physician in Minnesota: Here is the newly advertised language for Minnesota (to be implemented by Jan 1, 2022):












Excellent article. When was this survey undertaken please? Very important to know in order to learn whether the unanimous 2018 FSMB HOD resolution regarding these ADA impermissible questions has been acted upon by any significant number of states. Many are making the assumption that “all is well” after that resolution…but reports certainly suggest otherwise.
Also, although the licensure questions are an excellent starting point in the analysis of whether Medical Licensing Boards (MLBs) and are violating the ADA, as your vignettes poignantly illustrate, many of them with the enthusiastic assistance of their Physician Health Programs (PHPs) are flagrantly violating that law in their POST licensure procedures. For example, the “cookie cutter” handling of physicians who are ‘regarded as’ disabled on the basis of self-referral for burnout, referrals by residency programs for ostensible behavioral issues, referrals by hospitals as a part of sham peer review, referrals by employers for the same reason or in a genuine belief that something could be gained by PHP ‘counseling’, and perhaps most reprehensible, false and malicious complaints by vindictive employees, spouses and even patients.
Thanks Louise. Survey was done in June & July, 2019. Absolutely agree that post-licensing assaults to physician human rights continue in a variety of forms that were beyond the reach of the already-extensive 8,643-word article. I cover many of those human rights violations in medicine in my recent book (pub June 2019) as noted in reference #5.
In essence, we had to start somewhere so began with initial licensing applications by state. Clearly, mental health diagnoses have been weaponized against doctors. I also learned through interviewing many non-impaired fully competent physician respondents from various states that their mental health issues (though stable and well-managed) were considered an automatic “red flag” on applications. They had to go through the impaired physician protocol for flagged applications and many were placed in mandatory monitoring for substance use/abuse. Previously, I never understood why. Seems boards/PHPs/FSMB/FSPHPs believe that (1) “illness predates impairment” (it’s just a matter of time) and that (2) physicians with any mental health issues are HIGH RISK for substance use/abuse so just enroll them in 12-step programs as a “preventive” measure. Not evidence-based medicine.
Have you ever thought to recommend that a woman with postpartum depression begin a preventive 5-year 12-step program?
So ludicrous.
Thanks, Pamela. So glad you did this and VERY helpful to know the time frame given the pubic perception that the problem is now SOLVED because FSMB passed a non-binding resolution discouraging use of the ADA impermissible questions by MLBs. Not faulting you for not covering the waterfront; just want everyone to realize that this massive expose is really just the tip of the iceberg.
I have reposted on Linked In. (“Who in their right mind would practice in these states?”
And no, of course it is reprehensible and indefensible to send anyone with any pure depression into any 12 step program, let alone one preceded by 90 day inpatient hospitalization and followed by 5 years of forensic drug monitoring, as we both know and we and others are witnessing and publicizing more and more frequently.
It is a violation of human and civil rights and medical ethics on so many fronts , and the only reason that it continues to happen is that naive physicians trust that their boards are fair and that PHPs are there to help them. They do not get knowledgeable professional defense counsel with ADA expertise IMMEDIATELY upon any indication of interest by an MLB or its PHP, and they live to regret it. That is if they choose to live, after their livelihoods (and for physicians these are often synonymous) are stripped from them by these unscrupulous entities under the guise of “protecting patient safety”.
Quite the rabbit hole. . . Thank YOU for all you do to help physicians who are suffering. Let’s keep digging. And reporting. Curious what you feel is the #1 best route to protect the rights of those who are being victimized? Victim awareness? More JD/MD (DO) force? Removing illegal questions and helping PHPs and medical boards align with the law? What route do you see as the most high yield given the ongoing suffering and suicides within medicine. I’ve always felt a sense of urgency related to preventing suicides among my colleagues. I’m sure you feel the same.
I believe it is victim awareness and activism. If every physician were to read this column before applying for licensure/renewal and parse the questions carefully, answering honestly only those that can legally be asked; and follow up on the suggestion that if their state’s questions are suspect under the ADA they forward them to the US DOJ Civil Rights section with a cc to the Bazelon Center; and if contacted by the MLB or the PHP regarding any matter that could possibly affect their licensure immediately contact their malpractice carrier regarding coverage and (regardless) obtain ADA knowledgeable licensure defense counsel; and never “go along to get along” simply because they know they are innocent, or well, or not impaired, but rather seek all avenues of review and redress of any unjustified decisions being foisted upon them; and to be open and honest about ALL of the experiences (both positive and negative) they have had, or been witness to in this arena with anyone who will listen, especially members of the public who are losing sources of medical care; and prevail upon their legislators to critically study the practices of the institutions in their state that are driving physicians out of practice and sometimes to suicide; thus shedding daylight on suspect practices that heretofore have been shrouded in secrecy and shame, allowing them to propagate unfettered; then we would finally begin to make inroads into a system that has been making it unsafe for physicians to obtain needed preventive and supportive self care for the several decades since it became apparent that enormous profits can be derived from forcing “deep pocket” physicians into exorbitant and medically unjustifiable rehabilitation programs under the exaggerated guise of “protecting patient safety”.
The actions and words of just one person can be extremely effective.
Case in point: “As a chair of a large academic department of anesthesiology, I am frequently asked to complete credentialing [reference] forms . . . I recently received one such form that I found concerning. Among the various questions to which I was asked to respond was one asking if the provider had ever received treatment for mental health-related issues. As I completed the form, I circled the offending question and inserted my concerns that this is the type of question that creates barriers to health care professionals seeking mental health care services. Having made my point I submitted the form, assuming that was the last I would hear of it. Surprisingly, a couple of weeks later I received an email from a member of the facility’s credentialing committee asking to speak with me to better understand my concern. I contacted him and was pleasantly surprised by his immediate acknowledgement of my concern. He asked how they could improve the question, and I suggested they could put it in the context of inquiring as to current limitation of the ability to provide care, in place of their all-encompassing “ever” qualifier. He promised to make the change to the question and thanked me for pointing it out.” ~ Ronald L. Harter, M.D.American Society of Anesthesiologists Monitor, Aug 2019 Administrative Update “Making a Difference”
We need MORE of this kind of activism. Simple. Effective.
It also continues to happen because those physicians who do enter the system and get treatment become ‘dented cans’; if they raise concerns and/or objections about their treatment, few are willing to listen and take them seriously because they are seen as ‘the problem’.
CURRENT IMPAIRMENT is the coin of the realm if state medical boards want to avoid violating federal disability statutes. State boards have fought back since the 1990’s by defining certain medical and psychiatric conditions, or history of same, as inconsistent with being a “qualified person”. That argument usually fails currently. The other approach used by boards is saying that these physicians pose a “direct threat”. But “direct threat” is a term of art in the ADA. Here is the definition:
” “Direct threat” means a significant risk of substantial harm that cannot be eliminated or reduced by reasonable accommodation. 29 C.F.R. §1630.2(r)(1998). Direct threat determinations must be based on an individualized assessment of the individual’s present ability to safely perform the essential functions of the job, considering a reasonable medical judgment relying on the most current medical knowledge and/or best available objective evidence. Id. To determine whether an employee poses a direct threat, the following factors should be considered: (1) the duration of the risk; (2) the nature and severity of the potential harm; (3) the likelihood that potential harm will occur; and, (4) the imminence of the potential harm.”
The attempts to make “direct threat” arguments against physicians has been mainly clumsy and heavily-influenced by the quality of expert testimony and the handling of “junk science”.
Tom
The assumption that all illness predates impairment is another wild assertion.
Presumptively placing people who don’t use substances on substance abuse treatment plans. I’m still having trouble wrapping my head around this since 2012 when I first discovered boards/PHPs were doing this.
If anyone out there can help me understand this, I would appreciate your thoughts. Truly.
Thanks in advance,
The systems for ‘impaired physicians’ were developed mostly for those with substance abuse (alcohol/drug) problems. Anyone who doesn’t fit that profile is put into the same system because it’s what exists.
So the algorithm is an addiction recovery one regardless of what the physician actually needs? I would really love to hear from anyone who sought help (voluntarily or involuntarily) for a non-addiction mental health issue. Were you helped? I’ve only heard from physicians who have been injured by being mistreated on substance abuse recovery programs when they had no substance use issues—just anxiety, depression (usually occupationally induced or exacerbated).
What I’ve observed is that a system has been developed for physicians with drug or alcohol problems – and because a system hasn’t been developed for physicians with other mental health issues (PTSD, depression, burnout, other addictions/compulsions, etc.), they are forced into the same system if they want to keep their licenses. Square and triangular pegs forced into round holes, because round is the only type of hole that exists and ‘something has to be done’. The result is at best foolishness, at worst it magnifies the harm.
I spent three months in one of the few treatment programs specifically geared toward treating physicians, and the best description I know of it is a ‘treatment mill’. I could go on and on… The running (more than half-serious joke) was that they wouldn’t talk about a discharge date until the person’s money was running out – I knew some physicians who were kept there for more than 20 weeks, after being told (as we all were) before admission that it was a 6-week program. The physicians who were held up as being good examples seemed to me to be broken shells of human beings.
PHPs and Boards were going to rely on the treatment team’s reports, so if physicians wanted to have any chance of practicing again they were a captive population in the program. The system is rife with conflicts of interest and dishonesty. However, any concerns/complaints from the physicians in treatment are disregarded as being a reflection of whatever underlying label the team might choose (narcissistic, oppositional, denial, gaslighting, problem respecting women…).
I understand that you know of several doctors who died by suicide while you were there. Can you share more about that publicly here?
sara mamman, md mph.
emergency doc, resident turned drop out.
pure psych –> dx bipolar. alcohol was used as mitigating substance, self med.
i was terminated by my residency program 2/2 failure to thrive.
its a nonsense dx. i am fighting. from outside the system.
i want psych system REFORM.
Most of the state mental health questions are asking you if you have a condition that currently impairs your ability to practice medicine, not whether you have ever seen a psychiatrist or counselor. If you feel you are currently impaired to practice, then you should not be practicing. If you don’t feel you are currently impaired, then you answer “no”. I can give such question a pass as not being inappropriate.
Thanks for this, Tom.
Indeed, no application question should contain ANY time frame other than “current” or “currently” impairs. Should not be qualified with either “could” “could if untreated”, as so many do as a way of still attempting to extract impermissible information.
It seems to me that MLB/PHP cartels more often than attempting to use a “direct threat” argument, claim that physicians are in “safety sensitive” positions (as advocated to them by FSPHP and ASAM), along with certain other professions, and then they create this slippery slope scenario of illness preceding impairment, thus creating the self serving construct of “potentially impairing condition” and then argue that they are merely attempting to prevent impairment (and “protecting the public”) by jumping on any indication of past or present illness. Which they do with their pre-set interventions, largely based of course on the substance abuse model that is their raison d’etre . Still impermissible under the ADA to treat docs with a history of an illness that is not CURRENTLY impairing them, any differently from all others without any indication that they are unable, with or without reasonable accommodation to perform the essential functions of the job.
Absolutely true. Now I hear of cases of medical students pulled into PHPs after dean sends student asking for brief LOA for a rheumatoid arthritis flare (for example) to an in-house psychiatry consult where psych extracts all sorts of details about student’s past including remote use of ETOH in high school and then leaks all info back to dean. They send student to PHP for mandatory monitoring or removal from med school. One student revealed that 20 out of a class of 120 students were sent to PHPs for eval/Tx. Many PHPs are now giving orientation lectures at med schools encouraging students to call them if they have any stress or anxiety in med school. Huge COI.
One of my 4 areas of ABMS board certification is in occupational medicine and the cynical over-use of the designation “safety-sensitive” by employers who seek ever more intrusive and irrelevant medical qualification of workers is commonly-observed in crafting workplace drug and alcohol screening policies. These policies are often crafted for potential employer customers by large corporate vendors of drug screening services who have an interest in promoting the sales of their corporate drug policy products and services. Also, many state workers’ compensation programs promote the implementation of these dragnet policies by offering an indemnity payment discount and burden of proof shifting when workers reporting an injury are found to have body fluids or tissues that contain a potentially-impairing substance. So the employment landscape now contains many examples of workers deemed to be in safety-sensitive positions that strain credulity. However, my experience is that these employer mis-classification attempts mainly do not make it into courtrooms.
My impression is that the increased powers of ADA since the 2008 enactment of ADAAA is greatly under-estimated and nowhere more than in the healthcare fields. Flimsy arguments about protecting public safety and inadequate medical and psychiatric examination procedures and reports cannot be expected to fare as well after 2008 and pre-2008 legal precedents (extending as far as SCOTUS) will have less impact. Congress passed ADAAA to reinforce ADA after a quarter century of employer and court attempts to reduce its impacts. The early 1990’s saw the first attempts to use ADA in healthcare employment and licensing wither on the vine. The strengthened ADA is a more powerful tool and ALL the issues raised about ADA and healthcare more than two decades ago should not be considered settled law.
This is an excellent study. The write up was well organized, focused, clear. You and your intern (whom I hope you will express my compliments to) obviously put a great deal of time and effort into both the research and write up. Thanks to both of you for a job well done.
I shall let her know! She was amazing and getting all these applications organized on a spreadsheet that made the article MUCH easier to write. I had been wanting to write THIS article for years! Thank you Arianna!
What an excellent recap of medical licensing boards systematic and knowing violation of ADA in the pursuit of corralling all those it deems as disabled into its dangerous and rapacious PHP programs. Over the past 3 months, I and a colleague have been studying the ADA under the guidance of the lawyer who wrote the book on ADA for the ABA, Bill Goren. What we’ve learned is mind-boggling. As Louise pointed out, it’s not just the invasiveness and illegality of the discriminatory questions which are clearly in violation of the ADA, it’s what happens when you acknowledge illness.
While I’m in preparation of a longer post explaining ADA and its immediate applicability for physicians, I’d suggest that physicians in every state graded C, D or F contact the US DOJ Civil Rights Section to file an online complaint about the fact that these states are in apparent violation of the ADA. (see how to file a complaint under ADA.gov). Simply reference the offending questions as highlighted in this excellent study.
All would do well to research the 2014 US DOJ settlement with the La. Bar regarding its comparable ADA violations. The DOJ is serious about investigating these sorts of violations.
I’ll be following up with guidance on filing a complaint regarding discriminatory treatment if you have been compelled to be evaluated by a PHP and/or sent to one of their preferred facilities.
Great work Pamela and Arianna!
Excellent advice Kernan! Agencies and laws already exist to protect and defend us, yet very few doctors take advantage of the protections we have available to us. It’s so important to start framing these abuses as human rights violations so we can make real headway with a strategic plan. Financial penalties and legal repercussions much more effective than lavender spritzes and another “burnout” workshop. Sedating victims with meditation and mindfulness is not a solution. Pranayama breathing has it’s place. Just not the right treatment plan for institutional abuse of power.
I appreciate you having researched this topic, Pamela!
I’m applying for a couple of licenses in the C and D category at the moment. Maybe I’ll just stay put in the state where I’ve been practicing for 30 years~
May not be as bad as you think. Just depends how you answer the questions. . . Avoid TMI.
See, that’s a shame. I’m sure you have excellent skills that could be used in those C and D states. To have that hold you back is just not right…..
Exactly. I know of several doctors who didn’t even apply to C and D states because they did not want to “defend” their right to receive mental health care.
Pamela,
All in all our country is not doing very well in these regards. I’m assuming that many other countries in the world would have better scores in us. What’s been your experience with attitudes and practices elsewhere? As a health-care practitioner in California, I kept looking for my state and was appalled to see we received a D rating.
Given the dire state of mental health care in the USA and globally, the first place that we should be setting the standards for mental health care accessibility without stigma would be health care? Would it not?
I think the work you’re doing is truly game-changing for our profession. Laws will be enacted eventually to correct the injustices you’ve identified and shone a spotlight on. Public outcry will do the rest, but, as you identify, we must remain vigilant.
Labor of love. Have dedicated my life since 2005 to salvaging our profession and helping doctors who have lost their dreams find their way back to enjoying our beloved profession.
Thank you so much Dr. Wible. The ripple effects of your labor is astounding. You don’t have any idea how much you have helped and is still helping. You are a light. Keep shining to this dark area in medicine. God bless you immensely.
What a nightmare. I’m a med student with have well-controlled anxiety (on meds). I was planning to apply for residency in Florida and not sure if I should lie on the application. What do you think?
Use your best judgement. Many questions are illegal in their scope. Follow your conscience. The key is whether you are a danger to patients. Are you impaired?
My wife answered yes to the “ever been diagnosed with depression” question and was promptly referred to the PRN impaired physicians program. It has haunted her ever since. In her words, if she had it to do over again, she would NOT have answered yes to the question. This was in FL, 2006.
These questions are invasive, illegal, and counterproductive. Many competent doctors have been entrapped in these programs and sadly some have become suicidal and died as a result. We ALL deserve 100% confidential mental health care.
Great bit of research, Pamela. I really appreciate this investigation. It confirms what I already see–the lack of parity that is given to Mental Health. And that it is focused on doctors is so difficult. We already have so much ‘burnout’ and this revelation reveals so much more.
The root of many of out “burnout” woes is really chronic human rights violations as documented here in a recent keynote I delivered to Pennsylvanbia, Delaware, New Jersey PHPs and physicians from the tri-state area: Keynote: Physician Suicide—Prevention & Intervention
Nicely done Pamela. As a Psychiatrist I deal with these issues all too often. Apalling that a patient should be afraid to utilize their expensive personal insurance to pay for mental health provider fees, or unable to “fully divulge” the extent of their suffering to allow me to best help. Next you should look at getting a high security clearance from the Feds! DG
Tragic all around.
This is so very interesting, Dr. Wible! And disturbing!!!
great job Pamela.
Psychiatry has been weaponized against physicians in a variety of ways. Who here has experienced libelous entries placed into their EHR by psychiatry sucking up to the administration after a physician reported misconduct by a physician at that hospital, or by their personal physician? The EHR becomes a battleground for a false narrative against YOU, and a physician as patient is as vulnerable as is any patient, if not more because a physician’s concerns about quality and safety are presumed to be more credible. Then if you want to complain to the medical board or any other agency, the first they will do is want to read your personal EHR, which is now ruined, falsely stating psychiatric diagnoses or substance abuse issues that you don’t have! The reputational harm can be severe, and could cost you lots to defend yourself before a medical board, including hiring forensic psychiatrists to testify that you’re not nuts. Comments?
I have heard many, many accounts of this behavior, Been on the phone with physicians and med students who have had their careers destroyed by such unethical forces driven by greed. Here’s one from Human Rights Violations in Medicine (page 58):
Another resident shares, “Since starting medical school I have known one neurosurgery resident who died in a car crash due to fatigue, one of my former classmates died from an overdose of fentanyl, a resident at a hospital I rotated at died by suicide by leaping off the parking structure, and just a few weeks ago a resident at the hospital where my wife works died by suicide by gunshot wound. Reading your article was like cold water in my face, partic- ularly the following part: ‘If they violate work hours (by caring for patients), they can be forced to lie on their time cards or be written up as inefficient and sent to a psychiatrist for stimulant medications.’ I was a surgical resident who struggled with lack of sleep in a program which eventually was put on probation for duty-hour violations, though we were bullied into lying about our hours. Any violations were our fault, not the program’s. I was picked on by a more advanced resident, and the program director sent me to Employee Assistance Program because he thought I was the source of the problems. They sent me to a psychologist who diagnosed me with ADD. He sent me to a psychiatrist, who added bupropion and methylphenidate to my escitalopram. I ended up not having my contract renewed in the end.”
Just one example of using psychiatry as a weapon. Long history of this sad behavior within medicine.
I have just relocated to Louisiana and desperately need a provider LICENSE in Louisiana
What kind of license? Have you already applied with the board?
Perhaps one of the underlying misconceptions in the structure of medical licensing statues is the on-going and persistent belief that there is a separation between physical health and mental health, that it is more okay to be physically ill, than mentally. As if psyche and soma snap apart like Legos.
A cultural belief too. I hold medicine to higher standards and we should be demonstrating what real health care is (not discriminating against vulnerable groups who need it most in high-risk professions).
Dr. Wible, out of curiosity, have you mapped out the locations/licensures of the physicians you are aware of who have committed suicide and found a correlation between your A-F states? Is it less likely to happen in an A state? Most likely in an F state? NY is an A state, yet seems to have quite an issue with this. Is it just a higher concentration of physicians in the state?
THANK YOU for putting this information in one spot.
Ruth Braga MSN, RN
Physician advocate
What I do know is that there seem to be many more resident suicides in NYC area (NY is a Grade A state) though that likely has more to do with program toxicity and the concentration of residencies in NYC. Have not mapped out by state (though had a team working on that in past).
I have been reading this. I am so glad I did what my beloved mentor suggested and just put “no” on my medical license applications. I believe he saved me months of work and thousands of dollars of work on that one. It’s been a good choice and if I had it to do again I would do it again. Said the psychiatrist with treated and stable ADHD and depression (I don’t feel depressed and I feel great most days, and ADHD isn’t just about taking concerta, it’s also about leaving toxic environments and having the freedom to express my creativity.)
There is no such thing as a 12 step program for ADHD. Nor is inpatient treatment required. I once had an internal medicine program director tell me as a medical student that I needed a letter from my psychiatrist to state that I did not require hospitalization for “stabilization” of my ADHD. My psychiatrist just laughed and wrote a letter. Nope. No hospitalization needed for ADHD.
How stupid are these people anyway? And where did they get the unmitigated gall to propose a 12 step program or inpatient treatment for ADHD? Do they need their own licenses suspended for practicing goofy stupid psychiatry? Are they practicing outside their own scope? It sounds like maybe some board members need a complaint made to their own medical board for practicing psychiatry without a license?
Yes, a 12-step addiction recovery program for ADHD is probably not your best strategy and definitely not evidence-based medicine. Congrats for taking your own mental health seriously and seeking the care you need so that you can practice medicine safely without needless punishment by regulatory agencies that have overstepped the law in many cases.
Hello from Australia. We have had a national registration system since 2010 so we mostly don’t have the inter-state legislated differences cited in the excellent article.
As a psychiatrist I tell my doctor patients never to lie about anything on their forms because here it is an offence to knowingly make a false declaration and immediate de-registration is a possible outcome once uncovered.
We have many of the same sort of issues, but one uniform set of rules which are often applied very differently depending on which state you live in. I hope this helps.
Thanks Clive. Such a conundrum for great docs who seek mental health care and want to avoid being punished by regulating agencies here is US where there is a lack of uniformity in applications state by state and also subjectivity among various boards on how to handle the YES box.
Question: Can docs get truly confidential care in Australia without oversight by a regulating board or “approved” health program for physicians? If you have “approved” programs there are they based upon the 12-step program or evidence-based medicine?
I texted that article to our PHP (in NH), and she responded: “After years of work, the NH Board of Medicine should move from grade D to A on renewal questions if the state legislature approves the proposed wording changes. It is a very involved process that began 3 years ago. Hope to see the changes by January.” Just FYI!
Wow. Three years to align with the law in changing the wording of an illegal question on a form. Takes 3 years? In 2019? Really?
Update from Idaho Board on the status of mental health questions:
“It turns out that even though the Board approved the changes a while ago, we have been able to make the change only on this past renewal application (which just finished on July 1), but we have not been able to get it changed on the initial licensure application due to a technology issue relating to the Uniform Application at the Federation of State Medical Boards. I won’t bog you down with the details, but the short story is that those questions are embedded on a server that they are no longer updating, and until we are able to switch to their new electronic delivery system of all UAs (via API instead of XML), we will not be able to change those questions…. We will not be able to switch our database to the new API delivery system until our database upgrade is complete. That upgrade has been going on for 2.5 years and was supposed to be complete 1.5 years ago.”
How can it take several years to change the wording on a question? Most of these documents are online or downloadable PDF. Confusing how it can take years to update.
I texted that article to our PHP (in NH), and she responded: “After years of work, the NH Board of Medicine should move from grade D to A on renewal questions if the state legislature approves the proposed wording changes. It is a very involved process that began 3 years ago. Hope to see the changes by January.”
I appreciate these articles that Dr Wible publishes.
What was missed for this Nurse Practitioner, is that when she was practicing in Minnesota, Flexeril / cyclobenzaprine was prescribed for back pain, alone without narcotics, quantity of 90, refill of 1. I returned to Michigan and about 3 months later, refilled the script at Walmart.
Within a weeks time, I received a letter from the Board of Nursing that if this was a regularly occurring medicine, I needed to have a doctor sign off that it would not impair my ability to practice.
So Minnesota did not care, and the state of Michigan monitors all filled prescriptions for health care providers against a list they have deemed to impair practice. You gave Michigan a grade A. Just because there is nothing in writing regarding ability to practice, does not stop a state from invading privacy.
That is terrible! These Grades obviously have limitations are and only based on the initial licensing procedures for physicians. Obviously just one lens through which to view each state. I’d love to know what other states behave as Michigan tracking health care professional medications through pharmacies.
CAMMcB, you don’t say how recently this happened. To me it is somewhat surprising that a MI pharmacy would even honor a MN rx. That it was presented to them may have been some kind of a red flag that resulted in reporting to your board. What we do know is that MI PHRP contractor Ulliance has a record of presuming SUD in providers and acting pre-emptively along with healthcare licensing boards to suspend licenses in certain circumstances (such as a change of address causing a practitioner not to receive timely communications). Regarding a class action case launched by Ron Chapman who appears to have handled a lot of cases involving the PHRP. The class was not certified, but the claims quite disturbing if representative about the patterns of practice in your state. Obviously you should promptly respond to any communication from your board, but from your description here at least you do not have what a reasonable person would consider to be a “regularly occurring” medicine. If the board is invoking this criterion, they should have a regulatorily defined definition of a “regularly occurring” medicine. You should only legitimately be questioned if your use fits that definition. And even this inquiry (about your use of prescribed medication without any indication that it actually interferes with your ability to do your job or poses a direct threat to your patients) is questionable under the ADA, as it regards you as being disabled, and, using that criterion singles you out for questioning about your protected personal health information without any particularized analysis of your purported disability. Such discriminatory treatment entitles you to additional federal protections that an ADA knowledgeable attorney could assist you with. You should find one if you are currently under investigation.
Pamela, could you consider a parallel discussion regarding medical schools invading privacy also?
Absolutely. Have addressed medical school invasion of privacy in this new book: Human Rights Violations in Medicine. Contact me after you read it here and I’d love to counsel you on what to do in your situation.
Dr Wible,
Thank you for the information. It starts to explain a lot in my career (RN) as well as my (physician) fiance who died last year.
From what I understand, the only time he got into trouble with the state boards of both Texas and Ohio was from a coworker. This other doctor believes that anybody and everybody who is medicated for mental illness is an immediate danger to his patients. So when he overheard my fiance talking about being on antidepressants (chronic depression since 18 years old due to abuse in his childhood and a fact that he always spoke openly about during college, residency, and career, he reported him to the Ohio state board who reacted by putting him on probation for 5 years even though he never made a major mistake. Then the Texas board heard about it. He didn’t have the money or the time to run to Texas for the hearings, so he voluntarily gave up that certificate. That blackballed him with Medicaid and and several pharmacies (like CVS). It’s no wonder doctors are killing themselves with everyone trying to vilify everything they do. (got your lawyer ready for malpractice?)
I know that I will never go back to anything in the medical field even though I was very good at it. Everything I am learning validates my PTSD towards the medical field.
So sad that compassionate doctors and nurses are being victimized and unsupported for the obvious mental health challenges that come with the profession. I do feel optimistic that once people recognize the culture that sacrifices the lives of so many caring health professionals that things will change for the better. THANK YOU for sharing your story. I am so sorry you lost your fiance.
Please revisit the classification of WA. The questions you present are not current, they changed in Dec 2018 and shortened “current impairment” to past 6 months (from 2 years) and added a safe-haven provision for individuals known to WPHP. This means that individuals can seek help from WPHP and be exempt from answering the question on health related impairment on the licensure application.
Even prior to Dec 2018, WA was among the 30% or so of state licensure applications that were classified as ADA compliant in prior studies.
For all the criticisms of PHPs offered here and elsewhere, WPHP was instrumental in getting the licensing questions reviewed and improved and our work has been recognized as a model for getting this done across the medical regulatory community.
Collaboration and communication, relationships and hard work produce the needed solutions. Somehow we manage to move ahead despite misguided opinions of critics who have very incomplete information, throw rocks at us from the side-lines, haven’t ever walked in our shoes or even asked us directly what can be done to help.
The level of inaccuracy and misinformation in these posts is astounding and, frankly, apparent to organized medicine where there is deep understanding and appreciation for what PHPs do. These echo chambers are counter-productive and only reinforce the fear and avoidance they are intended to remedy. While there are certainly cases where physicians have not been able to benefit from PHP involvement, there is no question that PHPs have saved more lives and careers of physicians than any other institution in the health care sector. Discouraging physicians from seeking PHP assistance with unjustified claims of mistreatment plays on the susceptibilities of their illnesses and is irresponsible. There is motivation for visibility, self-promotion and validation lurking behind the guise of advocacy here. Meanwhile those of us doing the work will continue, out of the limelight, and will rarely ever post in forums like this. We don’t need to – you are doing a fine job of shooting yourselves in the foot without our help.
Thanks Chris, I’d love to see the updated initial licensing application. Has it gone live online? I will email you personally in just a bit to reach out for more clarity on Washington. And I thank you for making the progressive wording changes.
As someone who had heard from thousands of suicidal physicians, I certainly get to hear what is not working. I do not (obviously) hear all the success stories. (Those doctors who have successfully recovered from mental health issues and addiction are not the ones who contact me through suicide helpline.) In advance I thank you for the contributions you have made to helping physicians recover. I do know of one doctor who speaks very highly of her experience with the WPHP for mental health issues (non-substance abuse).
I also believe in collaboration and communication. Often the truth is somewhere in the middle. So very important to get all of us involved in physician health to create a physician safety net that works well in helping (never harming) our vulnerable physicians. To discount what great work some PHPs do (which I admit they work well for substance abuse in the article) or to discount that some physicians have been seriously injured by PHPs just creates polarization. I admire all individuals who have dedicated their lives to helping heal our healers. We can and must improve the services we provide to safeguard our physicians.
The PHP system might be on its way to helping doctors, however, it is far from perfect, and much work needs to be done, especially when a PHP is advertised as being non-punitive. The only non-punitive thing about a PHP is protection of your medical license. I think everyone will agree that paying on average $50,000 out of pocket to a treatment center plus an extra $5000 a year for the cost of monitoring and participation in a PHP is punitive, especially when you’re a resident or medical student. Don’t forget, this vulnerable population gets sent to these programs as well without the financial backing of an attending salary. Until the day doctors are not afraid to self-report, we are driving mental health disease and substance abuse underground which is going to hurt patients even more. If you look at your own records, you will clearly see that the majority of participants, even in your PHP, are not self reporters. I have personal experience with PHP’s, one being excellent, and one directly contributing the deterioration of my mental health and suicide attempt. I am one of the ones who called Pamela. Thank God she answered the phone. This particular PHP mandated that I see a cardiologist for my addiction care. Come to find out, he was a convicted felon with no addiction training. When I asked him for help, I was told that unless I have a six-shooter in my mouth, nothing would change.This particular PHP is run by an attorney with no medical education who pretends to be a doctor and dictates participants treatment even down to the level of what medication they can or cannot take. That sounds like practicing medicine without a license to me. When I called the PHP after my suicide attempt, and said that I have been depressed and need help and “I just want something to make me feel better” the response I got was “you sound like an addict”. Perhaps the quickfix mindset does sound like an addict, but why rub it in my face after such a traumatic event? It’s because she has no business talking to people as patients. No training. While I’m sure the Washington PHP is a good organization, I humbly ask you to comment only on that organization and not the PHP system as a whole. In my personal opinion, since the PHP‘s like to operate under the guise of the FSMB and FSPHP all treatment needs to be standardized and all PHP’s need to be standardized. Currently it is nowhere near that, and you know it.
If you have been helped (or harmed) by a PHP please feel free to leave a comment here. All are welcome and it is only through hearing the lived experiences of those who have received treatment from PHPs that they can be improved. Doctors have had a range of results within PHPs. Some have been helped. Others have been harmed. Some have died by suicide while under the care of PHPs. Some PHPs do not have physician oversight. Some do. Some seem to place everyone on 12-step addiction recovery as a preventive measure. Others don’t. Challenging to assess the quality of PHPs given that some are good and others not so much. Lack of standardized, evidence-based-medical treatment with physician oversight seems concerning.
That’s a fair request Yorktown. I’ll try and be more clear in the future. Likewise it would be helpful if folks would stop referring to PHPs as one monolithic entity and recognize that there are many different models and structures that vary by state. All can improve. I don’t speak here for FSPHP but only inform that there is a program under development called PEER (program evaluation and enhancement review) that aims to improve accountability, consistency and excellence among its members. Since each PHP is regulated at the state level, National Standards, per se, can’t be developed. National Guidelines are the correct solution, do exist and FSPHP’s have just undergone global revision in 2019. These will be the backbone of PEER and hopefully move everyone in the same, positive direction.
Excellent to hear. And thank you for your personal email. Wish much of what you shared could also be posted here for all to read and become more informed. I’d also love to speak with you in the coming weeks and will email you back a more comprehensive and thoughtful response to your letter. Appreciate all the clarifications and progress.
I’ve broken up my response to Dr. Chris Bundy’s 9/1/2019 comment to address selected elements. This is the first of likely several.
“…. Likewise it would be helpful if folks would stop referring to PHPs as one monolithic entity and recognize that there are many different models and structures that vary by state.”
I write, Dr. Bundy, not as a “folk,” but as a board-certified psychiatrist whose career was maliciously derailed by one state’s corrupt PHP. Curiously, after a scathing state audit, its executive director (a former president of your association) stepped down, leaving it to operate for a sustained period with utterly no medical director. And yet, it continued to run its malignant program with no medical oversight, utilizing SAMHSA-prohibited lab tests and conducting life-altering initial forensic psychiatric evaluations performed by a social worker and a licensed professional counselor, and with no corporate medical licensure (practicing medicine without a license or liability insurance). It did this with the full knowledge of that state’s medical board, its purported overseer, despite numerous physicians’ detailed objections.
Your reply is the standard evasion that FSPHP and its myriad collaborators routinely say – “if you’ve seen one PHP, you’ve seen … one PHP.” This is as if to say that they’re all so unique that there is no single guiding principle of assessment and referral by which they can be held accountable. This classic obfuscation is parroted relentlessly as if recited from a talking points script. If they’re all so unique, then why is there an entity called FSPHP which issues governmentally-quoted and judicially referenced guidelines? Oh, that’s right, because you claim they’re only “guidelines.” They’re just non-binding suggestions. Surely you’ve noted, the state and federal courts and other governmental entities don’t treat them as mere “suggestions.” In many states, veering from “professional guidelines” is considered to be unprofessional (disciplinable) behavior by licensure boards. But maybe not for PHPs.
Then also, FSPHP says it’s not responsible for its individual state PHP member’s behavior. There isn’t even a means to file a complaint to FSPHP about one of its member’s grossly unprofessional or illegal behavior. Nor is there any state overseer of most PHPs. They follow in the example of many state medical licensing boards which apparently operate in the complete absence of legally mandated oversight. Does this conundrum concern you? What we have here are “guidelines” that seem intended to give the appearance of a central overseeing authority and numb the target population – the physician community and other health providers– into having the false reassurance that their colleagues will be evaluated and treated by a state-sanctioned (and medical society-spawned) specialized physician health program operated by appropriately trained specialists with integrity. Indeed, maintaining the facade of medical integrity and treater benevolence while feigning due process seems to be this organization’s premiere achievement.
In further response to Dr. Chris Bundy’s 9/1/19 post, he writes:
“All can improve.”
This is not a matter of “improving,” Dr. Bundy. This is a matter of confronting profound abuse, organized unethicality and illegality. It’s a matter of taking ownership of a movement that has become corrupt through its lack of oversight and ever-shifting identity as a quasi state-sponsored immune entity conducting an intentionally nebulous “assessment” of individuals targeted as having “potential impairment.” It’s a matter of confronting a movement that has deviously shifted its mission from care of the legitimately diagnosed ill physician to “protecting the public” from intentionally undefined “potential impairment.” (It would be extremely helpful if you could clarify this concept as it serves as the legally acceptable pretext for apprehending a physician and subjecting them to the made-to-look-legitimate pseudo-medicalized para-disciplinary PHP RICO. And when you define this, perhaps you could share your process of coming to this understanding, i.e. do you seek critical input from those outside the RICO or is this one of several terms of art peculiar to this police-empowered enterprise that are defined only by those “in the know.”)
Indeed, this pervasive emphasis on “protecting the public” seems curiously coincident to the drive to tie burnout to patient safety and then equate burnout with depression, making it a “mental illness,” (one reportedly afflicting up to 50% of physicians) that can be leveraged to compel a physician into “assessment” and “treatment” at your “preferred treatment centers,” centers that demand cash up front (since these are not insurable medical illnesses) under threat of reporting the physician to the medical licensure board for noncompliance and licensure action. Potential for extortion? Are you concerned about that potential?
Additionally, Dr. Bundy writes:
“I don’t speak here for FSPHP but only inform that there is a program under development called PEER (program evaluation and enhancement review) that aims to improve accountability, consistency and excellence among its members.”
In fact as the president-elect of FSPHP, Dr. Bundy, you DO speak for FSPHP. It is this very slippery evasiveness that characterizes the devious deceptiveness of the corrupt PHP movement. Further, your reference to the self-corrective “PEER” program conceals the fact that, in reality, it is little more than an attempt to resist repeated calls for independent external oversight (for one prominent voice, see statements of Wes Boyd, MD [Boyd JW, Knight JR. Ethical and managerial considerations regarding state physician health programs. J Addict Med 2012; 6(4): 243–246]) by claiming a rigorous QA program of internal self-regulation.
So, you’re asserting that a movement that claims every PHP is unique and therefore can’t be held accountable by any central standard can be trusted to self-regulate. Really? And when are these evaluation processes and disciplinary standards for accountability going to be made public? Or is this something you’re also going to keep in-house? The timing of FSPHP’s newfound desire for self regulation is curious. Storm clouds gathering, Dr. Bundy?
Relying on the integrity of FSPHP’s entirely opaque “PEER” review program is as sensible as trusting the Catholic Churches’ promise to investigate its priest pedophilia epidemic. It’s fair to say they’re much more comfortable handling something else than self-examination. It’s now, only after close to a gazillion dollars in criminal prosecutorial settlements and concerted action by numerous states’ attorneys general combined with the exodus in droves of the formerly devoted faithful filling the collection plates that this secretive enclave is finally willing to take some modicum of internal accountability. Through the present, I see no evidence of any such ownership forthcoming from FSPHP.
As FSPHP’s incoming president, would you be wiling to share the specifics of FSPHP’s proposed PEER program? What about your plan to publicize its findings? Its corrective measures? Physicians’ capacity for redress? Or is the plan in reality to give lip service to accountability while exacting non dues income from participating PHPs?
Dr. Bundy writes “… National Guidelines are the correct solution, do exist and FSPHP’s have just undergone global revision in 2019. These will be the backbone of PEER and hopefully move everyone in the same, positive direction.”
Whether FSPHP’s 2019 Guidelines constitute a substantial revision from 2005 remains unclear. Their legal standing continues to be that of “suggestions.” What is also most notable is that there is no reference to compliance with the ADA. Compliance with other federal laws is given one mention on p.20 in an interestingly phrased Cautionary Statement: “PHPs may be required to comply with HIPAA and/or 42 CFR Part 2. If so, practices regarding handling and maintenance of records may be impacted.” MAY BE REQUIRED?
FSPHP is telling its member PHPs that each can make up its own mind whether to comply with 42 CFR Part 2 (governing all federally assisted alcohol and drug treatment programs) and HIPAA (strictly governing privacy and other patient rights protections)? This seems indicative of the magical thinking that emanates from this grandiosely delusional enterprise.
With this “out of sight, out of mind” intentional disregard, I would imagine it must be difficult for each state’s PHP to determine their need to comply with ADA given that it’s not even once referenced. I note that your co-chair of the 2019 Guidelines is Maureen Sullivan Dinnan, JD, and Debra Grossbaum, JD of MA PHS is an active member. One would think that attorneys, especially in this occupational healthcare regulatory arena, would be aware of the need for compliance with all applicable federal laws. Again, it would appear that FSPHP, like its individual state members, believes it is above such compliance. I trust that you’re aware that this indicates FSPHP’s deliberate indifference to applicable federal law and invokes serious consequences.
It is unfortunate that FSPHP did not apparently put these standards out for public scrutiny and criticism. Neither I nor my PHP-monitoring peers have seen such. As you probably know, there are numerous physicians – some directly harmed, others deeply concerned about PHPs’ tactics – who have reason to believe that some of FSPHP’s member programs are egregiously problematic if not corrupt. Then again, if one were running a state-sponsored RICO, I can readily understand why you might be disinclined to draw a lot of attention to your operation.
Surely, these are harsh judgmental words. And they’re backed up by an abundance of case histories of abuse by members of your federation.
Do you understand that one state program which happened to be the subject of an independent state audit in 2014 on the basis of multiple senior psychiatrists’ convergent concerns about a longstanding pattern of misdiagnosis was found to have potentially deprived 1,140 physicians of guaranteed due process protections? It denied them a copy of their official PHP diagnostic report (just as you may do in WPHP); it denied them the right to introduce independent diagnostic evaluation reports; it used its virtual board order authority (the threat of reporting to the licensure board for “non-compliance”) to sentence them to burdensome for-profit proprietary quasi-psychiatric evaluations at interest-conflicted private “preferred centers.”
These unusual “4 day inpatient evaluations” at out-of-state locations have no comparable equivalent in the entire US mental health system. At one or more of these “centers,” physicians have been subjected to interrogation by polygraph examiners, such specialists proudly advertised as being on staff. And then these same physicians were still denied access to any form of due process when these interest-conflicted centers “recommended” to the interest-conflicted referring state PHP that that newly diagnosed physician be sentenced to their own center or sent to yet another for-profit “preferred” “impaired professionals” specialty program – for three months! Cash only. Compliance required. And if they balked, they’d be reported as “non-compliant” and typically lose their license. And then from there, five years of “monitoring,” adhering uniformly to the purported gold standard PHP “blueprint,” itself based on a fundamentally flawed research paper.
Do you see a problem with any of this Dr. Bundy? Labeling those who bring legitimate criticism to your program as “misguided … critics who have very incomplete information [and] throw rocks at us from the side-line” is little more than distraction. As you and your ASAM and FSPHP colleagues continue to deny and obfuscate in this manner, you do so at the peril of the entire PHP enterprise.
Given what is now known about this scheme, I think it is fair to say that what your organization has participated in crafting has become not only a RICO operation but a systematic human rights violation. Intentionally designed as such or not (and that will be up to federal investigators to determine), it has become a massive scheme designed to entrap physicians in a financially bankrupting and psychologically devastating nightmare, one associated with a $12B drug testing and $34B drug treatment industry. Fair to say, you’ve definitely got a corner on the “impaired professionals” market. And from forays into lawyer assistance programs and the transportation industry, looks like you’re eager to apply this blueprint to perhaps all professionals who require licensure. That would spread the state-sponsored RICO licensee shakedown to every occupational licensing board in the country. Now that’s quite a market! You just got to make sure you use the same FSPHP lawyers to tell them to ignore federal law, okay?
It would appear that via FSPHP’s much vaunted though entirely opaque non-externally overseen PEER program, this abuse and violation of federal law will likely continue without any accountability, all the while giving the appearance of oversight.
Dr. Bundy. I believe it is you who is misinformed and sowing the seeds of self-promotion. As a fellow graduate of HSPH, perhaps you would be interested in debating me about these topics.
Pamela,
Back in the earliest days of my practice as a Licensed Clinical Psychologist
I learned at an annual APA convention that the standard for all
professionals living in rural counties is to “Go to the next county for your
mental health help.” As you well know, medical professionals of all types
are wary of creating any official record of mental health treatment. And,
as your current posting illustrates, they have reason to do so. During my
practice none of my files was ever sought by any medical licensing board.
However, as most of my years were spent in ongoing group practices, I do
worry at times that I might have left any notes not adequately circumspect
on medical staff so as to cost them a threat to their own practices.
Wow. I’ll have to ask around at the upcoming psych conference I’m keynoting this fall. I wonder what most psychiatrists recommend these days.
Dear Pamela, As a physician who struggles with suicidal thoughts, I appreciate what you do. Two years ago, I did a stint in a psych outpatient program due to depression, with great success. Since then I’ve moved to a new state and I find that I need support again. My medical director suggested I self-refer to the physician health program here. So I called (and didn’t give my name) and was shocked by how unhelpful they were. They described the process, which would delay returning to work. I’d be forced to comply with years of monitoring and pay for multiple evaluations and random drug screens. (Even though I don’t have a substance problem.) I may be mentally ill, but I’m not crazy! It seemed punitive and geared toward addicted docs with nothing to offer everybody else. I don’t think preventing suicide is on their radar at all. I would love to do more to advocate on this issue, but honestly I’m just trying to stay alive. ~ Adam
Those who self-refer to PHPs should be guaranteed that they will receive evidence-based medicine-the standard of care-with confidence and trust. Part of the concerning issue here is the variability between PHPs. Preventing doctor suicide has not traditionally been on the radar of medical boards or PHPs. Boards exist to protect the public FROM physicians and PHPs originated to rehab addicted physicians so they can return to practice safely (if possible). Neither organization was formed with an acknowledgement of the physician suicide crisis.
This info is very informative…. Keep up the great work…. Hopefully one day the abuse in the medical profession will stop!
Unless doctors start fighting back it will only stop when there are very few doctors left to abuse and they will have to start making being a physician a lot more attractive. It is already happening, I have never seen recruiters so desperate to find physicians. I even had a recruiter will to pay me if I could give them a lead for a physician that may be interested in whatever crappy doctor mill position they were trying to sell with colorful words, enticing pictures of family time that is all lies because the physician will never see the light of day not to mention their family once they start their abusive overwhelming underpaid family practice position.
I was definitely subjected to this discrimination, and it still comes up EVERY TIME I apply for a new job, license, or malpractice. All I had was run of the mill out patient managed depression, and I probably should have chosen to just lie about it like 95% of applicants must, but I didn’t, and almost twenty years later it’s still hanging over my head.
I used to be a program director and I was absolutely terrified that one of my residents would kill themselves. I had to send 25% of my residents to counseling for depression. In the last 16 days I’ve broken down crying 10 times. The biggest thing that delayed my going to my PCP and a psychologist was my fear of the PHP. I’ve personally seen what the PHP has done to a lot of good physicians, men and women who broke under the strain of medical practice and were blamed for it. I was so frightened that my PCP would report me to the PHP for being depressed that I lied about my mental health for years. I must say that I’m grateful that instead he and my psychologist are just straightforwardly treating my mental health problem for exactly what it is: a health problem. Right now I don’t need your help but it’s good to know that if I do have a crisis I have someone I could call. Thank you Dr. Wible.
Hey Pamela,
I was wondering, where does Washington, D.C. fit?
I actually don’t know. Can you send me a link to their medical board?
Sure. I can give you more details. I have a DC license right now and have met with the DC board once. I have a full, unrestricted medical license right now. Your article is so helpful. I applied for a Florida medical license, but will let it lapse and apply for it again. Just such a headache. I can tell you more about it. And the process is scary. I’m applying for another medical license right now and am not sure what to do.
Was there ever a consensus made regarding DC?
I think the whole licensing system is a business. I have not come across absolutely no scientific evidence that it improves patient care or saves lives. Absence of that what role does it have? Only the good Lord knows.
Thank you for this article. Reminded me of when I was choosing residency programs. I limited my options to states in your A and B categories just for the fear of being put under a magnifying glass for some treated anxiety with time off during med school. After all the hard work and a 1/3 of a million dollars in debt, I feared that I wouldn’t get a residency. Thankfully that wasn’t the case, but I still get a little anxious just thinking about the process.
I think questions can be asked in a way that protects the public and at the same time support a culture where physicians seeking well being are not automatically labeled as crazy and incompetent until proven otherwise. I believe the current system is counterproductive as many physicians never seek help due to fear, and ultimately burnt out physicians can lead to increased morbidly and mortality for patients.
Anyways thank you for all that you do,
Antonio
Very interesting and informative article. Just makes me furious at this one more abusive action against physicians. We as physicians need to start turning our anger outward instead of inward (suicide) and fight this oppressive system or switch professions!!!!!!!!We need to stop letting everyone bully us.
YES. “Action is the antidote to despair.” External action to remedy the human rights violations rather than self-homicide or voluntary death as the only way out.
Dr. Wible, Your articles are good compilation of information of well known facts . There is no action plan about reaching out to Medical Boards and inform them of this awareness of yours
Have a mass appeal signed by physicians suffering with mental health issues and send them to your B category Medical Boards. Take help of some mental health legal groups Have a dynamic manifesto with signatures of physicians discriminated due to mental health issues.Transmit this manifesto to APA & AMA.This will put you on the map with national recognition. My concern is that your “awareness campaign” will soon phase away unless you implement some action like NAMI does. People will come forward with large donation and endowments.Involve NAMI (Washington DC) under caregiver(M.D.s) survival appeal.. You don’t want this to be a passing phase of “ I told you so” soon to be forgotten, about what was told!
God Bless & Best of luck
My state is hardly a grade A state. Perhaps they do not ask questions, because they subpoena medical records instead. Although I had no history of substance abuse or mental illness, I was accused of same. I was also accused of “cognitive impairment” IN SPITE of the fact that all former supervisors had rated me as an outstanding clinician. My license was put under “emergency action.” I went through 8 months of sheer hell as they “investigated.” Although it was clear from the second month that there was absolutely nothing to investigate–especially after even the PHP cleared me–the Board refused to acknowledge their error; instead, the Board ruined me financially with legal bills, costs for evaluations for conditions I never had and my inability to work during their so-called investigation.
I live in perpetual fear of those minions of Satan. I am, in fact, so petrified of them, all doctors and all hospitals, that I will not even drive past a hospital (on the few occasions that I venture from home). I will never recover my reputation, nor will I recover my financial losses, given my age. And the worst of it is that I will NEVER EVER again have any semblance of peace of mind.
For the record, their error must be considered comparable to that of a surgeon who amputates the wrong leg–horrific, devastating, inexcusable, incomprehensible and indefensible.
Regarding “subpoena medical records” I have now learned that there are psych services available to physicians in which the medical records are not only handwritten without the complete name on the chart, these charts are stored in a SAFE inside the office that only opened by the fingerprint of the medical professional keeping the truly confidential records. Not sure a subpoena will work in these cases. What other ways have docs been guaranteed confidentiality?
Hello from Australia again.
A subpnoea is an order from a court to provide the documents and here it is an offence not to provide whatever is requested (ie the original unadulterated documents).
Treating health practitioners could also be sanctioned here for not keeping proper, legible and contemporaneous records that would be adequate for another practitioner taking over the care of that patient.
The US system seems broken to me.
It worries me also that the patients are unlikely to be protected by a system that has so many flaws.
Keep up the good work Pam.
Yes. Worrisome all around. Thankfully peer-support groups are popping up around USA and many physicians are spearheading out reach efforts to each other. Culture change is happening.
Although I live in a “Grade A” state (Maine), I still work in a high-risk field. I would never want someone call into question whether or not a decision or bad outcome was a byproduct of the problem list in my chart: “depression” or make a judgement based on the fact I take prozac. The word “depression” hardly encompasses the depths of me, or what I had to do to get better.
The use of physicians’ private medical records to discredit them and discriminate against them for disability insurance, licensing, hospital privileges, and medical liability cases is a violation of their human rights. Publicizing private medical records online is a form of extreme shaming and bullying. Of course, physicians who are incompetent must be removed from patient care. Why the public flogging of humanitarians? How does this benefit anyone?
Hi Pamela, I believe my initial Ohio licensure story and the ensuing consequences are an example of your medical board review. By checking the “yes” box for the application question: Have/are you treated for depression, I was required to sign a five year Consent Agreement, which includes a stringent quarterly regimen; each quarter, the following had to be submitted to the state medical board: evaluation letters from multiple colleagues to affirm my fitness for practice and appropriate interactions with staff and patients, scheduled meetings with an assigned Psychiatrist for validation of my fitness for practice, and a meeting with a board subcommittee, all completed prior to that month’s board meeting. This was done because I did not hide having been depressed and was (am) still taking an antidepressant. I’ve always wondered what would’ve happened if I’d just lied and said I’ve never been depressed.
“I’ve always wondered what would’ve happened if I’d just lied and said I’ve never been depressed.”
You would not have to do all of this:
“By checking the ‘yes’ box for the application question: Have/are you treated for depression, I was required to sign a five year Consent Agreement, which includes a stringent quarterly regimen; each quarter, the following had to be submitted to the state medical board: evaluation letters from multiple colleagues to affirm my fitness for practice and appropriate interactions with staff and patients, scheduled meetings with an assigned Psychiatrist for validation of my fitness for practice, and a meeting with a board subcommittee, all completed prior to that month’s board meeting. This was done because I did not hide having been depressed and was (am) still taking an antidepressant.”
I am not surprised at all to see my state at the bottom of the list. Since being hospitalized with severe suicidal depression, I have lost my privileges, malpractice insurance, a current case (malpractice) now wishes to settle instead of defend my care (patient died of blood transfusion reaction not negligence or poor care on my part), my specialty society is failing to let me sit for MOC, and these events are all reported to the board so I will face a board investigation soon.
It breaks my heart that as a society and community of physicians we do not extend the same care and concern that we extend our own patients. I tried so hard to handle my own mood disorder without the help I desperately needed because of the repercussions I new I would face. Going to the hospital was the very best thing I have ever done for myself. I am facing a total loss of my career and livelihood but I can now handle it and stay alive.
I am so thankful for the work you do. It made me smile when I was in the hospital and a physician gave me your name (as if I had never heard of you). They were giving me hope and giving me the care, colleague to colleague, that we all so need. I am praying that your work will continue to make the positive impact to help so many others like me.
Pamela, just listened to this months EM:RAP CME and they covered an abstract from JAMA psychiatry from this January. very disturbing. Tried to evaluate suicide prediction models in the military- essentially they compared various predictive models to actual suicide rates and situations in the military/veteran population. they concluded that none of the predictive models was helpful 🙁 very discouraging results from a very large study…not sure how rates compare within the medical population ~ Josh
I’m not a physician, but a registered nurse who can relate all too well. At the same time I was starting my career I was stalked and subsequently assaulted in my own apartment. For the next several months I suffered from crippling PTSD and was hospitalized on more than one occasion due to severe anxiety from this event coupled with sleep deprivation from shift work and wanting to succeed as a new nurse. To make a very long story short, in order to be discharged the hospital psychiatrist forced me to self report to my state board saying I was mentally unstable. If I didn’t he said he would hospitalize me indefinitely. I got out into a monitoring program for substance abuse which has never been an issue for me and I had to submit to random drug screens at my own expense. I had to tell my manager because she had to write monthly reports about my work performance. (Never an issue.) It was the most humiliating, terrifying time of my life. I’ve since received counseling for my assault trauma and my traumas surrounding the aftermath, but I travel 1.5 hours away and pay cash. …. that psychiatrist, it was later discovered, was running a pill mill out of his outpatient office. After he was caught and convicted he shot himself in the head. …. it’s been eight years since all of this happened to me, but it’s still painful to think about how I was treated when I was already suffering.
I had to self report to a program in my state called “NAP” which stands for “Nurse Assistance Program” and is a monitoring program specifically designed for nurses with substance abuse issues. Participation in this program allows you to keep your license without officially being flagged by the state board. But once your name is submitted to your state NAP, they are required to follow up. So even after I called back to explain the bind I was put in to self report, they said I had no other choice. It was supposed to last for three years but I found a very good employment lawyer who got them to lower the timeframe to nine months.
If I’ve learned anything over the years, it’s that having the opportunity to overcome my struggles has made me more compassionate, resilient, and present in my work. Patients deserve that much from their providers. There’s so much potential for positive change in this field for all parties involved.
On September 12, 2019 the Colorado Civil Rights Division (CCRD) issued a charge of discrimination against the Colorado Physician Health Program (CPHP) because it admitted at a May 16, 2019 public hearing convened by the State of Colorado that it employed “no standards” in deciding under what circumstances it would refer a recipient of program services to the Colorado Medical Board for “non-compliance”. Since the Colorado Physician Health Program has a service population comprised entirely of medically-qualified persons that are “regarded as” having a medical or psychiatric illness, condition, or impairment, the CPHP service population is protected under state and federal laws that prohibit discrimination on the basis of disability. A Colorado state monopoly private program that diagnoses, treats, or otherwise interacts with disabled persons and announces that it will treat these persons in an arbitrary, standards-free manner has incriminated itself. The claim that resulted in this charge of discrimination is supportable without any further discovery or witness testimony. In this case, a firm foundation for the charges can be made from the public record alone. A Colorado Civil Rights Division decision was necessary in making this charge of discrimination: CPHP had to be held to be a “public accommodation” under the plain language of C.R.S. 24-34-601 because the breadth of jurisdiction of the agencies enforcing Colorado anti-discrimination laws is different than those of federal anti-discrimination laws. This fact required that charges be filed at federal agencies in parallel with the state process.
Much more insight into the philosophy and operating norms of CPHP has become available because of the state contract procurement process in which CPHP is currently engaging. Despite a great deal of public comment against further weakening of the already weak confidentiality norms of CPHP, the State of Colorado has published a request for proposals (RFP) that seeks contractor performance that broadly violates medical confidentiality and disability anti-discrimination laws. Luckily, the Colorado General Assembly changed state procurement laws in 2017 so that “any aggrieved party” may protest specific procurement requests and awards. There are over six substantive bid protests about the current RFP SJAA 2020-52 that must be addressed during the period September 24-30, 2019. The substance of the responses will determine whether contracting agency review of the protests will continue at a higher executive level or whether the bid protests go to Denver District Court. A procurement award cannot be made with a pending bid protest.
It was revealed by the bid soliciting Colorado agency, DORA, in the public vendor questions and responses document added to the published RFP package on September 9, 2019, that a striking majority of CPHP service recipients are referred by third parties to CPHP. The numbers are reported in the Q&A document herein:
The distribution is very important when you consider that over half of Colorado physicians are explicit EMPLOYEES. Under Title I of ADA, the referral of employees for mandatory medical and psychiatric examinations is tightly regulated and requires that a referral source clear a high bar in making any such referral. Also, the content and standards of such an evaluation and any report of it are highly-regulated in federal statute.
The thrust of all these remarks is that CPHP now faces scrutiny from multiple sources: CCRD, parties aggrieved by the content of the new physician peer assistance contractor bid, the EEOC regarding a norm of apparent Title I ADA violations, the USDOJ regarding 3 or more separate Title II ADA complaints, and the FTC regarding the creation of a monopoly for physician peer health assistance services. Several committees of both chambers of the Colorado General Assembly heard testimony about the multiple problems with the CPHP status quo in April 2019 and the written testimony is presented here:
The state and federal agency complaints and the bid protests all go to the fundamental precepts of CPHP and its 33 years of operating norms. Interested persons should follow these developments closely because it is likely that the stage is set for resolution of some of these issues in Colorado. Changes to CPHP will likely reverberate nationally as CPHP is widely considered to be a flagship operation of FSPHP.
I practice in Alaska, the absolute worst state. I disclosed that I saw a therapist and was on antidepressants when my daughter died during intern year. I had to go before the medical board and explain what actions I had taken to correct my “impairment”. I received a very humiliating letter detailing how persons in Alaska develop SAD and asking for details as to how I was going to prevent that from happening to me, nevermind that I had already lived in Alaska for several years in the past and had never experienced SAD and wasn’t any more vulnerable than any other doctor applying. I had to present a written letter from a psychiatrist who had never seen me before and my PCP stating that I was fit to work as a physician. It’s absolutely ridiculous.
I would like to mention that this study on variation in state medical board licensing questions is in some ways analogous to the Dartmouth Atlas observational study on the variation in rates of medical procedures across the USA. The thrust of the Dartmouth Atlas study was that breadth of the variation in rates of procedures was not apparently related to the rates of disease incidence nor to the outcomes achieved by the procedures.
Dr. Wible et al. have described great variation in state medical license question items regarding past and current mental health diagnoses and treatments. All the state medical boards have recognized a general duty to protect the public from unsafe medical practice or something substantially similar but they approach this perceived problem with different measures. Some of these measures even look to be facially-apparent Title II ADA violations. Noting the variation in actions that states take which are presumably taken to protect public safety, are there are data linking the variations in preventive measures to variations in outcomes?
The apparent answer is “No”. This state variation in degrees of ADA violations is not related to any outcomes at all. The reason to mention this is that just like employer examinations are limited under Title I ADA to the scope necessary as defined by “job-related”, “business necessity”, and “direct threat”, state medical boards are required to follow the same standards under Title II ADA. Dr. Wible’s licensing question variation study is good evidence that apparent violations of ADA Title II by state medical boards are not defensible on grounds of “business necessity”.
I hasten to add that grading state medical boards by degrees of inappropriateness, irrelevance, and illegality of medical licensing questions produces only a single index of board behaviors. There are 47 or 48 state PHP’s across the nation that are FSPHP members. The 2019 FSPHP PEER Guidelines describe “best practices” for PHP’s and a fundamental philosophy that are completely incompatible with a host of state and federal laws that have a bearing on disability ant-discrimination and privacy. It would be incorrect to say that state medical boards that are rated favorably in the Wible study by dint of the absence of objectionable medical licensing questions have resolved all their problems with wide-ranging violations of anti-discrimination statutes that apply to physicians just like everyone else.
The consequences for physicians identified as having mental health conditions may get worse as Medicare threatens to exclude these doctors from its fee schedule. The following article outlines this plan to discriminate:
Rule Buried in Proposed Medicare Fee Schedule Could Have ‘Chilling Effect’
Kerry Dooley Young
October 01, 2019
ANYBODY who’s brought before the board or PHP on an alleged impairment issue MUST HAVE ADA informed counsel to protect their interests. Too many (all?!) enter without such expertise and they miss all these protections.
Also happening in the UK with abusive (or punitive) assistance programs.
There is another fear among doctors that if they disclose they are having depressive symptoms then GMC will say your fitness to practice is impaired (which is not done in case of physical illness). Therefore, stigma and discrimination is still prevalent in regulatroy body, and it is preventing doctors to seek timely treatment, help and support. So, if you disclose your career will be ruined and if you don’t then doctors might end up taking their life. If we want to improve the situation, First of all we will have to remove the stigma and discrimination from top.
Also agree with RJ above. I self-reported to GMC when I was first admitted to a psychiatric unit and some of their assessments felt nothing short of abusive.
Hi Dr. Wible:
A comment: I noticed in one of your lectures on physician suicides in October of ’18, you mentioned that the Oregon Medical Board refused your request to collect data on physician suicides. I’m not surprised. They do not want to be linked to suicides of licensees, as this might result in greater scrutiny of their management of physicians who struggle with addiction.The OMB, as you probably know, works in a vacuum with absolutely no oversight. They act as judge, jury and executioner.
I don’t know if you know the history of HPP (Health Professionals Program) or HPSP, (Health Professionals Services Program) it’s replacement. The former was instituted in the late 80’s in response to the alarming number of physician suicides, in part due to how their chemical dependency issues were managed by the Medical Board. The HPSP, (Health Professionals’ Services Program) the later, was formed following the disincorporation of HPP due to funding issues. As a physician who is being monitored by the HPSP, at the behest of the OMB, I can tell you that the level of misery among docs in the program is worse than I’ve ever seen due to the way the board handles “enrollees” .
Prior to my self-admitting to a rehab facility in Minnesota, the Board suspended my license. Upon successful completion of the program, although I did everything they asked of me, including a long history of clean toxicology panels, I’ve received no date for reinstatement of my license. Meanwhile, my clinic has gone down the drain after 20 years of successful practice, I’ve lost everything I worked for these past 2 decades. I’m not sure if the Board doesn’t fully grasp the hardship they are causing, or perhaps they just don’t care. Many of my colleagues I was with in treatment who are still in HPSP are in the same situation. In our weekly Caduceus group, it’s 60 minutes of rage about the boards treatment of licensees in the monitoring program. I don’t have raw data, but the group chair noted that the numbers of physician suicides are again on the rise. Not quite to the level of the pre-HPP days, but headed in that direction. I didn’t post my name because I’m concerned about reprisals from the board. Google: Dover vs the Oregon Medical Board. Thanks for taking the time to read this. I wanted to shed a little light on the OMB’s management of the participants in HPSP’s program, and why they might be resistant to providing you with data on physician suicides.
The Pharmacist’s impairment programs are completely punitive. I self-referred and was subjected to many years of mandatory Health Care Support Groups, which consisted of all men, except me. The facilitator was an EAP with no professional license. I went back to substance abuse and was eventually caught. I voluntarily went into the PIP, for 4 years @ $1000/month. It took the BOP 4 years to charge me, Then I was mandatorily forced into the PIP(pharmacist impairment program), placed on probation and was charged again paying $1000.00/month for the fees charged by the mandatory urines/HCPG/pharmacy board charge for being monitored by the Board. I was given no credit for the 4 years prior(I did everything they asked at a cost of over $35,000 including treatment at their demand and I spent a year in a recovery home) and had to start as a new participant. I was given 3 years of probation. In the third year I was kicked out of the PIP, because they claim I missed paying a lab fee and hadn’t responded to letters regarding that. The truth was, I had moved, and the lab hadn’t changed my address. Also, the case manager (an RN with no specialty in Addiction) relapsed, and the notes he had taken about my continuous sobriety disappeared.) The dental board case manager was assigned all of the pharmacists and my only phone call with him was a disaster. The next week I received a letter I had been kicked out with no reason. I called the dental board case manager over and over and never received a return call. I then called the BOP to demand a reason for my dismissal, and they told me to call the PIP. I finally got ahold of someone at the Diversion program and was told I needed to call the BOP to find out. This happened 3 months before I was to graduate from Probation. No one could give me an answer. I cried and became suicidal, because I didn’t know what to do. I had a last payment of $1400 for my probation costs. I didn’t know if I should pay it or not, and for 6 weeks I called the BOP as did my boss, and neither of us received a call back. The date came, I hadn’t paid the fee, and the next day I received a registered letter from the BOP revoking my license for non-payment of a fee and breaking the terms of my probation. I called the BOP immediately to explain the situation. I was told everyone from the BOP was gone that day because it was Easter weekend. I was suicidal all weekend, distressed and in the fetal position. I paid the money on the following Monday. I was told I could re-apply in 3 years. Life got worse. Obviously, I didn’t kill myself, as I am writing this comment. I will always have my life laundry displayed for public view on the Pharmacy web page for the rest of my life. After 22 years of sobriety, I have been able to be employed, but I have been disgraced when admitting to my wrong doing’s during interviews, like one of the retail giants, who told me “we don’t hire people like you.” This past June, (21.6 years sober) a disgruntled employee who was asked to resign, reported me to the BOP and said I was “impaired” while working. The Board inspector heard my story, after all the employee’s stated I was honest, a great pharmacist and never impaired. She told me she believed me but “you will always be vulnerable, while you practice, because there is nothing you can do to get the black mark off your license forever”.
There it is, I will always wear a Scarlett letter A because of something I did 22 years ago.
I would like other pharmacists to join with me.
Pharmacists are treated worse than any other Health Care Professional because of “our access” to dangerous drugs. There is so much to the rest of my story, but I have spent way to many words.
Thank you for listening
Ah yes! Please organize pharmacists who have been thrown under the bus. Seeking help for our mental health should not lead to punishment. So very sorry you were mistreated.
I had a miserable time (to put it mildly) when dealing with both NY and NJ PHPs. It shocked me to see that NY and NJ are considered the most physician friendly states.
“Physician-friendly” is rather limited in its scope and only (for the purposes of this article) applies to initial licensing applications. Does not mean that once you have a med board issue, toxic employer, or PHP experience in these states that you will be treated in a fair of friendly way. Sad but true. Physicians are so often punished and not helped for the very real wounds that they experience in medical training and practice. Thank you for being so courageous to share some of your experiences here (and with me privately). I’m appalled at the ways vulnerable physicians are treated in times of THEIR greatest need (after giving so much of their lives to help & heal other). Tragic. However (on the bright side), there IS help and more and more docs are waking up to the needs of their peers. Culture change is coming—-albeit slower than I would like.
Kudos to Nevada for being a GRADE A state and featuring so many articles on physician suicide and wellness in their newsletters:
Main article recent newsletter entitled: How Do Trauma and Death Impact Physician Well-Being? with quotes from Human Rights Violations in Medicine book.
Impressive!
I think that examining the history of legal challenges to state medical board licensure questions will explain some of the variation in the results that are seen. NJ has very simple questions now. But it took, Medical Society of New Jersey v. Jacobs (1993) to bring about these changes. The USDOJ amicus brief in this case is as applicable today as it was in 1993.
The message is clear. In order to eliminate these questions, the USDOJ has to be forced to complete the work it started in 1993. That means that the questions need to be eliminated in EVERY state by filing a complaint with the USDOJ and following up. If no action is taken, then it will take a federal lawsuit in District Court. But the brief was essentially written for you in 1993 and is available at the link above.
This should be viewed as a settled issue.
I timed this for accuracy. It took 12 minutes on the USDOJ ADA complaint website to write an ADA complaint regarding unnecessary, intrusive, and illegal questioning involved in Colorado Medical Licensure. I pointed out that Colorado lacks an ADA Coordinator as required by ADA Title II to address these concerns at the agency level and that there was no alternative but to file with USDOJ. The 1993 Medical Society of New Jersey case and the 2014 USDOJ settlement with the Louisiana Supreme Court were cited as precedents.
Anyone who is not in a Grade A state should do the same.
Remember that medical license questions contain tricks and traps designed to trip up or threaten licensed physicians. The closest thing you will encounter to documents like these are software EUA’s or credit card contracts. Everyone should approach them guardedly and with legal advice. No person is responsible to know or report everything good or bad that may ever been said about them. No crime is committed if one says something like, “I do not recall any such episode but if the licensing authority wishes to present evidence or documents to refresh my memory I will be happy to review and comment upon them.”
The Washington state medical license questions violate ADA Title II and Title V. By asking whether a physician has a condition (all of which are chronic) rather than asking if a person has a current impairment, they are breaking the law. A licensing agency that asks an applicant to request a reasonable accommodation or practice limitation is breaking the law. Reasonable accommodation requests can ONLY be legally-generated by an employee or licensee. A licensing agency that has no list of bona fide occupational medical qualifications for physician licensure (they cannot as none exist) may not require an applicant to get a medical evaluation at their own expense, receive treatment, or release complete medical records to a licensing agency. No agency is entitled to these records and requiring that an applicant relinquish federal civil rights as a condition of medical licensure is coercion and violates ADA Title V. The same standards apply to board assessments of “direct threats”.
Medical boards recognize that ADA Title II requires that licensing agencies must either pay for assessments of current impairment and receive only the determination and any other information that might have a bearing on reasonable accommodation. They assume license applicants do not know this and they hope physicians believe that granting a license may be conditioned on an applicant relinquishing civil rights.
These practices are propaganda and a con. None of them need to be challenged at boards, administrative “courts”, or in state courts. These are federal rights that are being violated and prospective injunctive relief against a state agency in available in federal court when their expressed policies and procedures violate federal law.
The medical boards display consciousness of guilt in convincing physicians to sign away their rights in applying for a license. That’s because these boards KNOW ADA, the Rehabilitation Act, 42 CFR Part 2, HIPAA all constrain their actions. They are counting on physicians NOT KNOWING that they have protections.
All it would take to stop this is a few docs applying for or renewing a medical license in some jurisdiction, under conditions in which they have little or nothing to lose, objecting to the requirements, experience delay or denial of licensure, and then file an Ex parte Young action for injunctive relief in federal district court. No depositions or discovery are required. The evidence for your claim is public documentation.
If you want to spice up your brief, use the USDOJ language appearing in their amicus brief filed in New Jersey Medical Society v. Rosen in 1993 and quote from public agency guidance on ADA Title II and ADA Title V.
No person or organization will voluntarily relinquish power. The boards are in the wrong in these matters and they know it. The boards hope that you won’t find out and try to scare applicants into giving up civil rights. Don’t let them. Level the playing field.
The California Board is biased and judgmental. In 2019, I was required me to supply them with all the venues regarding my manic depression treatment since 1980s. Of course, they wanted all the venue medical records before the beginning of the new year, 2020. Then, I received a Email from one of the California board investigators Informing me that I was not eligible to receive a license to practice in California because I have not met their new eligibility requirements. They required that I complete a three-year residency in family medicine as well as 24 months medical qualifying program before I would be able to apply for a medical license. The newly adopted eligibility requirements were enacted on January 1, 2020. Also, the California Board of Medicine did not accept my diplomatic status in the ABFP. I qualified under the grandfather clause in 1978. The ABFP did not exist when I graduated from my internship in 1970. Of course the board, wanted documentation letters of all my psychiatric care regarding mental illness of manic depression from all the venues including private psychiatrists, family physicians, and hospitals. Most of the venues eliminated the records after 10 years. Two of my psychiatrists have since died or retired. I knew this task was impossible for me to complete by December 31, 2019. MY initial application that I filed in 2018 was under review and because of my past history of mental illness. My application process is now a moot point. Incidentally Pamala, I’ve been under psychiatric care and have been compliant with my medications and stable for the last 20 years. Pamela, I just wanted to inform you of the new rules and regulations in California. I am not aware of any other medical board that has the same requirements of three year board certification in any medical speciality except California. I bet your State of Oregon does not have these new eligibility requirements. I thought the whole application process was totally unfair and discriminatory.
Your were too soft on the boards. We’ve communicated before on this issue & I really appreciate your review of their treatment of doctors and this definitely begins the discourse about how psychiatric diagnoses are weaponized against doctors. The boards should absolutely should be required to abide by HIPAA, allow independent review & have independent ALJ review & oversight. I would like to see a compliance panel that reviews all psychiatric & lab monitoring of doctors that has oversight of their activies. We should do a PhP review with grades! I’d be glad to help you review the PhP behavior of the boards and put that together for a grading system. I think a subterranean scale may be required for that one 🙂
I am in my third year of medical school, and I’m also in recovery from substance abuse. I intend to seek a career in Addiction Medicine or something in that path. I would like to target my search for residency programs in states where there the application for a medical license is less strict. I really appreciate this article – very detailed and thorough. I only wish that you hadn’t removed the data regarding substance abuse questions, etc. I will most likely use your grading of states for seeking programs, assuming their view on mental health is generally the same.
Any thoughts or other resources you could recommend? I’m quite anxious about this process coming up this Fall during interviews for programs, as I think I’ll have to be very clear and honest about my addiction issues and offer consideration to it being a strength rather than a weakness. It’s a lofty goal, but I believe being honest and straightforward in that situation would allow me to go into the program being known and comfortable.
I think you should narrow down your options (best programs & states) and NOT overshare your history or you may be wrapped up in a PHP for years. I’m happy to speak with you. Reach out here: https://www.idealmedicalcare.org/contact/
I will be participating in the PHP program, with ongoing engagement there for the next 5 years. If I remain adherent to the program, details of my case are not reported to the state medical board, just “participating in the PHP”.
If I were to leave for one of the “Grade A” states, would the medical board there interface with the PHP in my current state necessarily?
Many thanks,
James
Yes and there are ways to shorten your sentence in those situations. Happy to consult with you on specifics via a strategy session.
WOW, HUGE INFORMATION AND LINKS. THANKS A LOT FOR SHARING THIS ARTICLE.
Massive amount of dedication to create this piece though was a fascinating journey for sure. Glad I could be of help.
Fyi. South Dakota’s disclosures are officially changed as of may 5.
Applicants for licensure or renewal of licensure must “state whether the applicant is currently suffering from any condition for which the applicant is not being appropriately treated that impairs the applicant’s ability to practice medicine in a competent, ethical, and professional manner.”
I would also mention that most of these applications also ask for explanations for gaps in medical education or training or employment. Essentially they are fishing for more information. Responses like “leave of absence to get treatment for a chronic medical condition” or something similar will be met with requests for medical records or other information. So even if you get past these first questions, the applications are designed so that you’ll have to disclose in one way or another.
Why is PA considered “grade A?” It asks if the physician had ever engaged in “intemperate” substance use” which is insane. You must check yes and have your license denied and your life ruined for having been in recovery from a substance use disorder. Even if you’ve never drank in 20+ years? This question is an utter disgrace and this fallen-from-grace profession needs to get with the times. Many current med students are in recovery currently accruing massive loans. Are these criminally disgraceful and illegal questions going to be what greets them at the end of the tunnel? I suggest you look into the tragic case of Leigh Sundem. Pennsylvania has no business in the “A” category.
PA was graded (as all states) just based on mental health questions (not substance use). I agree with your comment though this was not the focus of the article.
Thank you. Has a criminal or at least civil wrongful death case been brought to these boards if a suicide resulted from their discrimination or misconduct?
Not that I know of.
Hello! I am a prenursing student that is currently taking a technical writing class and I would like to write about this issue and the lasting impact this has on medical staff. Would anyone be interested in helping me with this? I really appreciate Dr. Wible for bringing this to light, it certainly changed the path I chose for a medical career.
I am an M.D. and former primary care physician who was never suicidal but became burned out and then depressed after being fired by my hospital organization after one complaint, from one sociopathic female patient, after 33 years of medical practice. (Previous to this I had been considered a “top doctor” and had a full panel of satisfied but mostly elderly and complicated patients.) I can completely understand why physicians commit suicide though – our profession promotes empathy for patients, but none for any doctor against whom an embarrassing complaint is lodged by any patient, no matter how dishonest or sociopathic. In fact, the profession treats such doctors like a disgusting embarrassment whose careers should either be flushed down the toilet or sent to a group of greedy psychologists such as the Professional Renewal Center in Kansas, where you must confess to everything you are accused of, wallow in shame, and agree to humiliating, expensive and never-ending supervision in order to salvage a miserable and tenuous career. Any doctor who is brave or foolhardy enough to see a psychiatrist is at high risk of being forced to be evaluated by groups of cynical, greedy psychologists who have no empathy and seem only interested in extracting as much money from desperate doctors as they possibly can. There these doctors are taught how to focus on minimizing risk to themselves by distrusting all patients and referring all difficult patients to specialists. If these patients don’t want or can’t afford to go to a specialist, these doctors are taught to say “I can’t help you” (even if the doctor knows he probably could). I was an idealistic physician for 33 years, who tried to do my best for every patient, but I have become cynical about my former profession. It can certainly be very lucrative, if you concentrate on making a lot of money and avoid taking any risks to really help patients who may have any psychiatric disorder. When doctors focus too much on protecting themselves, patients can sense that, and will eventually become as cynical about doctors as doctors are becoming cynical themselves about the depressing medicolegal system they are trapped in, in which they are always at great risk of being sued or having their career end due to either one unintentional mistake (among the thousands of decisions doctors make every week), an unfortunate but likely unavoidable patient outcome, or a malicious complaint by an angry and/or sociopathic patient which may be partially or totally unfounded or misleading. I understand the profession wants to maintain its reputation by sacrificing doctors who cannot prove their complete innocence. But pretending doctors are infallible and forcing human doctors to hide any possible weakness or stress-induced psychiatric problem will cause doctors to become as sick or sicker than their patients! And eventually, it will cause some to become so depressed, or feel so guilty because they are not perfect or one of their patients has a bad outcome, that they kill themselves. I appreciate your shining a light on this problem, because I suspect the leaders of the medical profession would rather ignore it or cover it up.
Pamela I wonder whether you have commented before on how another concern for students accessing student health services is they **do not enjoy the strong privacy protections of The Health Insurance Portability and Accountability Act (HIPPA)**. Reading legal commentaries it is clear that HIPAA’s privacy rule does not apply to health records maintained by an educational institution if those health records meet the definition of “education records” or “treatment records” under the Family Educational Rights and Privacy Act (FERPA). Because student health records typically fall within these FERPA definitions, they are exempted from the reach of HIPAA’s privacy rule. See Department of Health and Human Services and Department of Education, Joint Guidance on The Application of FERPA and HIPAA to Student Health Records (November 2008).
Federal courts have consistently held that HIPAA does not create private right of action that would permit a person to sue in the event his or her records are improperly released. See, e.g., Adams v. Eureka Fire Protection Dist., 352 F. App’x 137, 139 (8th Cir. 2009). Courts have consistently held that there is no private right of action for a violation of FERPA. Thus, a suit by a student who claims his or her medical records were released in violation of FERPA is almost certain to fail
The latest WPHP contract has dropped the requirement for WPHP to track suicides and make a quarterly report to the Department of Health. It also explicitly endorses the use of abstinence-only diagnosis and treatment for SUD’s and any other condition in which it wishes to apply this pseudo-science approach.
WPHP has never made a quarterly report on suicides even when this was a contractual requirement. The DOH was asked to report the number of such cases and responded formally that they have no records on the subject.
Do you have a current WPHP suicide tally? The people who had responsibility for collecting these data completely shirked this responsibility.
The USDOJ has just ordered the Pennsylvania state courts to stop using abstinence-only approaches exclusively in its alternatives to discipline cases. Abstinence-only is not in line with current best evidence and is promoted by a cadre at ASAM.
I tried to get the Oregon Med Board to track physician suicides and twice they declined. Obvious place to track the active licensees who lapse due to death. No interest. I do have a list of doctor suicide cases that were involved with PHPs at the time of their deaths. Medical Boards exist to protect the public FROM doctors, not to protect or advocate for doctors. Sad reality. I am reading a book on the history of medical licensing and disciplining in America (note the emphasis on discipline/punishment).
Also want to bookmark this speech given by a suicidal surgeon in PHP – https://www.youtube.com/watch?v=JaNBH4UPHv4
I just renewed my Idaho medical license. They have changed the question about mental illness and substance use disorders in a positive way. Instead of the “have you ever…” question, it’s now something like “do you currently have a mental health or substance use disorder that is not being treated that could impair your abilities…” What a positive change!!! Thought I’d share.
See LornaBreene ALLIN campaign regarding ADA impermissible questions that persist even now on licensure, credentialing and indemnity applications. AMWA also maintains a map of states’ licensure questions compliance (not sure how recently updated, but there exists strong advocacy at AMWA for this cause and suicide prevention, since women physicians are at dramatically increased risk).
There has been progress since Pamela’s article, but it is frustratingly slow. And demonstrable backsliding suggests that due to liability concerns, permanent STAFF from these organizations may be impeding such changes, while (rotating) medical board members remain ignorant about institutional history and why they came about.
Also, the above cited language (which was directly taken from FSMB and has been parroted by AMA) is STILL ADA noncompliant, according to rulings by the DOJ. The “could impair your abilities”, especially when coupled with “if untreated” impermissibly asks the applicant to predict the future of their illness, something which authorities such as APA confirm is not possible with any degree of certainty.
Physicians and other healthcare professionals face many stresses in their careers. From long work hours, high expectations, and a heavy administrative burden, to an immersion in human suffering, the need to adapt to a rapidly changing healthcare environment, and a fear of making mistakes, it is not surprising that symptoms of depression, anxiety, and other mental health conditions are common among physicians. Even before COVID-19, there was an unprecedented level of burnout in the profession with many physicians reporting high rates of dissatisfaction with quality of life and work-life balance.
Despite these alarming trends, the medical profession as a whole has a long way to go in prioritizing physician well-being and overcoming the societal stigma around mental illness. As research is progressively demonstrating the dire consequences of ignoring physician mental health and the positive impact of a variety of interventions on physician well-being and subsequent patient care, physicians should no longer have to suffer in silence.
Many physicians who are dealing with mental health issues have questions about available resources, as well as whether they will be able to receive disability benefits for their mental health condition, and what, if any, impact seeking treatment will have on their medical license.
YES Yuli – absolutely correct. Longstanding problems WITHIN medicine that are perpetrating the mental health stigma against physicians that ultimately does not allow us to help patients facing mental health crises. I do not refer to our distress as “burnout” as what we have actually been subjected to are human rights violations. Doctors have not been allowed to be human (to sleep, eat, care for ourselves, get mental health care without fear or punishment). We have not been protected by labor laws that protect all other workers or laws that protect citizens of the USA such as ADA, due process . . . A real travesty for us ALL. Patients included.
This is all heartbreaking. I realize how much I have been spared a great deal of trauma. I live in a Class D state and by God’s grace and mercy I’ve answered “yes” and have not been penalized. Do not the same entities realize that we are impaired by sleep deprivation during training that can cause anyone to be psychotic and mentally ill? I don’t understand the logic in any of the criminalization in obtaining mental health care as a provider of care. If obtaining mental health treatment is forsaken, why are we treating the public for mental health? Do magic letters after our names make us superhuman? Make it make sense.
I am currently doing a monitoring agreement for a substance use disorder I don’t have. I hope to get a license in one of the F states after I finish the nightmare of the monitoring agreement in the current state in which I am licensed. Will the F state make me enter a monitoring agreement in that location in the future to obtain a license thereor will the monitoring agreement from my current location show that I am “rehabilitated?” I deeply regret seeking help for my mental health issues and also regret becoming a physician. If money weren’t an issue, I would gladly surrender my medical license.
Dr. Wible,
Can you please list the legal questions by state ? I can’t find them anywhere online.
Thank you for all that you do.
They are in the article listed state by state. What state are you looking for?
If you are hating your PHP, you should join our weekly support group for docs who need to be extricated from PHP abuse. Check out groups here: https://www.idealmedicalcare.org/physician-support-groups-every-sunday/
It looks like there’s been significant progress on this front! Thanks for your advocacy Dr. Wible! California now asks about current impairment, and I see from the comments that SD and ID have also followed suit. This is fantastic news for all of us.
YES time are changing and more openness about the occupational mental health hazards of the profession. Though still important to be vigilant to get CONFIDENTIAL care on your own (and not through employer or school when possible). Please see these 13 tips for getting confidential care as a doctor.
Depressed Doctor: How To Get Confidential Mental Health Help for Physicians