Dr. Wible’s keynote delivered at the 19th Annual Chicago Orthopaedic Symposium (begins with a beautiful legacy to the life of Dr. Dean Lorich by Dr. Matthew Jimenez). Downloadable MP3 above.
Thank you. I’m truly honored to be here and extremely grateful that you have given me more than 10 minutes to discuss doctor suicide. Looking at your agenda (three days of q-10-minute lectures back-to-back) as a family doc, I’m just a little blown away that you can cover complex acetabular fractures and mangled lower extremity grade IIIC salvage versus amputation in 10 minutes when I can barely treat a patient with a UTI or step throat in 10 minutes.
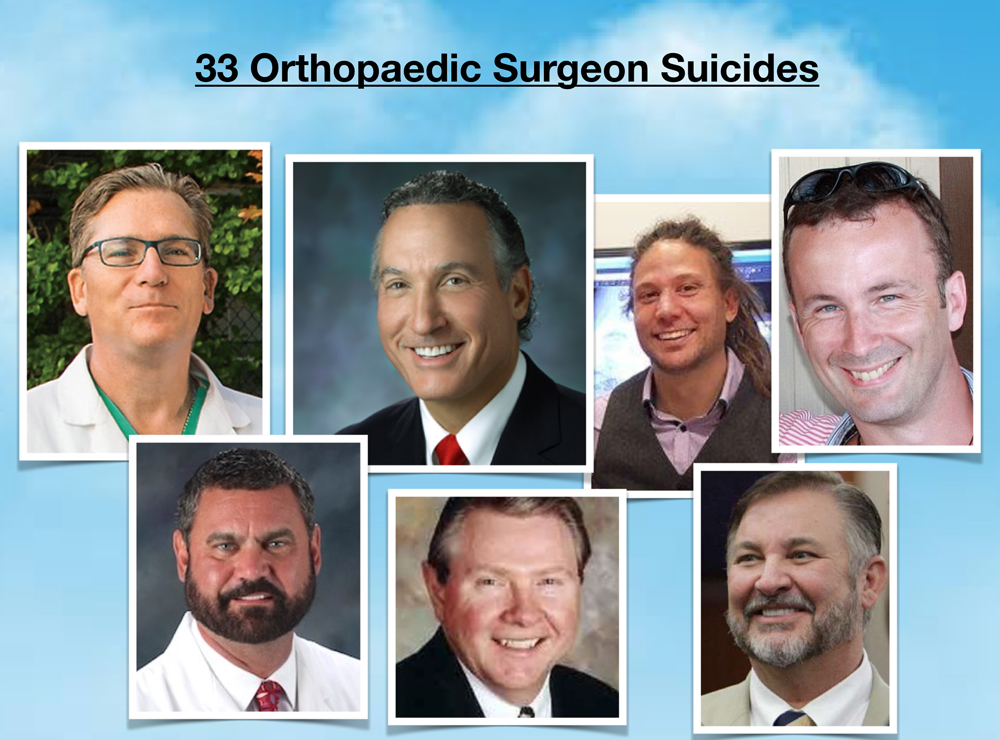
I’d like to dedicate my presentation today to Dr. Dean Lorich—and to the many orthopaedic surgeons we’ve lost to suicide. I’ve had the opportunity to get to know many of these men through their colleagues who reported their suicides to me and more intimately through their mothers, sisters and children left behind.
Today, for the first time, I’m sharing my data—what I’ve discovered from investigating more than 1000 doctor suicides—and specifically the suicides of 33 orthopaedic surgeons. Data—often devoid of emotion and humanity—means little without a human face so I’ll start by sharing the incredible lives of two orthopaedic surgeons whom I deeply admire, Dr. Steven Ortiz and Dr. Benjamin Shaffer.
Most of you know Dean. Just curious how many of you know Steve or Ben?
Though we know each other professionally, how many of you feel you really know each other personally—the deep feelings and inner world of your colleagues? I want you to truly know these two men—not just as skilled surgeons—but as the amazing human beings we were blessed to have on this planet. And then I’d like to invite you to get to know each other (while you are still living) as deeply as I’ve gotten to know Steve and Ben posthumously. I’ll begin with Ben . . .
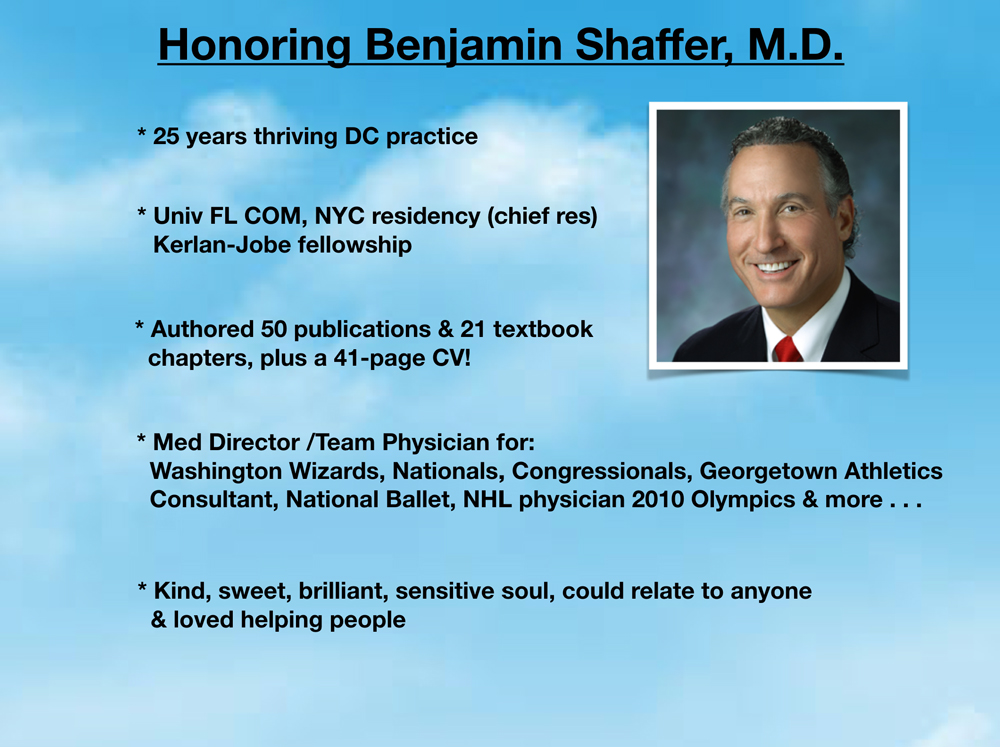
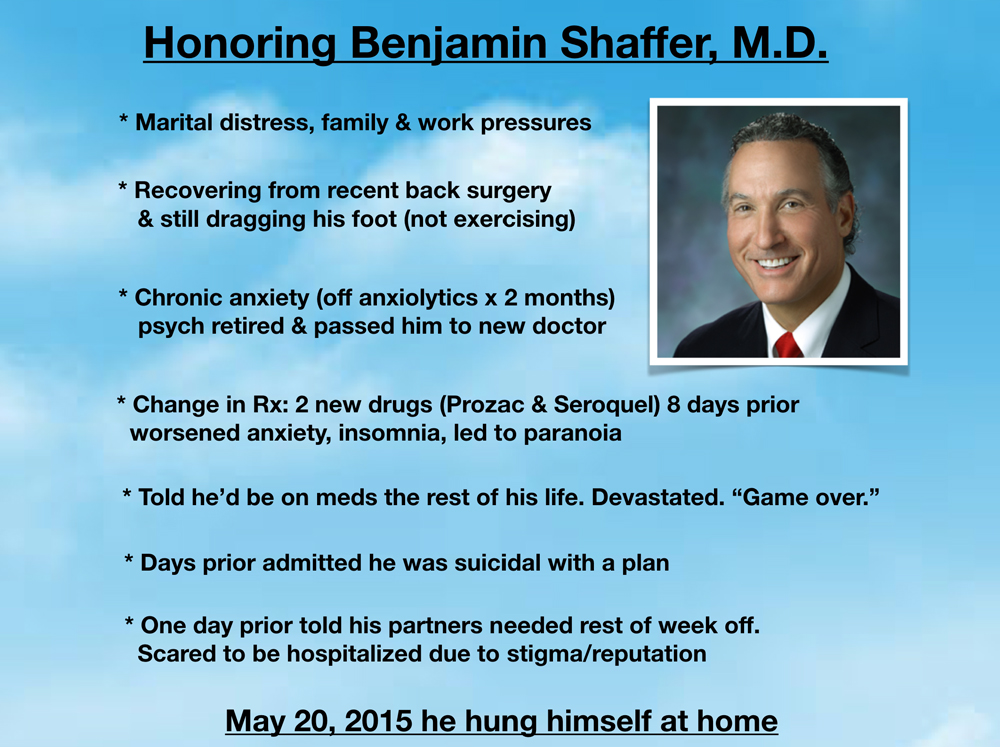
The orthopedic community suffered a devastating loss with the suicide of Dr. Ben Shaffer. He was in practice 25 years as a much beloved and trusted orthopaedic surgeon in Washington DC. Dr. Shaffer graduated from the University of Florida College of Medicine, completed his orthopaedic residency in NYC where he was chief resident, then specialized in sports medicine with a fellowship at the Kerlan-Jobe Orthopaedic Clinic.
The author of more than 50 publications (21 were textbook chapters), Dr. Shaffer trained orthopaedic surgeons around the world. He has an impressive 41-page CV (officially the longest I’ve ever read). He was the medical director or team physician to a gazillion professional sports teams in the DC area. Dr. Shaffer was also consultant to the National Ballet, NHL physician for the 2010 Olympics in Vancouver, PGA Golf Tour, Women’s World Cup Skating, and the list goes on . . . Impressive! Right?
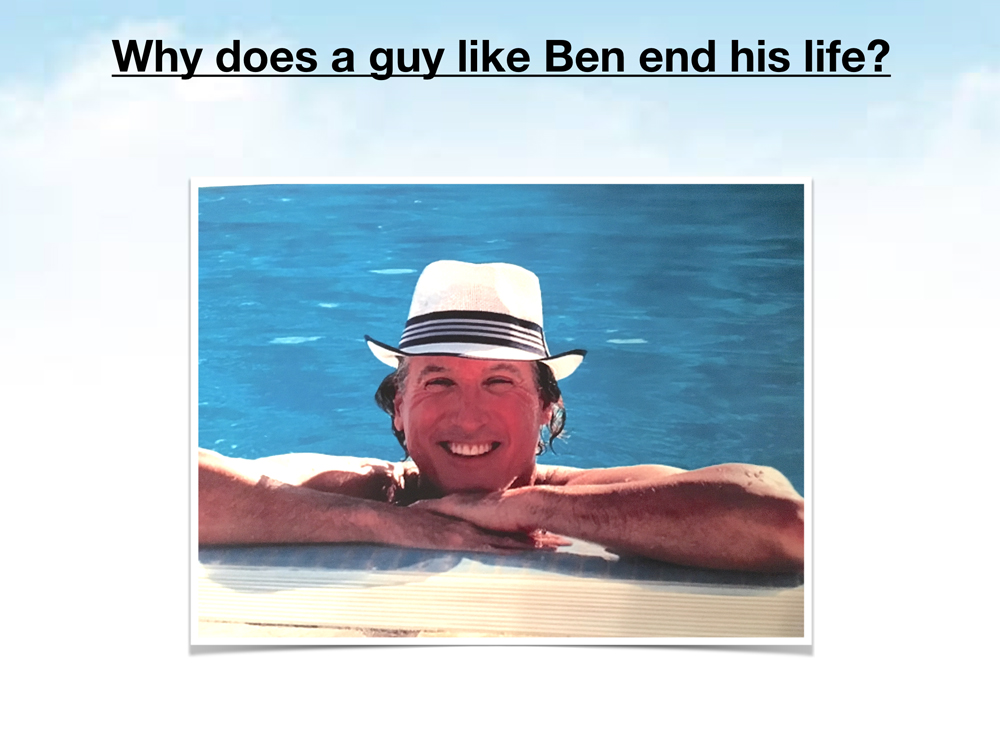
Yet Ben was more than a surgeon, he was a kind, sweet, brilliant sensitive soul who could relate to anyone—from inner city children to supreme court justices. He was gorgeous and magnetic and he loved helping people. So why does a guy this successful end his life?
As with most suicides Ben’s was multifactorial. He had marital distress, diminishing reimbursement, and personal health problems. He was recovering from recent back surgery and still dragging his foot so he couldn’t run or work out (activities that would have made him feel better).
Ben also had chronic anxiety. He saw multiple therapists during his lifetime. His psychiatrist had recently retired and passed him on to a new one who didn’t know him. He had been on anxiolytics for years and was weaned off two months before his suicide. Ultimately it was Ben’s uncontrolled anxiety and insomnia (related to sudden change in medication regimen) that led to his death. For insomnia, he was told to take Benadryl or meditate—both ineffective as he was still sleeping just two or three hours per night and trying to operate and see patients each day.
Eight days before he died, he was prescribed Prozac and Seroquel which worsened his insomnia, increased his anxiety, and led to paranoia. Then his psychiatrist told Ben he’d be on medication for the rest of his life. Ben was devastated, hopeless that he’d ever have a normal life. Ben told his sister he felt backed into a corner with no good options and it was “game over.”
Days before Ben died, his therapist asked him if he was thinking of suicide and he said, “Yes.” He then asked Ben if he knew how he would do it and Ben said, “Yes.” He then asked, “Are you going to do it?” Ben said, “No.” (Ben was smart enough to know that “yes” could potentially cause a problem for a physician.)
Ben knew he should check himself into a hospital, but he was panicked because of career ramifications due to the stigma attached to doctors seeking help for mental health. He was terrified that he’d lose his patients, his practice, his marriage, and that everyone in DC—team owners, players, patients, colleagues—would know about his mental health problems and he’d be shunned.
The night before he died, Ben finally told his partners he needed the rest of the week off because he wasn’t sleeping well. He was ashamed, yet they were fine covering for him. Ben left the hospital in sheer terror. He wanted to tell them that he had changed his mind.
Though he had slept that night, he awoke utterly wiped out on May 20, 2015. He had just returned from driving his son to school when he hanged himself on a bookcase with rope from a box that had been delivered earlier in the week. He left no note. He left behind his wife and two children.
Dr. Steve Ortiz had a very different career trajectory, yet suffered the same outcome as Ben.
Steve was one of the most thoughtful, kind, compassionate, and highly ethical men you could ever hope to meet—especially if you needed back surgery.
Though we never met, I feel I know his heart and soul as my brother in medicine. Maybe it’s because we’re the same age and he went to Sheldon High School right down the street from me in Oregon.
After high school, Steve was a sprinkler fitter for 10 years then did construction. One time when working construction, Steve tore his meniscus. He had surgery immediately. On follow up when the doctor showed him his x-ray he almost passed out and had to be helped to sit down by the nurse. He literally couldn’t stand looking at his own x-ray.
He returned to school at 28 earning a chemistry degree from Fullerton Community College then a full scholarship to UC Irvine and Stanford Medical School, orthopaedic residency in New York and spine surgery fellowship in Minneapolis—a total of 19 years of medical education!
Steve was one of those unusual guys who never forgot birthdays, holidays, or his family on special occasions. You’ll never guess what he did for his daughter’s thirteenth birthday . . .
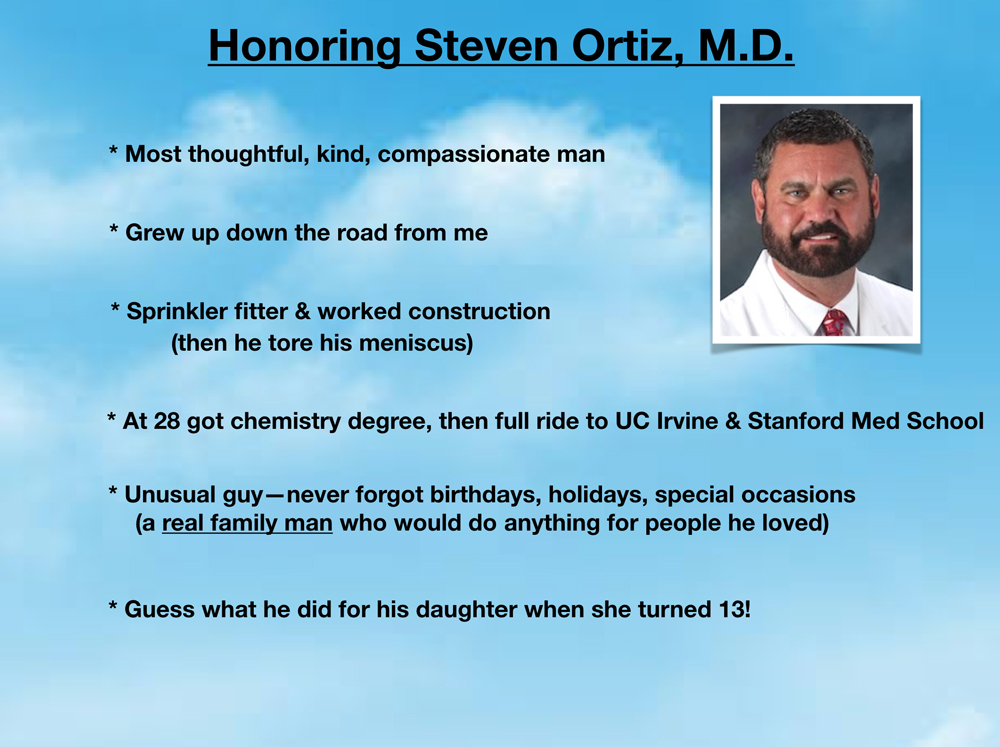
Since Steve had moved his family to Stanford for med school just before his daughter turned thirteen, she hadn’t made many friends so didn’t know how to celebrate her birthday. On her birthday her dad came home and told her he rented the entire medical school auditorium for the afternoon and he invited her whole soccer team to watch a movie and help her celebrate. He even rented a popcorn machine and bought everyone candy.
Yet Steve—such a devoted family man—had to sacrifice relationships with the very people he loved the most so he could help and heal others. With his kids and wife finally settled in California, he was distraught having matched in New York for orthopaedics. During his five years of residency he only got to see his kids once each year. That marriage eventually failed and he remarried a woman who wanted to be near her family in Florida. So, of course, Steve agreed. (He had trouble saying no!) After fellowship, he set up his practice in a Florida hospital where he was adored by patients and staff (just read comments on his suicide news article). He was always ready to help others. When one of his patients became ill, he flew home from his vacation to care for her!
Steve—the ultimate fix-it-guy—didn’t like when things were in disrepair. There was a huge pothole in the hospital parking lot that was driving everyone crazy, but it was never taken care of by the powers that be until Steve went to a local hardware store and bought several bags of cement and gravel. Imagine a spine surgeon out in the hospital parking lot repairing potholes before work.
But Steve’s problems with the hospital were deeper than parking lot potholes.
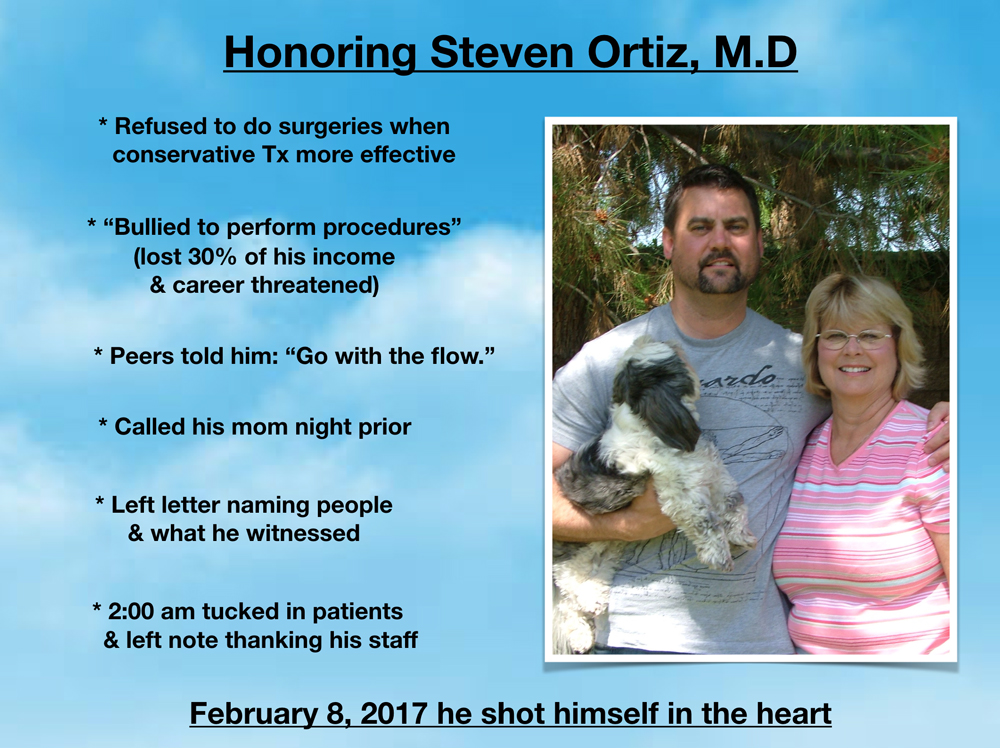
He refused to do surgeries when conservative treatments would be safer and more effective, particularly for elderly patients. Yet the hospital was making money from all these procedures and Steve felt he was being bullied to perform unnecessary surgeries. His colleagues said he should just “go with the flow.” He wanted to leave and they wouldn’t let him. They referred fewer patients to him and he lost 30% of his income. They threatened to ruin his career.
He called his mother the night before he killed himself to share these details. She knew none of these challenges he faced every day until that 30-minute phone call. He had already planned it. At 5:00 pm the night before he wrote a letter naming people and what he witnessed. (Due to an active investigation I’m not at liberty to share more.)
Dr. Ortiz was an open-hearted truth teller, a whistleblower who had only been out of training for three years. On February 8, 2017 at 2:00 am he tucked his patients in and wrote orders to make sure they were all okay. He sent a thank you note to a surgical nurse asking her to thank all his staff for taking wonderful care of his patients. In that note, he told her he decided to “check out.” At 3:00 am he went out to the hospital parking lot (the one where he repaired the pothole) sat down in his truck, and shot himself in the heart.
So how did I get involved in these crime scenes? Why am I so obsessed with doctor suicides? Three reasons. 1) I was a suicidal physician in 2004. I thought I was the only one. Maybe I was just too sensitive and idealistic. I have a personal stake in this issue. I feel it to my core. 2) Eight years later, I discovered doctor suicide is quite literally a hidden epidemic! It came as an absolute shock that so many of my colleagues were dying by suicide. 3) What created my relentless 24/7 obsession was the discovery that these suicides were being covered up—by my very own profession! That’s when I got pissed and I couldn’t shut up.
Full disclosure: I have OCD. My obsession—my disturbing recurrent thoughts that I ruminate over are about why all these doctors are dying by suicide. My compulsion—my daily (even hourly) ritual is tracking all the names and details of each case as they come to me. I’m a strong believer of channeling my mental illness into something productive. So rather than wash my hands compulsively, I’m tracking doctor suicides. By nature, I’m really more of an investigative reporter trapped in a doctor’s body. I’m the type of person who can’t stop a project until it’s completed. Like Steve, I’m a truth teller and a whistleblower. I never went looking for these suicides. These suicides found me.
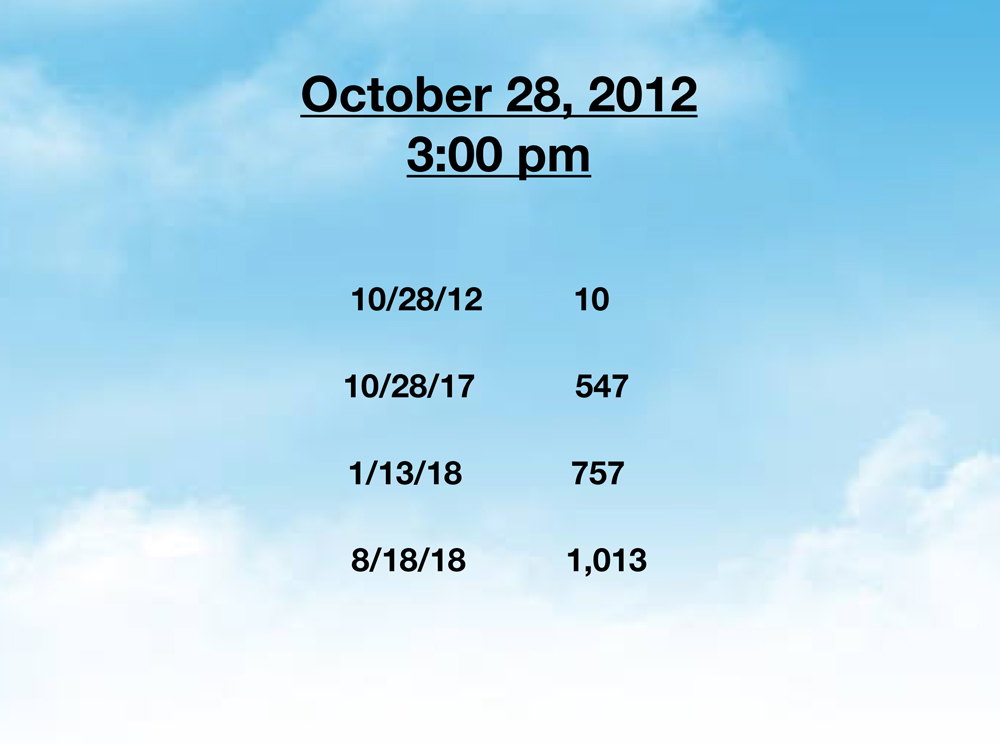
On October 28, 2012, at 3:00 pm my life changed forever.
I was sitting at the memorial service for the third doctor we lost to suicide in my small town—in just over a year. Top-rated doctors. Suddenly gone. Yet during the entire service nobody uttered the word suicide aloud. Kind of hard to solve a problem when nobody will talk about it. Everyone kept whispering “Why?” I wanted to know why. Sitting in the second row at that service I started counting dead doctors—doctors who died by suicide (or highly suspicious circumstances later confirmed as suicide). I suddenly realized BOTH men I dated in medical school—who died at 44 and 39 years old leaving wives and children behind—were likely suicides too! Later, I confirmed both overdosed.
Within a few minutes I had counted 10 doctor suicides.
I had to leave the service early because that evening I was teaching a business retreat for physicians who wanted to launch successful independent practices as I have (Yes! I’m one of the few rogue solo docs out there stilling doing house calls). On my two-and-a-half-hour drive up into the mountains I continued to obsess on doctor suicide: Maybe it’s just the men that I date who die by suicide . . . Maybe Eugene, Oregon, is a hotbed of physician suicides. (People have actually accused ME of only dating guys who die by suicide and choosing to live in a town where so many doctors die by suicide.) Am I really the only one losing my friends, lovers, colleagues to suicide—ALL of them doctors!? (FYI: I’ve never lost any non-physicians in my life to suicide.)
When I arrived at the retreat, I opened the initial session with two questions: “How many of you have lost a doctor to suicide?” All hands were raised. Then I asked, “How many of you have considered suicide?” All hands remained up—including mine—except for a female nurse practitioner. By the end of the retreat they had all submitted names of these doctors on sticky notes, scraps of paper, and index cards.
So I started a doctor suicide diary as a way to track all of these suicides. I bought a beautiful journal with clouds (much like the background on my slides) where I began handwriting all the names and details. Five years later I had a registry with 547 doctor suicides. By then I obviously had to transfer all the data to an online spreadsheet where I’m tracking by case number, name, age, specialty, date, location and method suicide, plus any circumstances or backstory. All the while I keep relentlessly writing and speaking about doctor suicide—and people keep contacting me with more and more names for my registry.
I never went looking for these suicides. These suicides found me.
By January this year, I had 757 cases on my registry. As of today I have 1,013.
Meanwhile my house has turned into a shrine for our lost colleagues with entire walls covered with photos of suicided doctors and medical students. And because so many people keep calling and writing me, I’ve been running a de facto doctor suicide hotline from my home for nearly six years now. Yes, I’m up at all hours of the night on the phone with doctors I’ve never met who are having panic attacks at work in between patients and others who are sobbing on the phone with me. Again, I never intended to run a suicide hotline, yet doctors keep calling and I keep answering the phone. Truly a labor of love. After speaking to thousands of suicidal doctors and medical students, I now have a depth of understanding about physician psychology and suicide that is probably very unique in the world.

Here’s what I’ve learned from 1,013 doctor suicides.
High doctor suicide rates have been reported since 1858. Yet 160 years later the root causes of these suicides remain unaddressed.
Physician suicide IS a public health crisis. One million Americans lose their doctors each year to suicide. Yet they are never informed the real reason why they can’t see their doctor who just saved their life or delivered their first child. They’re told to just pick another doctor!
Many doctors have lost several colleagues to suicide. Some have lost up to eight during their career. With no chance to grieve. In fact many medical institutions don’t offer grief counseling services or allow any time off for surviving colleagues who are often forced to work more hours to cover the shifts of their suicided peers—and may not even be permitted to attend their funerals!
We lose more men than women. For every woman who dies by suicide on my registry, we lose four men.
Suicide methods vary by region and gender. Women prefer to overdose and men choose firearms. Gunshot wounds prevail out west. Jumping is popular in New York City. In India doctors are found hanging from ceiling fans.
Male anesthesiologists are at highest risk. Most die by overdose. Many are found dead in hospital call rooms. Google “doctor found dead in hospital” and I would bet most are male anesthesiologists.
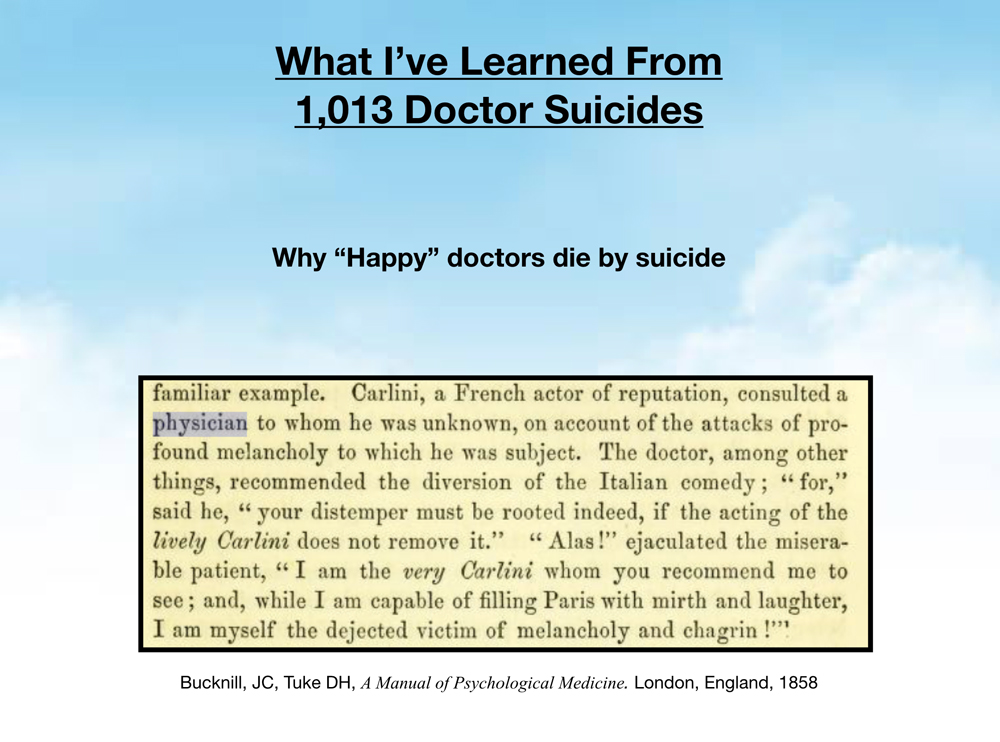
“Happy” doctors die by suicide. Many doctors who die by suicide are the happiest most well-adjusted people on the outside. Just back from Disneyland, just bought tickets for a family cruise, just gave a thumbs up to the team after a successful surgery—and hours later they shoot themselves in the head. Doctors are masters of disguise. Even fun-loving happy docs who crack jokes and make patients smile all day may be suffering in silence. We are all at risk.
There is this perception that “happy” people don’t die by suicide, yet often the people who are most happy on the outside—the very people who spend their days making other people happy (maybe a coping strategy?)—are the ones who are terribly lonely and depressed. Consider reaching out to your “happy” colleagues to see how they are doing.
When I read this excerpt from the 1858 Manual of Psychological Medicine I kept thinking of Robin Williams and all the happy doctors we’ve lost to suicide:
“Carlini, a French actor of reputation, consulted a physician to whom he was unknown, on account of the attacks of profound melancholy to which he was subject. The doctor, among other things, recommended the diversion of the Italian comedy; “for,” said he, “your distemper must be rooted indeed, if the acting of the lively Carlini does not remove it.:” “Alas! ejaculated the miserable patient, “I am the very Carlini whom you recommend me to see; and, while I am capable of filling Paris with mirth and laughter, I am myself the dejected victim of melancholy and chagrin.”
Sensitive souls are at highest risk. Some of the most caring, compassionate, and intelligent doctors choose suicide rather than continuing to work in such callous, uncaring and ruthlessly greedy medical corporations.
Doctors have personal problems—like everyone else. We get divorced, have custody battles, infidelity, disabled children, deaths in our families. Working 100+ hours per week immersed in our patients’ pain, we’ve got no time to deal with our own pain. (Spending so much time at work actually leads to divorce and completely dysfunctional personal lives).
Doctors develop on-the-job PTSD. Especially true in emergency medicine and surgical specialties. Then one day they “snap” like this guy, a friend of mine who against all odds survived his suicide attempt to now enlighten others.
Patient deaths hurt doctors. A lot. Even when there’s no medical error, doctors may never forgive themselves for losing a patient. Suicide is the ultimate self-punishment for the perfectionist.
Malpractice suits kill doctors. Humans make mistakes. Yet when doctors make mistakes, they’re publicly shamed in court, TV, and newspapers (that live online forever). We continue to suffer the agony of harming someone else—unintentionally—for the rest of our lives.
Doctors who do illegal things kills themselves. Medicare fraud, sex with a patient, DUIs may lead to loss of medical license, prison time, and suicide. Even doctors who witness unethical things are at risk of suffering and not being protected as whistle blowers as noted above.
Assembly-line medicine kills doctors. Brilliant, compassionate people can not care for complex patients in 10-minute slots. When punished or fired for “inefficiency” or “low productivity” doctors may choose suicide. Pressure from insurance companies and government mandates further crush the souls of these talented people who just want to help their patients. Many doctors cite inhumane working conditions in their suicide notes. (Assembly-line medicine was 100% responsible for my suicidality in 2004. Thankfully launching my independent practice cured me!)
Bullying, hazing, and sleep deprivation increase suicide risk. Medical training is rampant with human rights violations illegal in all other industries. Physicians have suffered hallucinations, life-threatening seizures, depression and suicide solely related to sleep deprivation. Resident physicians are now “capped” at 28-hour shifts and 80-hour weeks. If doctors-in-training “violate” work hours (by caring for patients) they are forced to lie on their timecards or be written up as “inefficient” and sent to a psychiatrist for ADHD medications. Some doctors kill themselves for fear of harming a patient (or because they did harm a patient) from extreme sleep deprivation.
Blaming doctors increases suicides. Words like “burnout” and “resilience” are often employed by medical institutions to blame and shame doctors while deflecting attention from inhumane working conditions. When doctors are punished for occupationally-induced mental health conditions (while underlying human rights violations are not addressed), they become even more hopeless and desperate.
Doctors fear lack of confidentiality if they seek mental health care. So they drive out of town, pay cash, and use fake names to hide from state medical boards, hospitals, and insurance plans that ask doctors about their mental health and may then exclude them from state licensure, hospital privileges, and health plan participation. (Even when confidential care is available, physicians have little time to access care when working 80-100+ hours per week).
Medical board investigations may increase suicide risk. One doctor hung himself from a tree outside the Florida medical board office after being denied his license. In several of these orthopaedist suicides, ongoing hospital review or loss of privileges played a primary role in their suicides.
Doctors choose suicide to end their pain (not because they want to die). Suicide is preventable. We can help doctors who are suffering if we stop with all the secrecy and punishment. Why not support and care for the people who are here to care for us?
Ignoring doctor suicides leads to more doctor suicides. Thankfully an Emmy-winning filmmaker has completed a documentary that is now shining a light on the physician suicide crisis. View movie trailer here & attend a screening.
Doctor suicide notes reveal the true cause of suicide. Why aren’t we studying these notes? I have a book of suicide letters I’ve published from 53 doctors (many writing to me debating the pros/cons of dying by suicide). The reasons doctors die by suicide are in the book. Download free audiobook here.
Doctors have a great work ethic until the end! Yes, we literally are checking on our patients, reviewing critical labs, and completing out chart notes before we orchestrate our suicides.
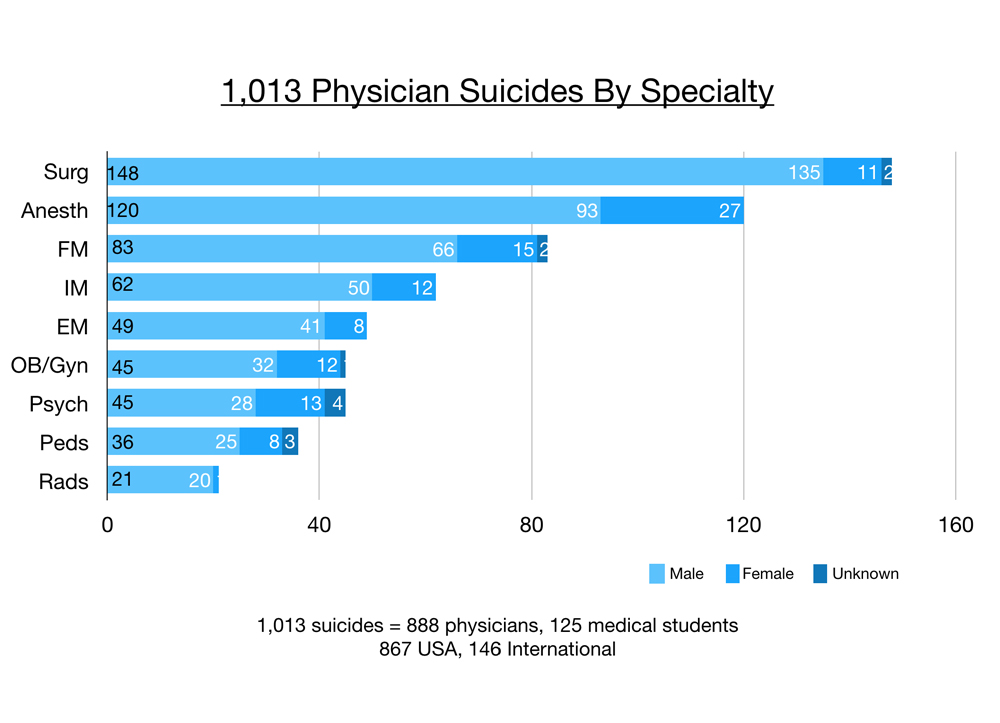
I’ve analyzed 1,013 physician suicides by specialty that have come to me via friends, family, colleagues over the past six years. Of these 1,013, 888 are physicians and 125 are medical students. The majority (867) are suicides in the USA and 146 are international. Surgeons (including surgical subspecialties excluding OB/gyn) have the greatest number of suicides, then anesthesiologists, family docs, internal medicine, emergency medicine, OB/gyn, psychiatry, pediatrics, and radiology. Males (light blue) far outnumber females (darker blue) in all suicides per specialty. The darkest blue represents doctors who have died by suicide with incomplete data on gender.
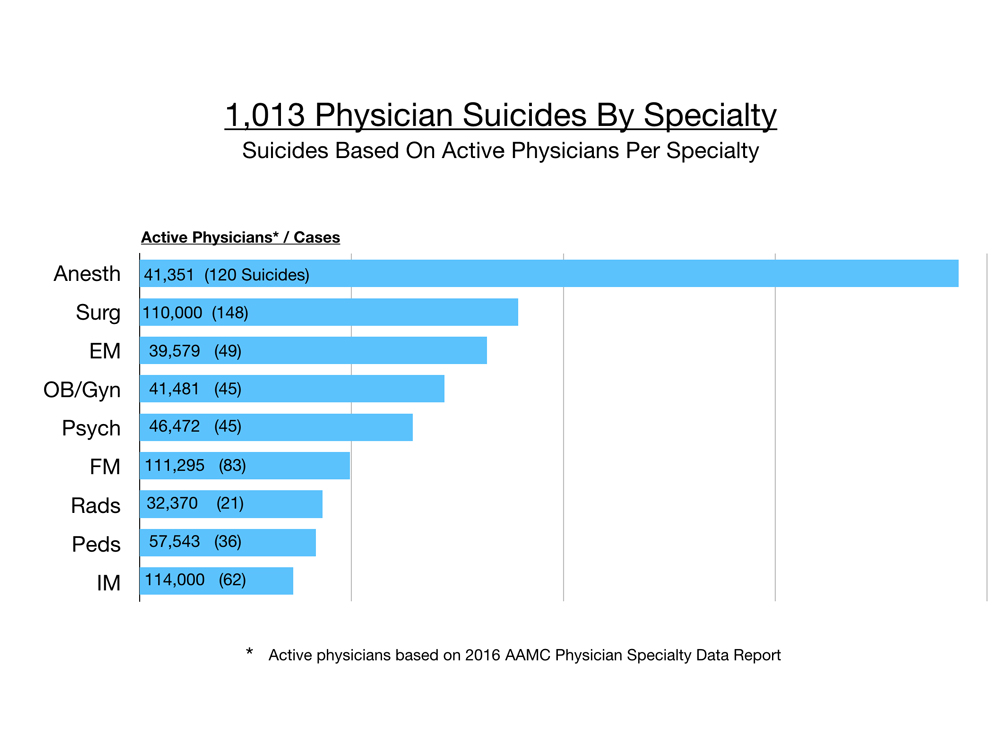
However, when accounting for numbers of active physicians per specialty, anesthesiologists are off the chart and far in the lead. Surgeons are number two, then emergency docs, OB/gyn, and psychiatry. Physicians per specialty are from the 2016 AAMC Physician Specialty Data Report that measured only the active physicians in the largest specialties. Still this gives us a sense of the prevalence of suicide per specialty. Then I analyzed the 148 surgeon suicides and divided them into their subspecialties.
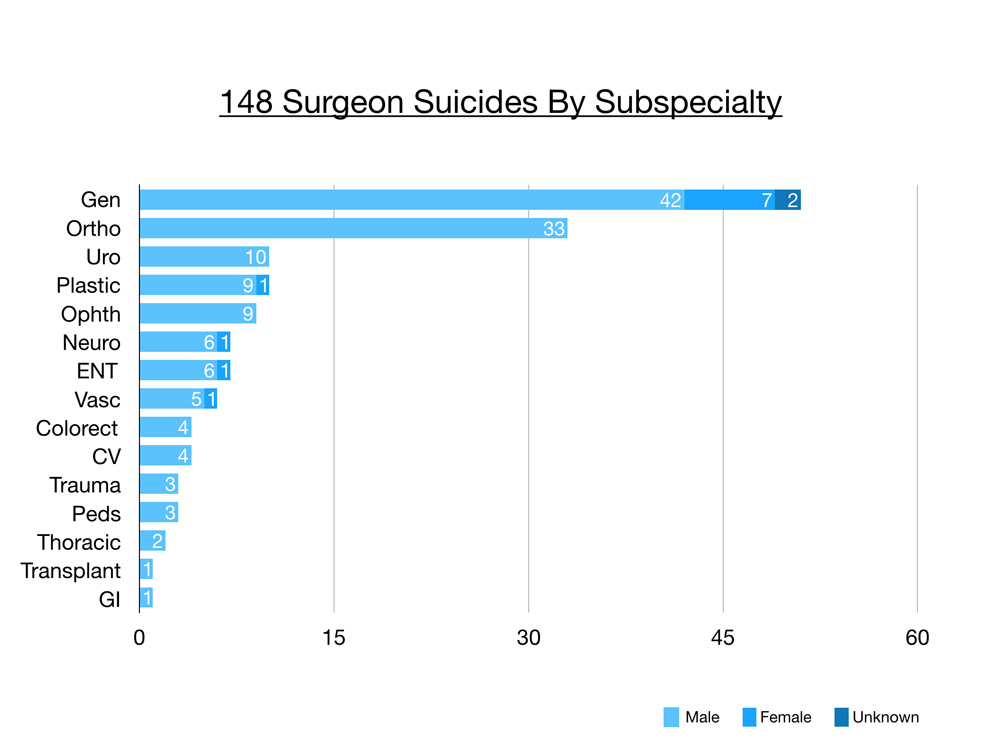
Raw numbers from my registry reveal general surgeons at 51, orthopaedic surgeons at 33, then urology and plastic surgery with 10 cases each, ophthalmology with nine, neurosurgery and ENT with seven, vascular six, and so on. Several of these surgical subspecialties only have a few thousand active practicing physicians and so the sample size is quite small and it does make it more challenging to analyze and reveal trends.
Today I’ll focus on the 33 orthopaedic surgeons we lost to suicide. Why they chose suicide. And what you can do now so that you don’t lose your own life or life of a colleague.
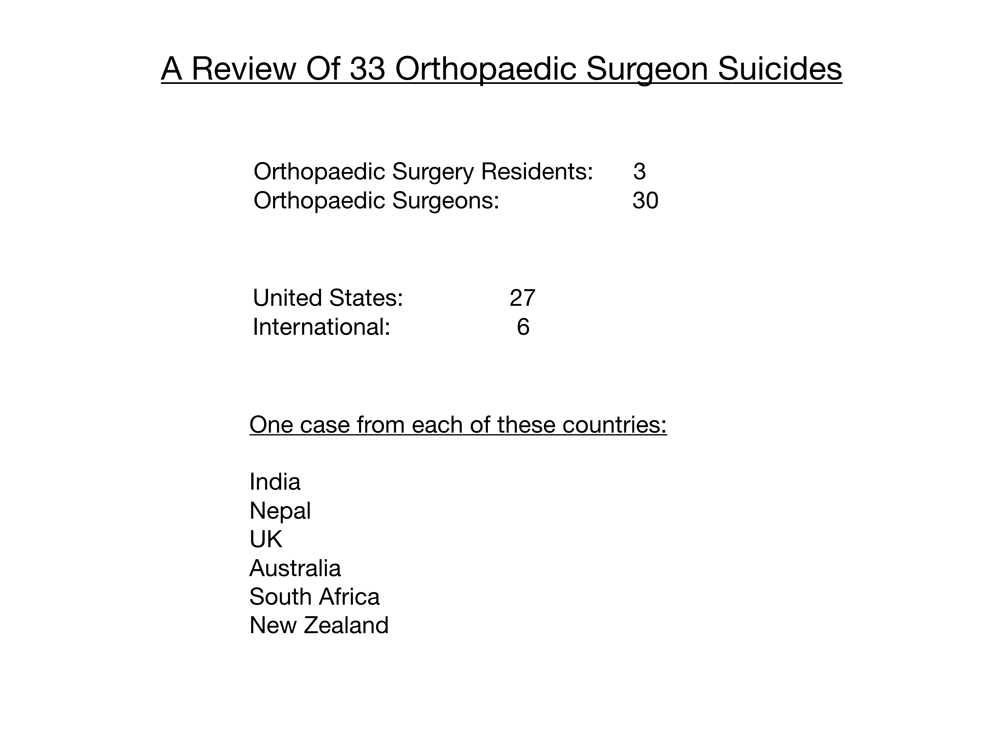
On review of the 33 orthopaedic suicides, 30 were surgeons and three were residents. Again most (27) in the USA and six cases international. One from each of the following countries: India, Nepal, UK, Australia, South Africa, New Zealand.
These numbers are the tip of the iceberg. I certainly do not have a comprehensive list, nor does anyone on the planet. Many doctor suicides are well hidden for a variety of reasons, stigma within society, the medical system, even families (who have asked me to lie about the suicides—even when video footage shows the doctor purposefully stepping off the roof of a hospital). Many times even death certificates do not specify suicide (even when there is a suicide note). Doctors may list cause of death on the death certificate as an accident (again for a variety of reasons including reputation of their colleague and life insurance payouts). Some physicians who die by suicide make their death appear to be an accident, again for reputation and life insurance.
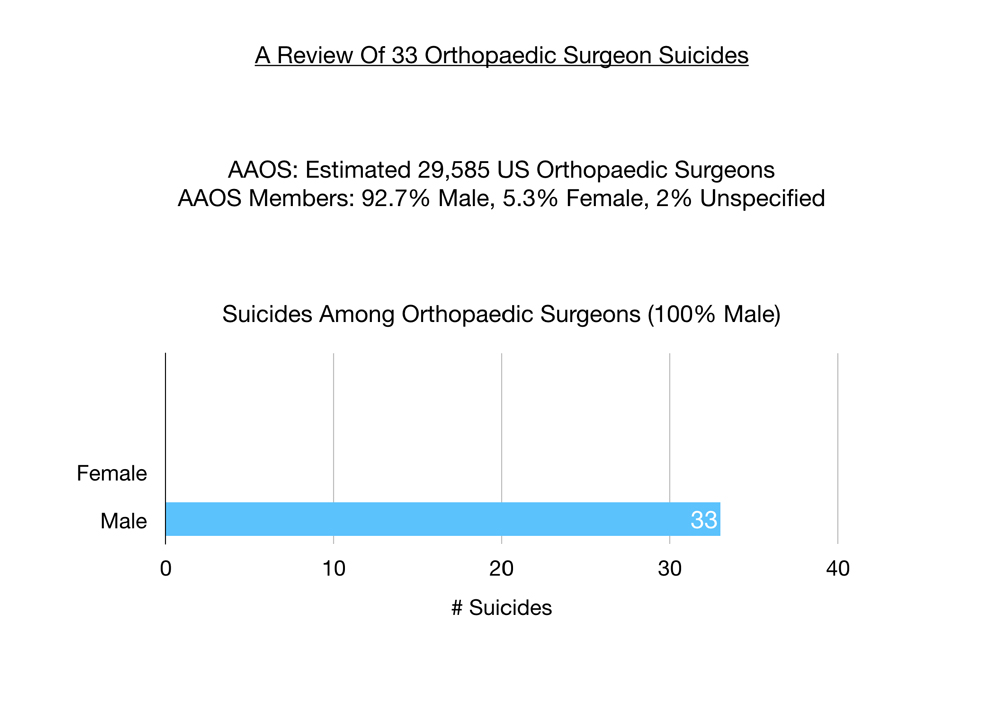
Analyzing these 33 cases of orthopaedic suicides it is not surprising that in a male-dominated specialty (apparently 93% male per AAOS) all 33 orthopaedic surgeon suicides are male.
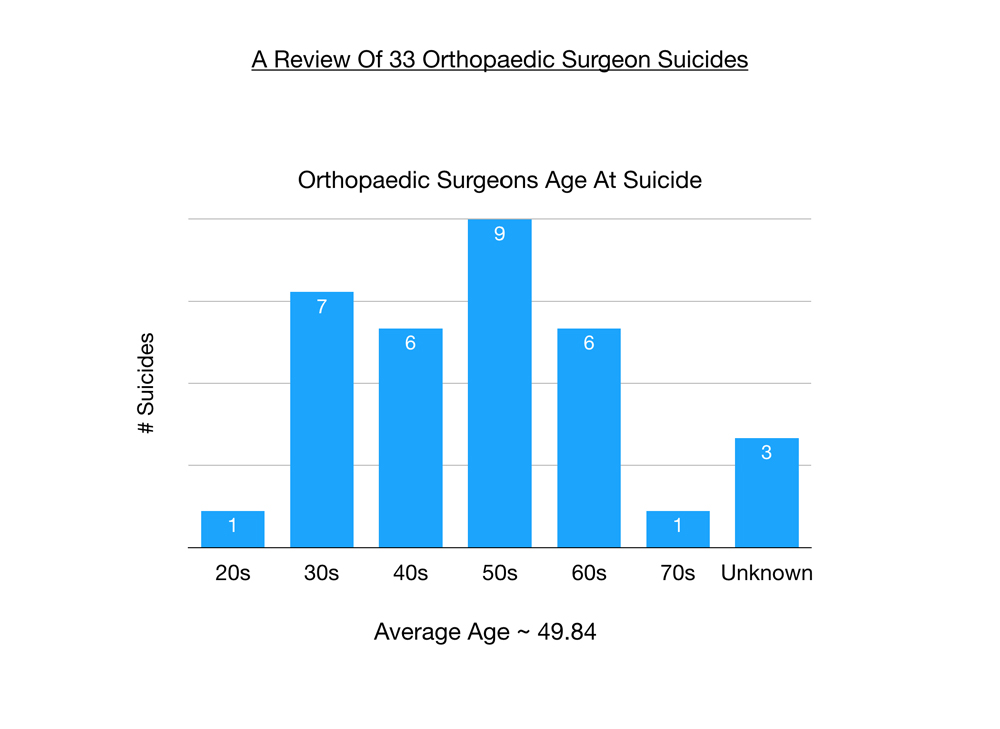
The average age at suicide among these orthopaedic surgeons is 49. Ages range from 25 to 73. Orthopaedic surgeons in their 50s tend to be a high-risk age group.
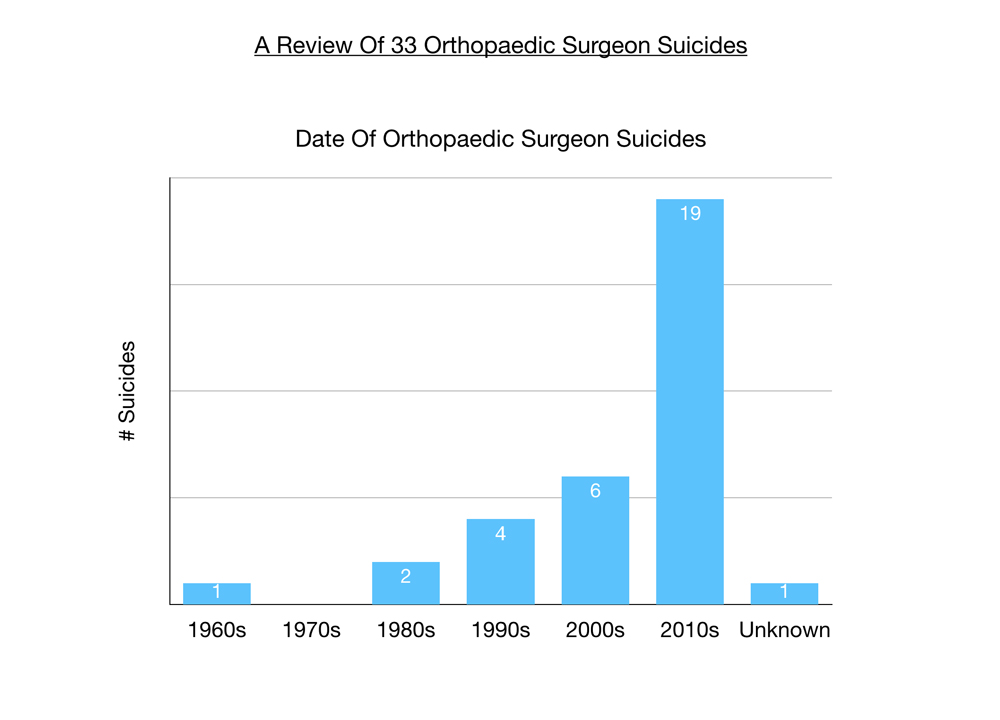
The majority of these suicides were in the last 10 years though I recently discovered one from the 1960s in my hometown.
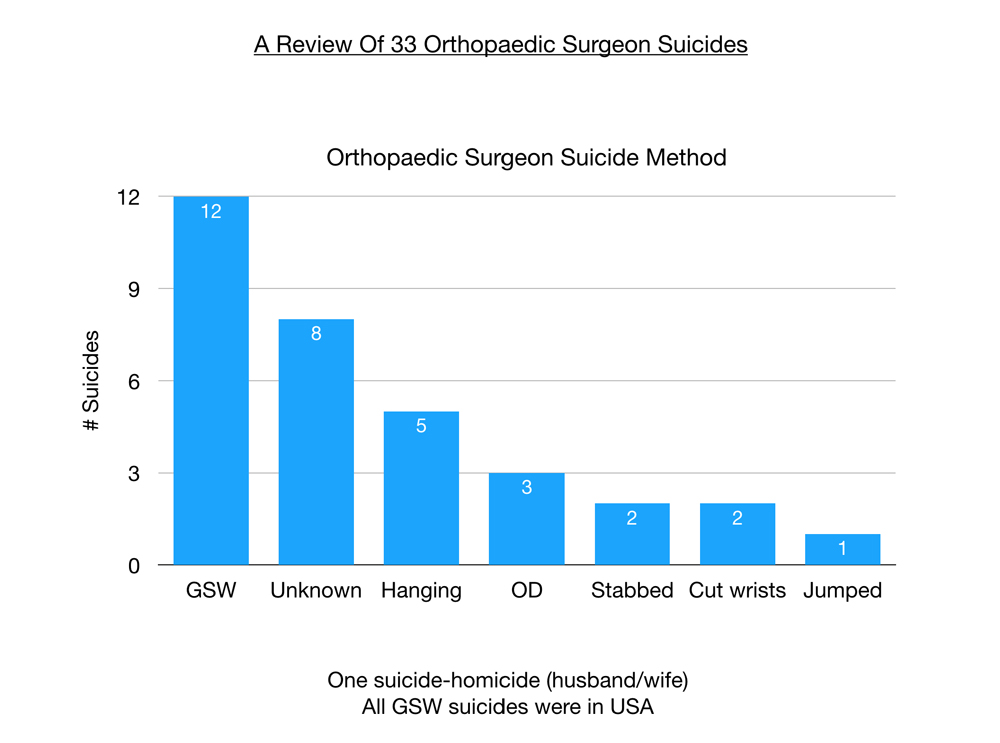
Most popular method of suicide among orthopaedic surgeons is gunshot wounds in the USA. Then hanging and overdose (these dominate overseas). Due to the taboo nature of suicide, eight of the cases reported to me by friends and colleagues have unknown method of suicide. A unique method for physicians (very uncommon in other populations) is stabbing oneself to death.
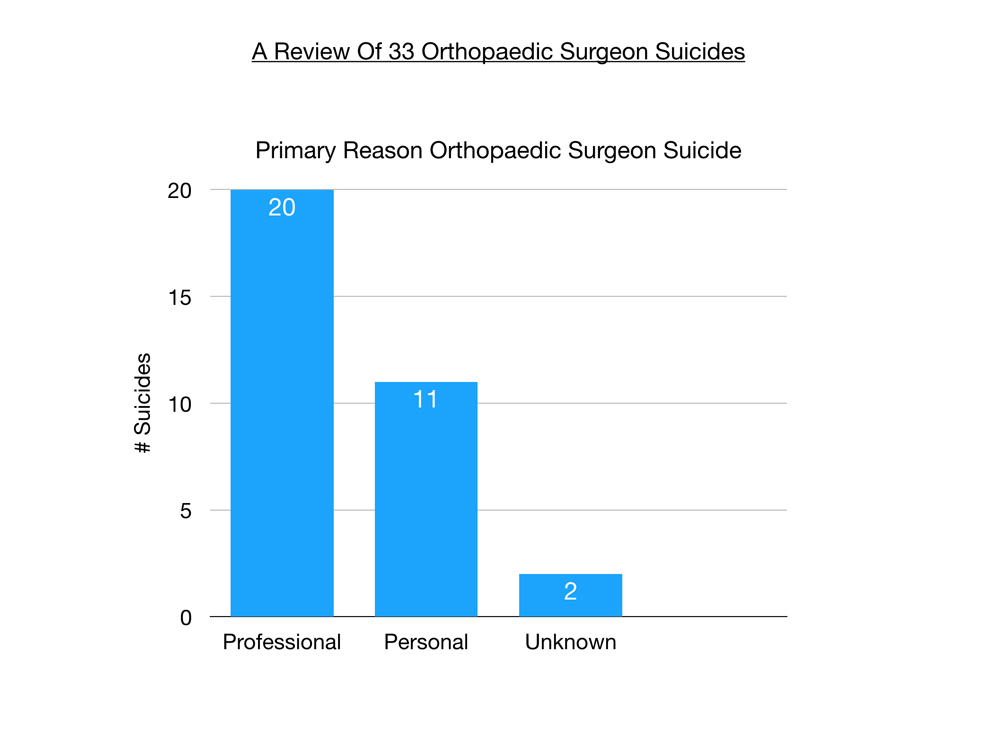
Of greatest interest to me are the reasons why doctors kill themselves. Most suicides are multifactorial, a series of events that unfold in the months leading up to the suicide. In categorizing these suicides, I was interested in the one factor at the end that made life so intolerable that these physicians saw no other way out. For orthopaedic surgeons, most are choosing suicide due to professional, not personal reasons.
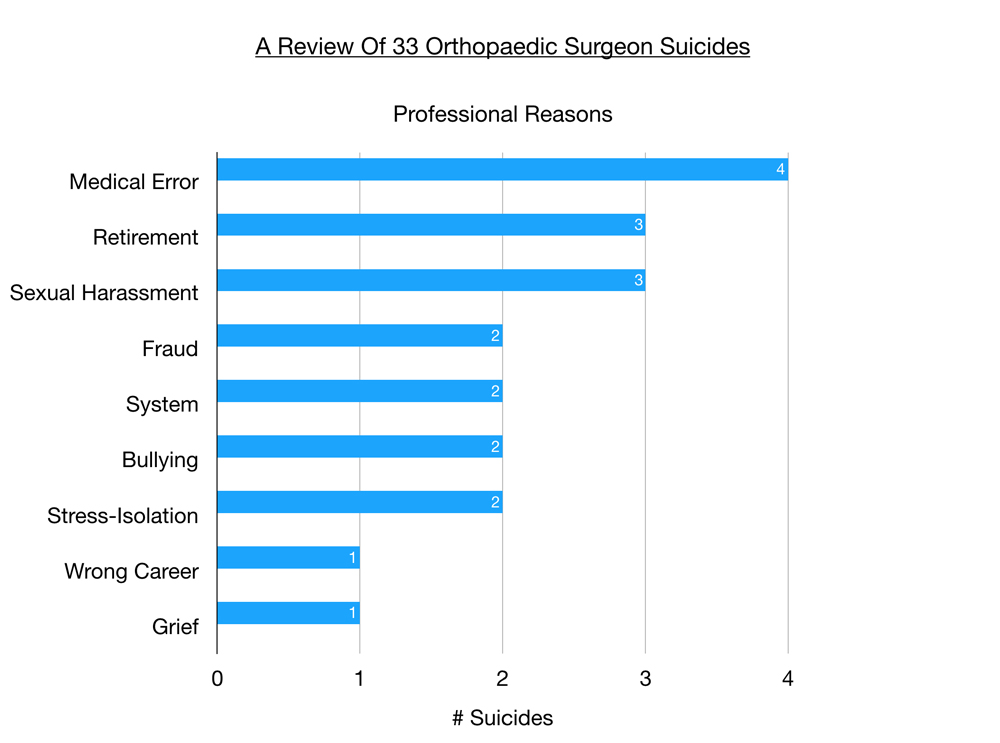
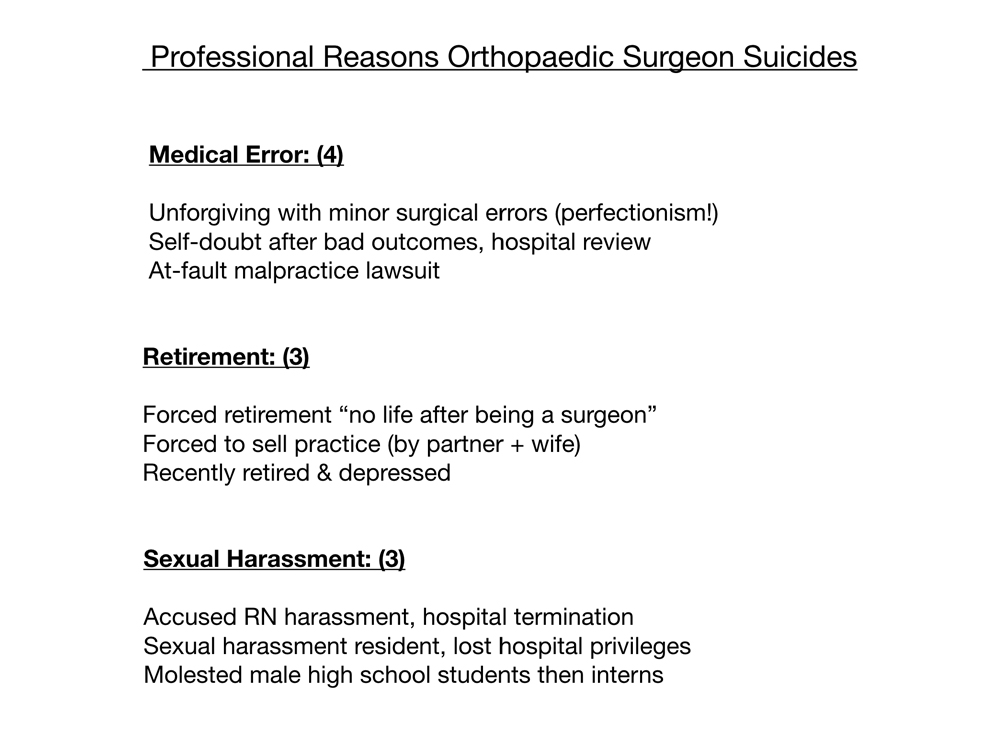
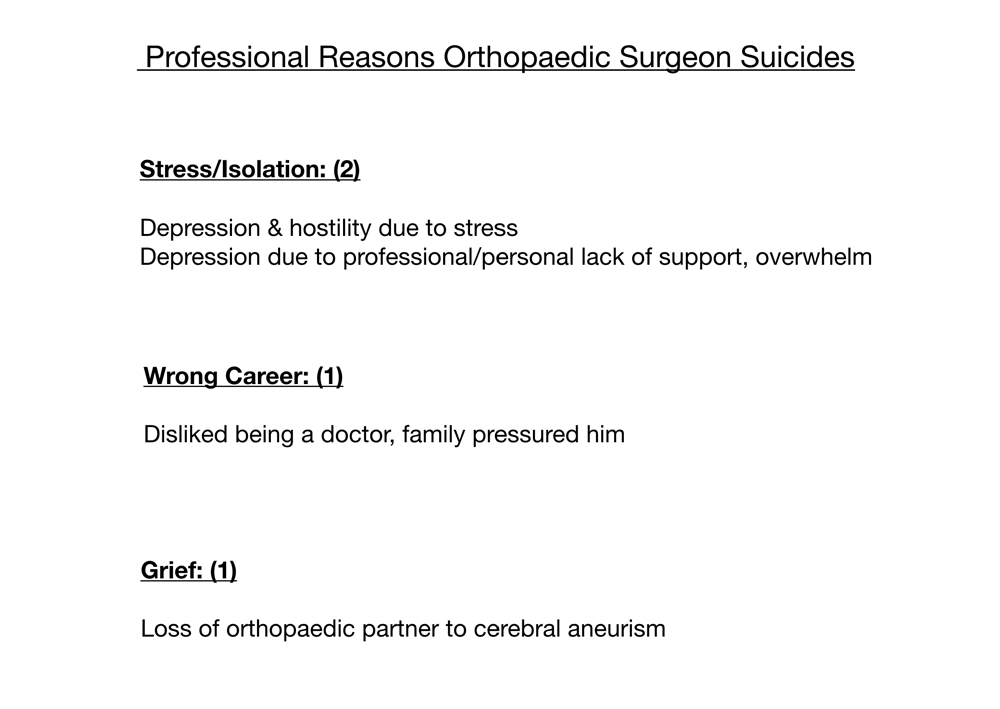
 In order of significance, are medical errors, retirement, sexual harassment (and repercussions like loss of hospital privileges), fraud, the system, bullying, stress & isolation, wrong career, and grief after sudden death of orthopaedic partner.
In order of significance, are medical errors, retirement, sexual harassment (and repercussions like loss of hospital privileges), fraud, the system, bullying, stress & isolation, wrong career, and grief after sudden death of orthopaedic partner.
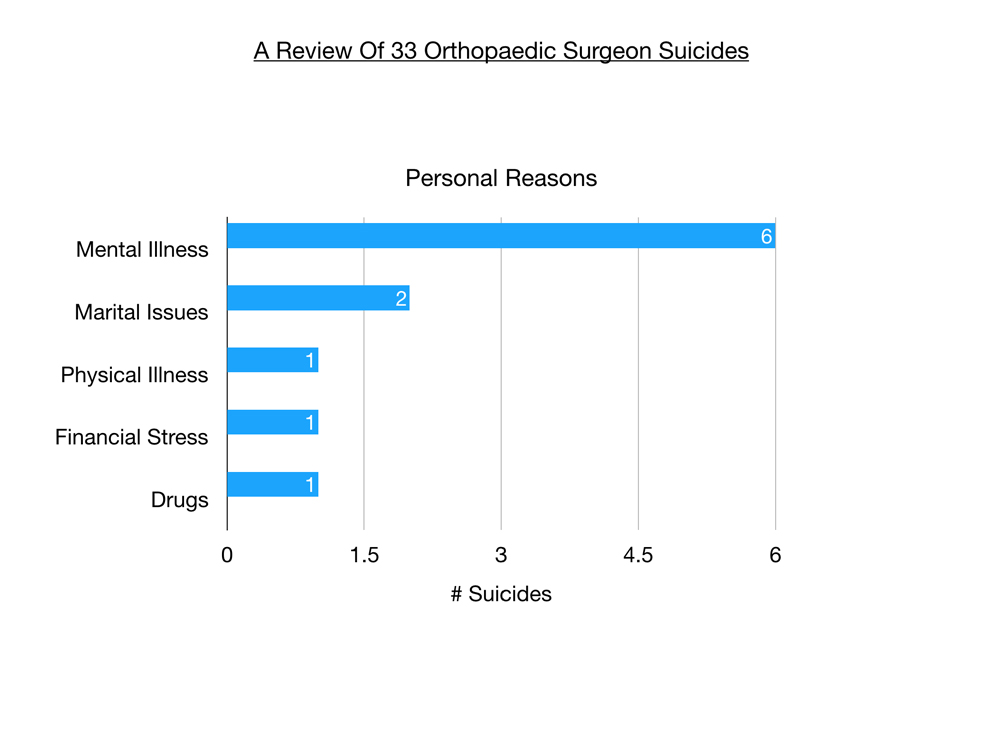
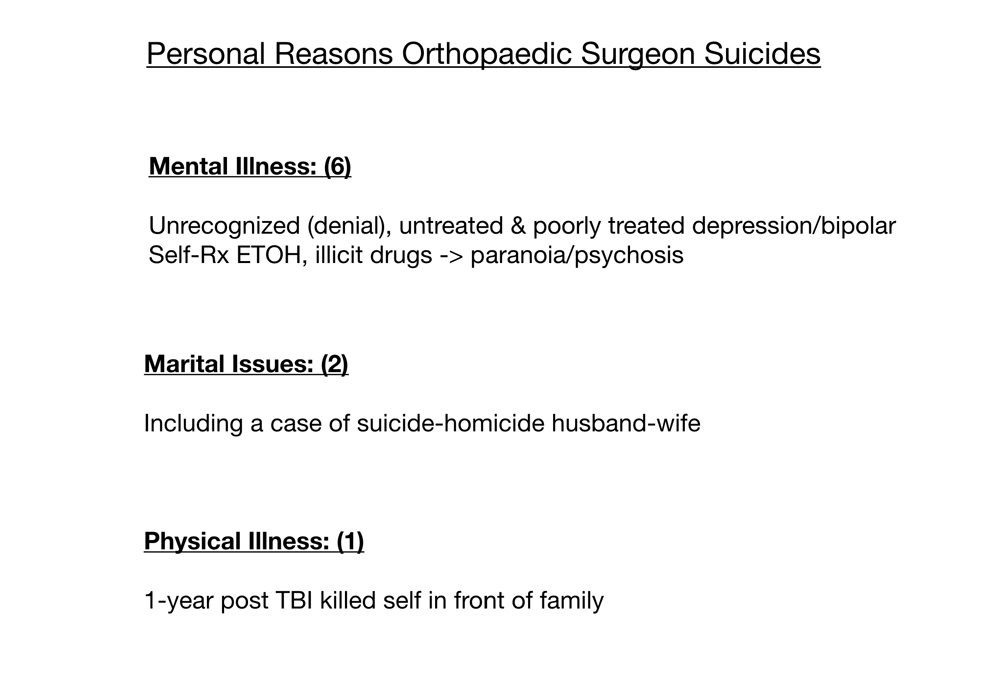
Personal reasons include mental illness, marital issues, physical illness, financial distress, and drugs.
 Top professional reason for orthopaedic surgeons choosing suicide is medical errors. Perfectionism leading to self-loathing for even minor surgical errors, self doubt after bad outcomes on knee replacements with pending hospital review, and one case involving an at-fault malpractice suit.
Top professional reason for orthopaedic surgeons choosing suicide is medical errors. Perfectionism leading to self-loathing for even minor surgical errors, self doubt after bad outcomes on knee replacements with pending hospital review, and one case involving an at-fault malpractice suit.
Next we have retirement and sexual harassment with three cases in each category. Forced retirement due to age, pressure from wife and partner to sell to hospital. When one’s identity is so wrapped up in an all-consuming career like orthopaedic surgery, who are you when you retire? Many times we are alienated emotionally from our spouse after years of working excessively and there is a risk that retirement can unearth failing marital relationships. Retirement can lead to boredom and a feeling of uselessness.
Sexual harassment as a precipitant to suicide among orthopaedic surgeons came as a complete shock to me. Sexual harassment, of course, can span the gamut from comments objectifying or sexualizing staff and other physicians to unwanted physical contact to even molesting male high school students and interns over decades. Obviously in that last case (after the police raided his home) he was heading for prison time. In the other two cases I do not have the specific details but these appear to be accusations of verbal harassment of female staff. In one case a young new surgeon wanted to date an RN and was persistent about it. She reported him for sexual harassment. The hospital consulted with their legal team that recommended he be terminated and he went home and shot himself.
Next is fraud—witnessing hospital corruption, becoming involved in a toxic department in which there is criminal activity, and feeling pressured to participate in medical care that you deem unethical, unnecessary, or even criminal.
Bullying is known to lead to suicides in middle school and high school. Bullying also is more common that we’d like to acknowledge in our residency training. One female physician told me her boyfriend from medical school was accepted into a highly-coveted orthopaedic residency. He had type 1 diabetes. Just weeks into his intern year his attending told him: “You’ll never make it with diabetes.” He went home and shot himself in the head. Others report years of ongoing subtle bullying on top of all the other stressors of practice.
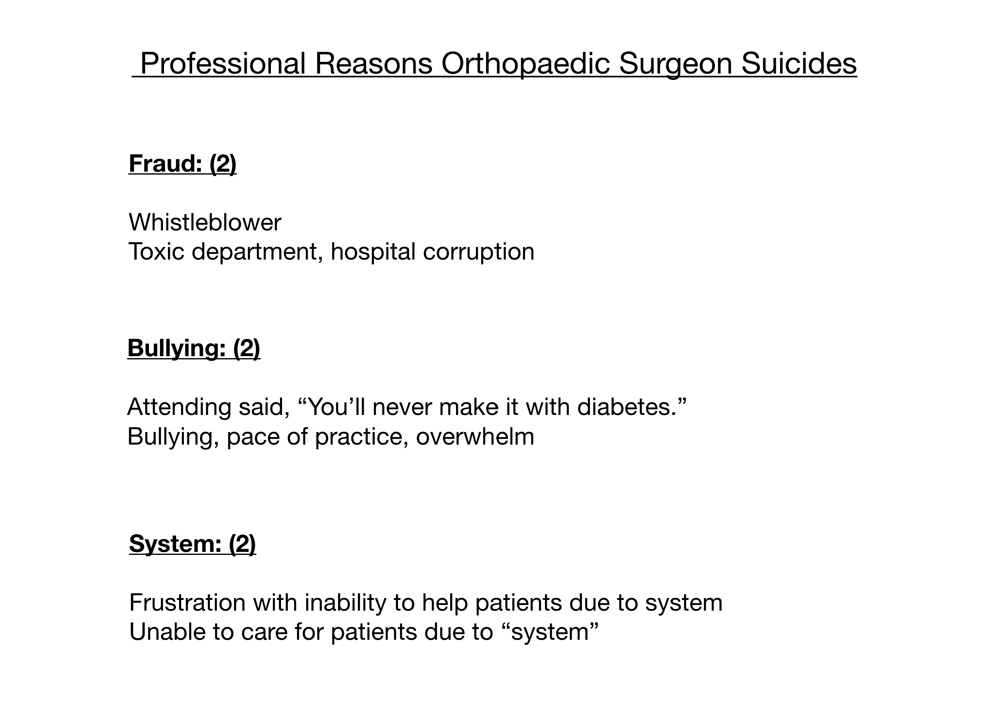
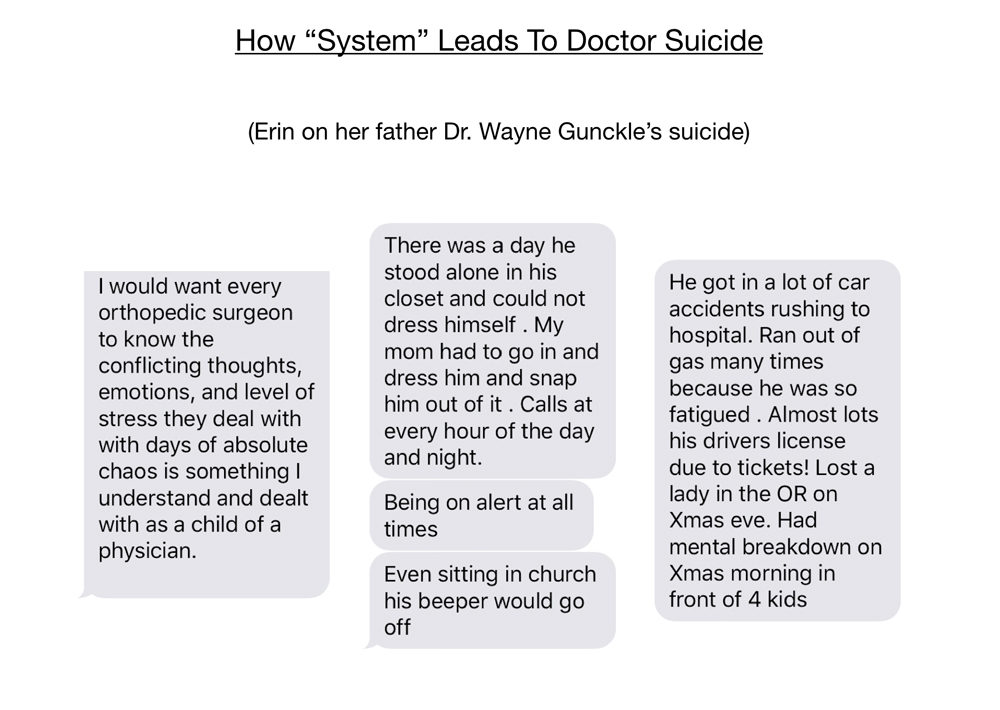
The “system” includes insurance hassles, hospital politics, and even the stresses of being a business owner or an employee (unique frustration with each). To elaborate, I’ll share a conversation I had with Erin Gunckle regarding her father Dr. Wayne Gunckle, an orthopaedic surgeon who died in 2011.
As his daughter reports: “It’s stressful getting the approval to do a damn surgery in the first place. If you don’t get it the patient may die. If you save them you may get sued. And if everything goes well the implant may be recalled. That’s what was going on when he died.”
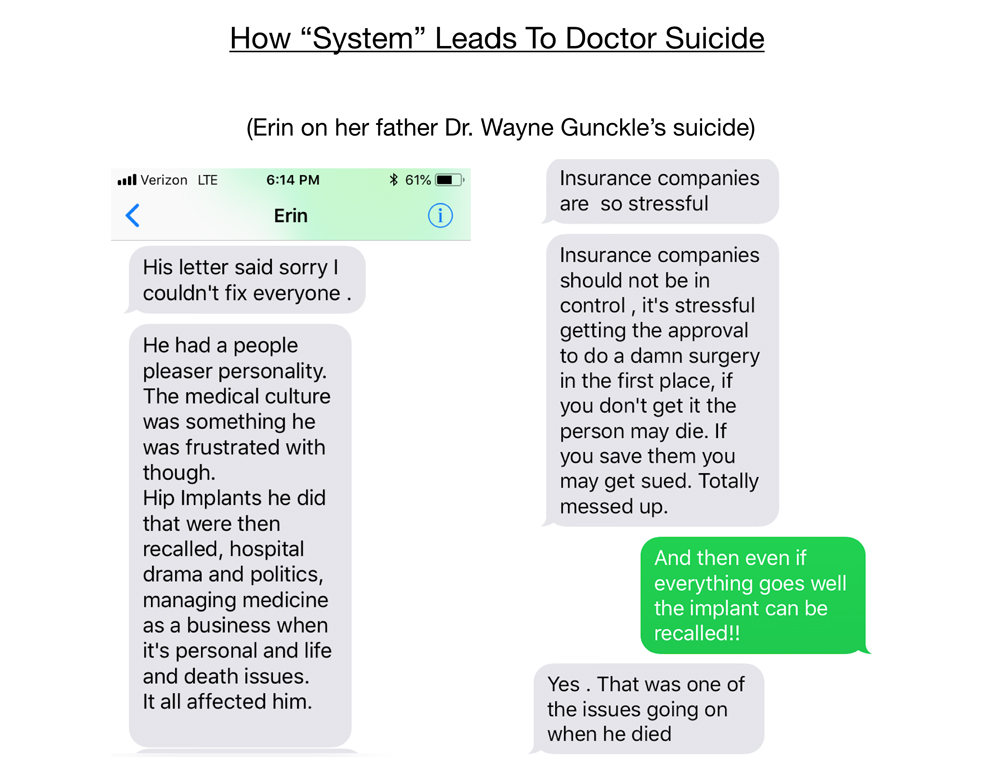
So on 3/27/2011, Wayne bought a rope on his way into the office Sunday morning. He had planned to finish dictating his charts before his suicide, but stopped abruptly and hung himself.
He left a suicide note: “I’m sorry I couldn’t fix everyone.”
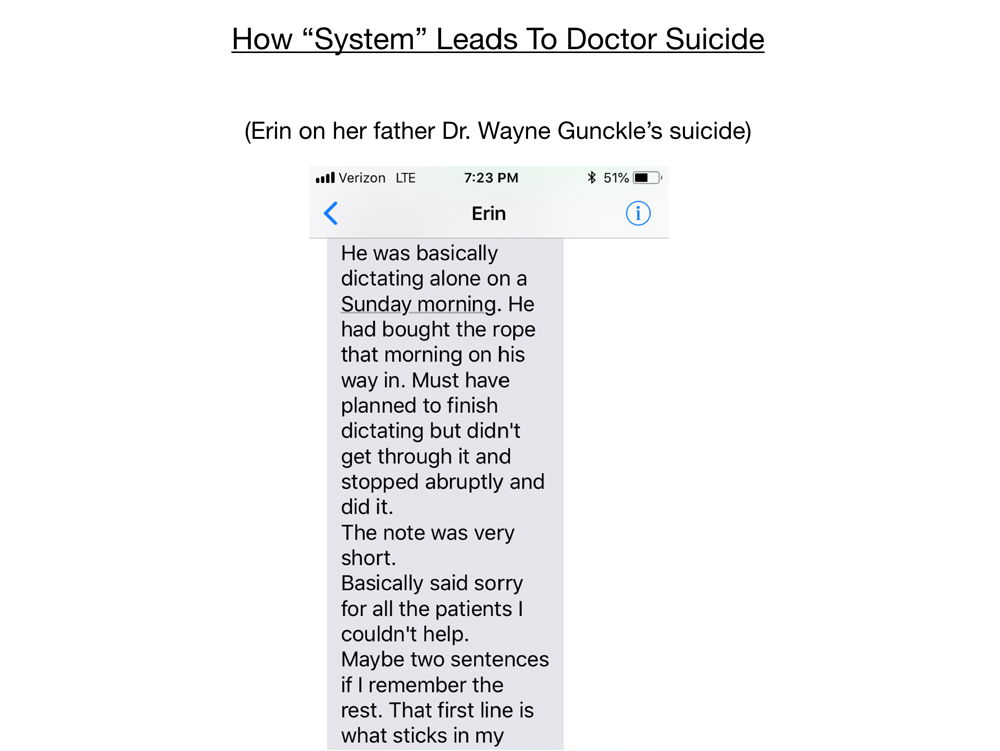
The lack of support and sheer overwhelm take an emotional toll on all of us over time. Erin writes: “There was a day when he stood alone in his closet and could not dress himself. My mom had to go in and dress him and snap him out of it. Being on alert at all times. Even sitting in church his beeper would go off. He got in a lot of car accidents rushing to the hospital. Ran out of gas many times because he was so fatigued. Almost lost his driver’s license due to tickets. Lost a lady in the OR on Christmas eve. Had a mental breakdown on Christmas morning in front of four kids.”
Continuing with the professional reasons for suicides: It’s not a surprise that orthopaedic surgeons would suffer from stress and isolation leading to overwhelm. Some then suffer from depression and even hostility. One felt pressured by family to pursue medicine and was in the wrong career. And the one that I recently investigated in my town died in part due to a grief reaction. In 1996 an iconic orthopedic surgeon died suddenly by cerebral aneurysm, weeks later his only partner died by suicide.
Mental illness tops the list of personal reasons. Six cases of either unrecognized (denial), untreated, poorly treated depression or bipolar. Sometimes doctors self-treat with alcohol, stimulants, and other illicit drugs eventually leading to paranoia and psychosis. Stigma prevents doctors from seeking treatment.
Marital issues, pending divorce, including a case of husband-wife suicide-homicide. Do you realize there is a Facebook group for wives of doctors in domestic violence relationships? The predictable end result of not being proactive in caring for these highly stressed individuals who fear seeking mental health help.
One surgeon with traumatic brain injury killed himself in front of his family.
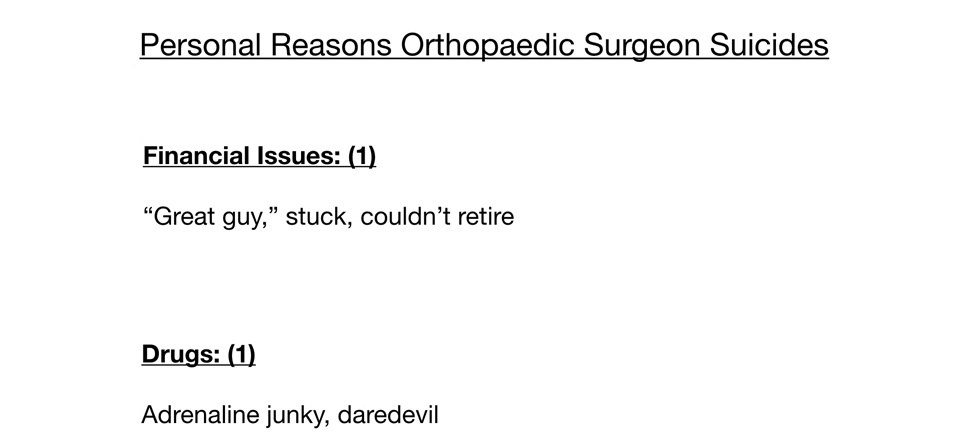
Additionally, one orthopaedic surgeon had financial issues, was unable to retire and felt trapped. Another had what appeared to be a drug problem.
Most are multifactorial. Professional success often leads to personal life atrophy. So it is challenging to isolate just one component as the central cause as many of these victims had chronic issues that were brewing and neglected for years. The good news is that gives us a lot more time to intervene to help prevent future suicides.
Most suicides are impulsive. I interviewed several male physicians who (against all odds) survived their suicides. I asked, “How long after you decided to die by suicide did you take the pills or slice your artery?” Answer: three to five minutes. Again, though the final decision took less than five minutes to carry out, the underlying issues that led to that decision to die by suicide had been present for years to decades.
The reason why most die by suicide is for emotional pain relief. In absence of support the only way they know in the moment to get out of the pain is suicide.
In conclusion, here are very simple no/low-cost solutions that can be adopted immediately to prevent suicides specifically among orthopaedic surgeons. You are more than your craft. Doctors are human. We require emotional support to thrive in medicine. The culture of medical education has too often pitted us against one another in an environment in which your success depends on crushing your competition. What if we interacted as human beings first? I invite you to embrace each other as brothers and sisters in medicine.
Even perfectionists make mistakes. The stakes are incredibly high and mistakes are inevitable when working on the mechanics of the human body. Expect (and train for) medical errors. Orthopaedic surgeons are taught like mechanics. Your personal and mental health needs may be least attended to compared with other specialties like family medicine.
Offer non-punitive support for bad outcomes and bad behaviors. First do no harm to yourself and your colleagues. Doctor means teacher. Use words that heal and above all do not injure other people. Often those who are injuring others have been injured themselves in medical training. As they say, “Hurt people hurt people.”Medical institutions should be safe spaces—free of bullying, sexual harassment, and public humiliation. A cycle of abuse involves perpetrators, victims, and witnesses. We can all actively stop this cycle in a way that helps everyone heal without losing any more lives.
Reach out. Take my challenge to get to know each other personally—not just professionally. Assume “happy” doctors are suffering silently. Create a buddy system—even informally. Pair up with a colleague and go to lunch once a week. Talk about more than sports, RVUs, and complex tibial plateau fractures (in less than 10 minutes!). Really talk (for maybe an hour) about how you are feeling—about your life. Know that there are counselors, therapists, psychiatrists who have practices dedicated to solely serving physicians and our special needs. (Yes, as a surgeon you are in a special needs group). Schedule regular sessions (even by Skype/phone, off-the-grid if necessary). You are not alone. You are welcome to contact me 24/7.
We need to talk about the tough things—fraud, corruption, and suicide. Support whistle blowers, depressed and suicidal physicians. Share your emotional struggles openly so that others feel safe to open up to you. Don’t just “go with the flow” and pretend like everything is okay. It’s not. We have the highest suicide rate of any profession. You can be a lifeline for those who are at the end of their rope.
Do No Harm—is an award-winning documentary by Emmy-winning filmmaker, Robyn Symon. A four-year project just completed this summer that honors nearly 100 doctors who have died by suicide including Ben Shaffer, Steve Ortiz, and Wayne Gunckle. Now screening at hospitals, medical schools and conferences. Attend NYC screening on September 12 & 13. Panel discussion to follow. I’ll be there and would love to see you. Grab your tickets here.

I’m open for questions. Download your free audiobook of Physician Suicide Letters—Answered. Most letters are from physicians on the edge debating whether to live or die. Most decided to stay on the planet with us. Most of these orthopaedic surgeons who died by suicide would have wanted to have a different ending. We have a lot to learn from them. Thank you.
Have you lost a doctor or medical student in your life to suicide? Please add their name to registry here.












This is all very sad. I am a retired UK clinical psychologist with 30 years NHS experience, not one of my 100’s of patients ever killed themselves. I saw patients with all manner of problems referred by their GPs. This meant that some of them asked me to treat their colleagues. We invariably had a few useful sessions. In UK Clinical Psychologists have peer supervision which gives them the opportunity to confide in a trusted colleague about all the difficulties encountered professionally, personally and at work. I think your recommendation to make these relationships is one of the most useful ones you make. I hope you have an opportunity to consult a colleague yourself.
That’s a great track record? Did you lose any physicians in the UK that you knew to suicide?
Reading this brought tears to my eyes. I’m the mother of Dr. Ortiz (talked about in the presentation). Oh, how I wish he had known of Dr. Wible and the help he could have gotten.
If any physicians, residents, med schools students or hospital personnel reading this article have a need for help due to stress, overwork, bullying, please seek help, it’s out there and it can start with Dr. Pamela Wible.
There are so many people who care but they can’t help if they don’t know about you!
Hi Gloria. This was just brought to my attention. I am the nurse he contacted before he left this earth. He was a great friend and physician and is truly missed every day even after all this time. So sad that we weren’t able to stop this from happening to him and so many others.
I was the nurse that Steve emailed before taking his life. His death was a devastating blow to our community. I am sad that he felt that was his only way out. We still talk about him a lot when we are working. I hate that this is such a big issue for people who dedicate their lives to helping others. He was a decimated and caring physician.
My father was a physician and took his life 40 years ago on Dec 7, 1978. If you want more information, don’t hesitate to contact me. Honestly did not read the whole article because it still is very painful, yet I would be more than willing to share details if it will help with research and provide more recommendations on how we can better support physicians so this stops.
It would absolutely help. Emailing you now.
Hi Pamela;
Thank you for all you are doing for physicians who have or are contemplating suicide.
I am one of these physicians and , because of this, left my medical practice 18 years ago.
I would like to speak with you about the issues . How do I contact you ?
CE Moon, MD
https://www.idealmedicalcare.org/contact/ Happy to talk . . .
Superb Work Pamela.
Congratulation!
I do not know anyone else doing something like this.
Labor of love for my brothers & sisters in medicine. I could have been one of my statistics. Thankful that I’m alive to bring my comrades back to life—at least in print & now in film. There is a “Wall of Remembrance” in the documentary with nearly 100 suicided doctors who are honored for their contributions to medicine (kind of like a Vietnam Memorial for doctors). View movie trailer here: http://donoharmfilm.com
Hello, I managed the trauma program. A general/vascular/trauma surgeon that I worked with in San Angelo, TX commited suicide in 2013 – Patrick Gibson, MD. There was another surgeon (his partner) that also committed suicide in ~2009. Thank you for addressing mental health crisis/issues in healthcare. I was hired to come in and revive their trauma program after his death and didn’t know until after I’d gotten there that he’d commit suicide. His name was 2009 David Saborio, MD. Shot himself in the head in a local park. Pat or “Gibby”, as we called him shot himself in the same way in the same park. When I learned this, I asked if they were investigating since two surgeons died that way both from the same toxic hospital which had numerous leadership turnovers. I know he also had a lot of professional pressure. He was the only general surgeon for a long time for this hospital. There was one other hospital in town. But San Angelo is hours from larger cities and higher levels of care. There had been 3 surgeons in his practice. The oldest one was primarily retired. Then Saborio commit suicide and left only Gibson. When I got there to work with them to get the trauma designation back for the hospital, it was a lot for him. The retired surgeon would take call one weekend a month or so to give him a break. Then that surgeon dropped dead of a heart attack. Gibby was there, they were all watching grandkids play a basketball game, gave him CPR until medics arrived but he didn’t make it, they pronounced him in ED. As soon as I got word the next morning I went and found him as he was coming out of the OR to give my condolences. I’ll never forget how he laid his head on my shoulder and cried. He said “my partners keep dying on me.” A few months later they hired a new surgeon who was fresh out of residency. We were able to get the trauma designation back, then I resigned shortly after that. From what I was told they struggled again to keep leadership for the program and keep the designation. Gibby also told me that the surgeon didn’t stay (her military husband was transferred) so he was alone again, I don’t know for how long. He was one of the few people I stayed in touch with after leaving there. The last time I spoke with him, he was celebrating the birth of a new grand baby. I’m still heart broken over him being gone.
Wow. I’m seeing there are clusters now in certain hospitals and residencies. Just reading the last few comments. Two in the same park? We actually had more than one doc die in the same park too. Similar locations to the point where the medical society director was concerned that it was a hot spot for doc suicides. Unreal.
Will send you Pat Gibson’s obituary. It includes a lot of details but suicide is not mentioned.
3 Residents within the U of M residency programs have committed suicide in the last 3 months. Where is the outrage at the medical training system!? Demand answers from the people in charge of these programs. MN Daily found it pertinent to run an article on a study which showed a possible increase in suicidal thoughts within the LGBT acne community in 2017, thats right, the LGBT acne community. But when residents are killing themselves right under your noses you are silent! Demand answers and actual change, offering counselors and forums as a solution is comically deficient in addressing the real systematic problem. Residents and medical students are put under immense pressure and at any point in their pursuit they can be cut off due to any number of reasons (test scores, poor performance, health reasons). Demanding perfection of people for a decade is an unreasonable expectation. The university needs to offer exceptional resources and they need to let the residents know, no matter what happens the university has their back and will support them through tough times. Hiding physician suicides is common and an outrage. Mn daily needs to do their part in exposing the broken medical training system that demands too much from people and the consequences are dire!
Systemic issue and occupationally-induced especially with 3 in one hospital in 3 months! Root cause analysis points to medical education human rights violations of our doctors-in-training. Are these in the same residency program? Complex situation and many programs far worse than others. Thank you for speaking up. I’m heartbroken. Please send me the names as I want to make sure they are represented on the registry.
We need to go back to a balance of life and work that we used to have in the 1950s and 1960s before HMOs and business leaders took over the medical field.
Why are we not charging the CEOs, their fellow doctors and nurses with murder who cause these doctors’ deaths because they were bullying these doctors and creating slavery-like working conditions?
Thank you for bringing this to light, all you do, & being of service in this way. I am in the military part time and a wonderful physician colleague (family doc) and of course the happiest and sweetest man you’d ever meet also in the military, who treated everyone has an equal, but later found out had deep struggles with marriage and balancing his commitments and he committed suicide by hanging 2/4/17. From my own experience, it’s a challenge for those who want to be physicians or other medical providers as it’s a calling and devotion to your patients and others who don’t have that same drive& devotion to be healers like perhaps spouses or partners, they often times in their desire for a more balanced home life put further undue pressures and criticality on their spouse physicians, as not only there’s daily long hours but throw in deployments. (It’s a double ‘being of service’ whammy) that really beats up a stable home life. I would imagine military physicians are up there on suicides (and/or going ballistic overseas). Again, keep up the amazing work and I hope to attend a retreat to get my own biz off the ground doing what I love!
I want to make sure he’s on the registry. I’ll email you. So very sorry Diana. Military docs get kinds of a double whammy.
What an astonishing and astonishing sad and tragic presentation Pamela.
So glad that you are bringing this out into the open.
We’ve been in touch before and as you know I was a boots on the ground suicide specializing psychiatrist for many years, mentored by Dr. Edwin Shneidman, a pioneer in the study of suicide.
Here is a link to an infographic called the Road Back from Hell that I have been using with vets and active military. It has helped them by giving them a vocabulary to express what they feel, the doing of which seems to help.
Something that I am discovering with military that perhaps some of your doctors who are depressed and feeling suicidal might relate to is feeling not in control = feeling out of control and following that, the next step is feeling they will literally fall apart and shatter and never come back and always be a burden.
So at that point they kill themselves to avoid that.
BTW this is also the point where many vets are looking down the barrel of a gun and discover God. In a number of cases they are able to “surrender” to God and that allows them to short circuit or bypass the “not in control –> out of control” beginning of the death spiral.
And then something paradoxical happens. Instead of coming apart, they let go of control, lean into their faith, cry with relief and then slowly begin to come back to their senses.
You’ll get a sense of how faith can rescue people if you read the transcript of Brian Dawkins NFL Hall of Fame induction speech.
I believe that if we have groups of physicians sharing their feelings along the Road Back from Hell journey as vets are doing, this can help them get their feelings out, lessen the isolation (where you’re more prey to your imagination) and they will be able to lean into the shared humanity and vulnerability they are all feeling.
I’m also listing an article I wrote as my website entitled: Why people kill themselves. It’s not depression.
God bless you for this work Pamela.
Should be “astonishingly sad”
Doctor just told me: “I know of several colleagues. A plastic surgeon. A neuro-ophthalmologist, A Gynecologist. A Medical student + Several ” could be’s ”
For those who want to submit names to confidential registry please include: For registry I collect specialty, age at death, date of death, location, and any other circumstances you
wish to share (which I shall keep confidential).
One thing I would like to know from the physicians who considered suicide and did not follow through: What kept you alive? What kept you going? Perhaps this will give the rest of us clues as to how we can reach out and prevent further losses.
For myself I can say that I was in bed 6 weeks praying to die in my sleep and not wake up in the morning. I felt like I was in a depressive coma or something. What kept me alive is 1) I’m not a violent person (so no gun and no desire to do anything violent – overdose would have been my method for sure) 2) I was SO depressed I couldn’t even think straight to plan anything so what kept me alive is that it is very uncommon for a healthy vegetarian woman to die in her sleep at age 36.
As for others, I have heard it’s their kids that keep them going. One told me it was the dog. Feeling like you had someone depending on you kept some going. Download free audiobook (Physician Suicide Letters—Answered) as 53 docs share their feelings and reasoning for dying or staying when on the edge.
I was at a very low point in medical school, having requested a second non-consecutive year leave of absence, which the main Dean of the school responded to by advising the promotions committee to ask me to withdraw (a euphemism for being kicked out).
The Dean of Students, who to this day I believe was an angel sent to earth to save my life, delivered the bad news to me and before I descended further towards suicide, he stepped in, saw value and a future for me – that I didn’t see – based on some ability to care he saw in me that wasn’t graded in med school and then took on the medical school and its Dean to appeal their decision at his own expense.
When an angel steps into your life and saves it, you’re never the same again, but it compels you to pay it forward which is why I became a suicide specialist who intervened with people as he did with me, rather than studying it as an academic. That explains my challenges in getting through to the medical establishment with my non-evidence based approaches.
Pamela, once again you continue to amaze me! You so eloquently deliver sensitively an uncomfortable topic that needs to be discussed in medicine today. Since knowing you, I now see physicians in a new light and realize all the pressures they have endured to continue caring for their patients. It is time for the healthcare system and medical administration culture to change from demanding more from physicians and instead provide the support these healers need to heal their patients and themselves. Thank you for your passion and dedication.
Im sure you were made aware of this Canadian Medical student who did not match to a residency program 2 years in a row. Debt, shame and societal pressure ultimately led him to take his own life.
Robert Chu MD
Yes. He is on the registry. I’ve spoken to his father. His photo is actually up in my house and he is going to be featured in the forthcoming film. Please view trailer here and come on out to a screening this fall: http://donoharmfilm.com
Matt Levin, MD here in Western PA
We’ve talked a couple of times and I gave “testimonial” about your first book the Goats, etc.
Sorry can’t get away midweek for your NYC present but look forward to your future work.
As a solo for 15 years, and treating several physicians for GAD, etc, I am pleased to see you making progress.
I am sure you are aware of the academic work on “burnout” a Stanford group is doing, as you were quoted in the Medscape article.
I would be pleased to be an “east coast resource” for suicide outreach if I can help.
Please let me know through email if I can be of further assistance.
Like you I am solo, and I like it that way….
Take care,
Dr Matthew Levin
I won’t put an email down here as medical needs should go through the office.
PS Yes I lost a professional friend to suicide by GSW; the “system” still has his name on the sign in front of the building I pass almost every day – it’s been 3 years now.
“very enlightening article. i am an orthopedic surgeon as well from the philippines. just like to share but i dont want my name or email written in the comment section. i have thought about these things too. like wishing the plane im on to crash or drive my car off the cliff. the worst is i see or imagine myself sitting on the bed with the gun in my mouth. medical practice is tough in my place. i can work 24/7 without complaint. if it is just the bulk of surgery as long as the materials are provided. the thing is that due to lack of manpower and resources, patient care and surgery is delayed which puts the patient at high risk for complications and us doctors for liabilities and public shaming. added factors are: i live alone in that workplace away from my family which i only get to see once a month (if i get lucky) or once in 3months. it has been 10 years that i havent spent christmas holidays with my family as i was always on duty for those days. we always postpone christmas and new year. my workplace is 380km away from our home. there were even times that i feel numb towards my patients…. at the back of my mind “there must be something more to life than this… i cant keep going on like this…” i felt trapped in a loop. eventually, i resigned. now im doing fellowship and feeling better. as to what comes next, still uncertain….”
have a few thoughts about anesthesiologist: first, they have ready access to lethal drugs and are skilled enough to be successful. Second, their workday is a lot like an air traffic controller’s, busy at the beginning and end of a case and mostly boring on the middle but they can’t leave their seat, then occasional episodes of pure terror. Third, they get blamed by the more glamorous and better paid (?) surgeons a lot. Time everyday to ruminate on and obsess over perceived failures. Also their schedules are completely tied to the surgeons’ schedules.The ones I know are also extra sensitive to pt pain and pain management lives in anesthesia in my institution, and they seem to feel patients’ pain more than other surgical people.
Have you noted any pattern at certain institutions? I started residency in California. I ended up at Mt. Sinai in NYC. It was like night and day. While my previous program was supportive and nurturimg during one of the hardest parts or our careers—sinai was horrible. The environment is so cold and harsh and cut throat. It was so bad that a number of the cheif residents had to be talked in to going to the graduation so the dept wouldn’t look bad. I found out why when i myself felt humiliated when I graduated and the dinner celebration where my family and friends had come across the country for graduation only to have a gruesome “roast” of the cheifs. Residents are routinely criticized and not supported and subtly encouraged to lie about our work hours. I was actually not surprised to hear of a couple of suicides out of Sinai a couple years ago. I was warned it was a “malignant” program and it was. Having had the benefit of a non malignant program i had already had my confidence built up and supported and i knew that was not normal or right- unfortunately most of the other residents had no comparison – so accepted that as normal. I’ve never said anything about this so please do not share my name—but keep an eye on malignant programs that push stressed residents over the edge.
They don’t mention, as a cause, doctors who are falsely accused of things for either Religious reasons (abortion providers being set up by zealous Catholic prosecutors and Heads of OPMC’s), rejecting sexual advances by very mentally ill patients, etc. who later falsely accuse them. The observations seem to focus on the doctors’ personal internal crises and the only mention of external forces relates to Malpractice suits and the stress that causes, or personal home problems. The focus seems to be on the doctor and not really on societal pressures. I spent 2 months in Lawrence, Kansas working with Dr. Richard Irons, author of “The Wounded Healer” and his staff who had over 25 years experience with this issue. Their insight would add greatly to this article.
An hour certainly is not enough time to dive into the magnitude of data I’ve collected and insights gleaned from speaking to thousands of doctors—many injured by the “system” and blamed/shamed in ways that are completely disabling. Sadly. many of us are set up to fail in part due to an artificial cap on the number of physicians leading to shortages (creating a ton of stress on those who remain) and lack of compassionate leadership at our medical institutions that often seem more interested in short-term profit than in the health of their physicians.
I dont think of suicide but I am very depressed. I dont talk about it with anyone, not even my husband because I need to be strong for my family. There are days I feel I am in the wrong profession. There are days I think I dont want to be a doctor anymore. I dont have enough time for my family especially my daughter. I feel like I missed so many things in life because I have dedicated my life to medicine. I try to be strong everyday and face my struggles day by day and try to be happy despite of.
Call me: 541-345-2437 or send a confidential email here and I’ll call you back: https://www.idealmedicalcare.org/contact/
Funny question submitted by a doc:
“Pamela, I was very touched by this piece regarding the orthopaedic surgeon suicides, namely the stories of the two surgeons that you depicted. From looking at the figures breaking down the numbers it appears to me a staggering number of these cases are male. Being a guy who was a star football player tough guy type who is now in medicine (the common sterotype of most Orthos), I am wondering what the best way to get through to them would be? You are undoubtedly the leader and a true hero in this field, but you are what can be conceived as the opposite of the ortho stereotype, a west coast maternal type (no offense intended : ) ). Do these macho guys have a hero in the mental health / physician suicide struggle that looks and talks like them? There was recently a piece on ESPN.com about some prominent NBA players who have been struggling with mental health issues and how few of them talk about it because of the stigma associated with it. A few have come forward however and led the charge, showing that men can be vulnerable and theres nothing wrong with it. These are the people that orthos treat and the tough guys that men look to most often as heroes growing up. If you have an example of a male ‘Pamela equivalent’ that is as passionate about the subject as you are, please let me know, I’m very curious. Thanks again for what you do, you undoubtedly are saving lives every day.”
My response:
“I am happy to help any group of men find the guys among them who can be leaders in this area and facilitate a group that will create culture change in any institution. What I would suggest is a panel discussion (which I like to do after keynotes) in which men will step forward and start to share among each other their struggles and successes within the realm of mental health. I have an example on YouTube – a spontaneous moment during a keynote that demonstrates how your solution is already in the room: Medical school dean talks about losing student to suicide. No need to bring in a Pamela-esque guy from out of town (I don’t really know of any guys like me :). You can harness the champions among you in your organization. . . a west coast maternal type (no offense intended : ) – love it!”
Hi I’m a general surgeon, practicing in Cebu, Philippines. Doctor suicide is rare in the Philippines. I would like to know how we can help… perhaps by comparing.
How to help:
1) Collect data in your country—examine every physician death—especially among younger doctors (and male anesthesiologists)
2) Perform psychological autopsies on all suicides.
3) Show the film in your country at hospitals, clinics, medical schools: http://donoharmfilm.com
Begin the conversation about doctor mental health. Thank you Shawn!
Reading this both angered me and left me with an unknown salty discharge. Thank you for sharing what has been a sobering read.
Salty discharge is part of the solution. And anger is an excellent fuel for action.
At once saddening and surprising because suicides among doctors in my India is nearly unheard of.
Actually more common in India than it may appear.
Do you know anything about the motives for the suicide of Dr. Dean Lorich? Thank you.
Nothing I can discuss publicly at this point. You can read the media. Lots of “theories” out there.
Dr. Wible: I am Dr. Dean Gerard Lorich’s wife. Nobody speaking out about my husband and the father of our three beautiful daughters has tried to contact me since his death.
Alternatively, how might I find you?
Deborah
I’m so glad you reached out. I didn’t know how to reach you and will email you right now. You can always contact me here and I will get back pretty quickly: https://www.idealmedicalcare.org/contact/
Your husband was much beloved by this group of orthopaedic surgeons and they really wanted to dedicate my keynote to him.
Ms Lorich:
I was one of Dean’s first residents at Jacobi, on the very first day that he began… I was a senior resident at the time. I had occasionally contacted him over the years with clinical questions as well. My deepest condolences on his passing. The entire orthopaedic community is diminished by his absence.
Jim McL.
Dear Dr. Wible:
Your presentation at the 19th Chicago Orthopedic Trauma Symposium was excellent. This is a follow up to the last audience response question after your talk. There is a body of literature that implicates the drugs used to treat mental health disorders may be causing more harm than appreciated. Since you are on the forefront of the suicide epidemic perhaps you will find this information relevant. The book
“Anatomy of an Epidemic: Magic bullets, psychiatric drugs, and the astonishing rise of mental illness in America” (2010, Broadway Paperbacks)as well as Mad In America shed more light on this crisis.
Dear Paul,
This week on Mad in America, Martin Plöderl and Michael Hengartner discuss their recent research investigating the association between drug prescriptions for mood disorders and the suicide attempt rate among adolescents. Noting that their findings are in line with those from randomized controlled trials, they write: “Put together, these data strongly suggest that antidepressants can cause suicides and aggressive behavior,” despite mainstream psychiatry’s continued claims that these drugs reduce suicide risk.
Also in blogs this week, Helen Spandler reflects on what she has learned from working alongside psychiatric survivors for 30 years, writing that it has been “profoundly unsettling and challenging, but ultimately rewarding.” Patrick Landman examines “the psychoanalytic struggle against the DSM” over the past 40 years, and Eric Coates shares memories of a friend who had taken her life, writing that “the things that conspire to drive a person over the edge are too numerous and varied ever to point and say, it was this one.” And in this week’s personal story, Michelle Llamas shares her struggles with severe panic attacks and how a book she had dismissed as “self-help quackery” later showed her alternative methods of treating her problems.
In research news, we report on a new Journal of Mental Health article questioning the ethics and effectiveness of mental health services. We also take a look at the connection between education level and prescription drug misuse in young adults, how publication biases inflate the perceived efficacy of depression treatments, how peer support reduces chances of psychiatric readmission, and how prenatal exposure to SSRIs alters fetal neurodevelopment. And on our podcast, we speak with Sami Timimi, Peter Gordon and Stevie Lewis about their formal request to remove a UK Royal College of Psychiatrists representative from Public Health England’s review of prescribed drug dependence, due to his financial ties to the pharmaceutical industry.
As always, we welcome you to follow and join in on these critical conversations, and many others, through our news features and blogs.
Until next week,
Emmeline Mead, Managing Editor
Great article Pamela, I’m always scared when I see your posts because they’re so heartwrenching. But I think two things wee need to address. And they should start in medical school. Counseling students on how achieve work-life balance and how to maintain their relationships and marriages.
No other professions demands time away from family as much as doctors. Hospitals needs to ensure, they’re staffed well enough so that doctors are working shifts like everyone else and no not just simply filing forms about hours. They need to be grounded with their families. I think marriage breakdowns are a major source of pain and strife.
Absolutely. Given that some surgery programs used to BRAG about 100% divorce rates among their residents, I think this is a great idea! BTW, med students CHOSE those programs bc they thought they’d get better training there!!!!
My father was a physician. He did not directly commit suicide although I expected it. He did stop taking BP lowering meds… which probably contributed to an earlier onset of dementia… which did become a major factor in his death. One of his brothers did “actively” commit suicide. My sister is a practicing Midwife… and shared on FB your report with a comment that she identifies with one of the examples… I also would have to honestly “keep my hand raised”…
I’m grateful someone is even thinking about this…I just completed an orientation at a large, prestigious hospital and there was no mention of physician burn out or depression/suicide, just the usual about caring for the patient first etc. I’m concerned about the workload on the floors, there’s a maximum number of patients a nurse can have for safety reasons, yet no max for physicians…same old same old… Thanks for caring.
Michael Brown was a nutcase. Why include him with the others? I’m from Houston and his mental/drug issues were well known. It would have been there no matter what his profession was. Putting him alongside respectable doctors is a disgrace.
I realize the extent of his situation and untreated severe mental health condition. My registry reflects ALL doctor suicides—including homicide/suicides and others. As with all people and professions there are some who are more disturbed than others.
I mentioned to my psychiatrist who was treating me for depression and P.T.S.D. (who was also vetted to me as THE psychiatrist in my state to be seen by for physicians) that I was not suicidal any longer but that I was surprised that after three prior years of nearly daily SI that I had not acted on it. Within 24 hrs this psychiatrist without further evaluation recommended to the board that I no longer be allowed to see patients and I was ordered to cease practice. No transition period for my patients nor any possibility to find appropriate care for their follow up. I was told to give them a list of possible providers and that I was not allowed to explain to them any circumstances simply that I could no longer see them. I remain horrified and hesitant to consider returning to practice despite horrendous need in an underserved area.
Dr Ortiz was a wonderful surgeon and well liked in the community. Heard him speak at hospital marketing dinner lecture several years before his demise. Such a loss–unfortunate outcome for a wonderful surgeon.
Interesting, but being a surgeon myself I talk about there being one more layer of the cause.i.e. Stress and depression are reactive, not causative in these situations. Having worked in 4 countries(so far) there are national, cultural differences but the end-results rare the same. It is too easy to put it down to gender/race based discrimination or even perfectionism. Being surgeons describes us completely, as surgery is our vocation, our true calling. For starters, I would suggest dropping the P from PTSD. Interested in exploring this further? So far, I have been turned away from all doors I’ve knocked on, just to get those who should take notice to listen
Thank You for sharing this. I got chills reading the article. It further reinforces the fact that violence, suicide & mental illness are related and in many cases preventable, if we were to examine root causes,and explore systems-wide/community-wide strategies.
I am curious…did any of the ‘near miss’ doctors mention a history of Childhood Sexual Abuse or any other ACEs?
If you’re looking for excellent resources on prevention, see The Prevention Institute & Berkley Media Studies. BMSG just released a Guide on Sexual Abuse Prevention… I have found that the suggested strategies are relevant across health issues.
Thank you again for bringing this to light.
All the Best.
This is a very good research blog. I want to tell you how much I appreciated your clearly written and thought-provoking article.
I’ve followed you throughout the years and like how your presentations have become more data-driven (or “evidence-based”). Of course, I wish you didn’t have any data to work with, but I digress.
As a general pediatrician with a history of major depression, ADHD, and anxiety, here are 3 things that thus far, seem to work for me:
1) I DISCLOSE my diagnosis to my patients, within context, of course. By “patients”, I mean parents.
2) I ask MY patients to support ME. Sometimes, we need to forget the B.S. that patients cannot be our friends.
3) I try to have a hobby and share it with others as much as I can.
#3 is obvious. Talk to me about something I like and it’s like a mini-vacation. In the future, I’ll work on some sort of calendar so patients know there’s an event related to my hobby. There was an article in The New Yorker (I forgot now) that argued the opposite of addiction is not sobriety, but human connection.
I disclose my diagnosis freely and gladly, again within the context of the encounter. Before, I was terrified of doing so (and still am, but do it anyway). The usual stresses of daily practice – finishing notes, patient care, going beyond to have a patient receive the care they need – can drive sane people crazy. We’re gonna fail because we’re not perfect. We do NOT understand that. But patients and parents DO. Especially when discussing mental health in children, the stress of parenthood, and usual “adult problems”.
The “cheerful doctor” acts this way because he/she needs to. Alcohol and drugs are a lot easier but much less creative. A teenager once asked, point-blank, if I ever thought about killing myself. I said: “No! I love food way too much!!” Which was my actual response to a previous program director who only viewed depression as a one-way street: unless I was suicidal, I should not bother anyone. It was a sign of weakness. Now, I ask for a hug after almost every encounter and I tend to receive at least 1, usually from the parent! This started one day simply because I truly needed a hug. I was giving some personal advice to the mom (well-known to me) of a beautiful, perfect baby. She lost her 1st child in devastating fashion from a heart defect. She needed a hug too, and from that day on, my personal RVU formula includes earning a hug from at least 75% of my patients. Most days, it’s usually 60%, but the ones I don’t get now, I’ll get later.
Don’t smoke, barely drink, and am scared to death of benzos. I use them sparingly (once a week) and only by the insistence of my psychiatrist. Though I’ve always been friendly, asking for help, much less affection, is something foreign.
My wife is amazing. She trained as a healthcare professional and currently stays at home with the children (a full-time job of its own). However, she still doesn’t understand why my depression and ADHD have not been “fixed” with medications, or why some nights I simply can’t sleep well. She does help me greatly, but we’re wired differently. My pre-teenage child knows I have depression, but we’ve never formally talked about it. Perhaps it’s time we did. It’s the bad thing about reaching out for help – if I fall, they’ll view it as their fault. A burden most of us do not want to pass on to our family. Which is the reason I tell my patients… so that burden is now shared.
You want me to write a letter to your insurance, another to your child’s school, and one to your employer, while working on prior authorizations? No problem – but I demand a hug or some outward form of encouragement to keep me going! It doesn’t have to be physical, but my empathy is not unlimited and as a salaried physician, get paid the same for every patient. These interactions almost always happen in the hallway, partly to avoid any “appearance” problems, partly to teach parents and patients “this is the way medicine is suppossed to be practiced”.
Also, thank you for mentioning that physicians can and do have children with health problems. One of my children is autistic… while the child has made FANTASTIC progress over the past 3 years, the thought that my child will not have a “regular” adulthood is a source of constant anguish. As I tell my patients: my child simply needs more help… but then again, which child doesn’t?
Ironically, I do NOT disclose my depression, ADHD, or anxiety to my physician colleagues. Hospitals may be callous, and health insurance companies are greedy, but it’s my physician collegues that will chit-chat among themselves, or send “anonymous concerns” to a superior. Our “public persona” may be “tell someone if you’re depressed, get help!” but physicians will be the first ones to not trust each other and refer to a committee or a medical board. Perhaps I’m a loner, but that’s been my experience.
The way I see it – I can certainly lend a hand to any of my personal physician friends. We do need to heal ourselves, but if patients want an empathetic physician that’s always available, they need to keep me healthy too.
“I DISCLOSE my diagnosis to my patients. I do NOT disclose my depression, ADHD, or anxiety to my physician colleagues.”
That really says it all. We have been pitted against one another and infighting among victims only perpetuates the stigma and isolation. We are brothers and sisters in medicine. We should be each others’ biggest cheerleaders.
I’ve followed you throughout the years and like how your presentations have become more data-driven (or “evidence-based”). Of course, I wish you didn’t have any data to work with, but I digress.
As a general pediatrician with a history of major depression, ADHD, and anxiety, here are 3 things that thus far, seem to work for me:
1) I DISCLOSE my diagnosis to my patients, within context, of course. By “patients”, I mean parents.
2) I ask MY patients to support ME. Sometimes, we need to forget the B.S. that patients cannot be our friends.
3) I try to have a hobby and share it with others as much as I can.
#3 is obvious. Talk to me about something I like and it’s like a mini-vacation. In the future, I’ll work on some sort of calendar so patients know there’s an event related to my hobby. There was an article in The New Yorker (I forgot now) that argued the opposite of addiction is not sobriety, but human connection.
I disclose my diagnosis freely and gladly, again within the context of the encounter. Before, I was terrified of doing so (and still am, but do it anyway). The usual stresses of daily practice – finishing notes, patient care, going beyond to have a patient receive the care they need – can drive sane people crazy. We’re gonna fail because we’re not perfect. We do NOT understand that. But patients and parents DO. Especially when discussing mental health in children, the stress of parenthood, and usual “adult problems”.
The “cheerful doctor” acts this way because he/she needs to. Alcohol and drugs are a lot easier but much less creative. A teenager once asked, point-blank, if I ever thought about killing myself. I said: “No! I love food way too much!!” Which was my actual response to a previous program director who only viewed depression as a one-way street: unless I was suicidal, I should not bother anyone. It was a sign of weakness. Now, I ask for a hug after almost every encounter and I tend to receive at least 1, usually from the parent! This started one day simply because I truly needed a hug. I was giving some personal advice to the mom (well-known to me) of a beautiful, perfect baby. She lost her 1st child in devastating fashion from a heart defect. She needed a hug too, and from that day on, my personal RVU formula includes earning a hug from at least 75% of my patients. Most days, it’s usually 60%, but the ones I don’t get now, I’ll get later.
Don’t smoke, barely drink, and am scared to death of benzos. I use them sparingly (once a week) and only by the insistence of my psychiatrist. Though I’ve always been friendly, asking for help, much less affection, is something foreign.
My wife is amazing. She trained as a healthcare professional and currently stays at home with the children (a full-time job of its own). However, she still doesn’t understand why my depression and ADHD have not been “fixed” with medications, or why some nights I simply can’t sleep well. She does help me greatly, but we’re wired differently. My pre-teenage child knows I have depression, but we’ve never formally talked about it. Perhaps it’s time we did. It’s the bad thing about reaching out for help – if I fall, they’ll view it as their fault. A burden most of us do not want to pass on to our family. Which is the reason I tell my patients… so that burden is now shared.
You want me to write a letter to your insurance, another to your child’s school, and one to your employer, while working on prior authorizations? No problem – but I demand a hug or some outward form of encouragement to keep me going! It doesn’t have to be physical, but my empathy is not unlimited and as a salaried physician, get paid the same for every patient. These interactions almost always happen in the hallway, partly to avoid any “appearance” problems, partly to teach parents and patients “this is the way medicine is suppossed to be practiced”.
Also, thank you for mentioning that physicians can and do have children with health problems. One of my children is autistic… while the child has made FANTASTIC progress over the past 3 years, the thought that my child will not have a “regular” adulthood is a source of constant anguish. As I tell my patients: my child simply needs more help… but then again, which child doesn’t?
Ironically, I do NOT disclose my depression, ADHD, or anxiety to my physician colleagues. Hospitals may be callous, and health insurance companies are greedy, but it’s my physician collegues that will chit-chat among themselves, or send “anonymous concerns” to a superior. Our “public persona” may be “tell someone if you’re depressed, get help!” but physicians will be the first ones to not trust each other and refer to a committee or a medical board. Perhaps I’m a loner, but that’s been my experience.
The way I see it – I can certainly lend a hand to any of my personal physician friends. We do need to heal ourselves, but if patients want an empathetic physician that’s always available, they need to keep me healthy too.
I committed to the medicine path as an undergrad at a competitive state school. Biology program extremely competitive, even though not ivy-league. I volunteered with the hospital, and saw first-hand how harsh the physician life could be through the incessant complaining of the patients. I got a job acting as patient simulator (and helping out with the grading) for the MD and PA programs. In the process, I got a job at the University Hospital working in pathology, doing assay development-DNA analysis. It really changed my course. I switched to research, completed a master’s in molecular pathology, took some business classes, and here I am in biotech.
Why does this story matter? I knew that I didn’t have the emotional wherewithal to handle direct patient interactions-when things went wrong. I was a massive perfectionist. At least I only risked molecules, not people. Maybe I would have done fine as an MD. But, we should all be fully aware of the occupational risks and check ourselves honestly to see if we are emotionally equipped. Maybe the word needs to be spread how hard it really is to practice medicine, and change is needed as well.
My father was a therapist (social worker) and I feel that the exposure to all the trauma basically took away his will to live. He worked on suicide prevention, at-risk population issues, gender issues, marriage and sex therapy… He didn’t kill himself, but did seem to !consciously! let himself go–to diabetes. Didn’t take it seriously at all, almost like he wanted it to ravage him. It’s like reliving all his patients’ traumas made him loose his faith in humanity and he just wanted the pain to end. Gosh, we really need to help those on the front lines.
Anyone working with humans directly trying to heal them and alleviate pain and suffering. Kudos to all of you. God bless you and let’s hold hands and get through this together.
Cameron – EXCELLENT that you assessed the working conditions in medicine first hand and made a personal evaluation of your emotional resources to handle this type of grueling though fulfilling work. Thank you for your wisdom!
I truly believe that the state of healthcare in America is in a crisis. It is unfortunate that it is likely that many more physicians will commit suicide. I have practiced orthopedics for many many years and am able to conclude with CONFIDENCE that the system does NOT care. Our freedoms as basic citizens have been usurped as means for continuing to reduce costs. We operate under the sword of FEAR. If an administrative body or patient does NOT end your career, your colleague will. We are vehemently punished for providing care, not because we harm patients, but because someone else bears the costs of our services. Free Speech will be the downfall of the American surgeon, as one may say or allege ANYTHING because it is only the physician’s reputation that is at risk.
Have you seen the reports om CEO apparently infecting surgical sites to discredit orthopaedic surgeon . . .
I would absolutely agree that the state of healthcare is in crisis and often things need to get worse before they get better. Physicians should use free speech to stand up for one another and speak out about the human rights violations in medicine. Sadly doctors have been divided and conquered through fear-driven medical training that glorifies self-abuse and neglect so we have been easy to control. Not anymore. Doctors are now standing up for their rights in greater numbers.
CEO apparently infecting surgical sites to discredit orthopaedic surgeon.
dr wibel why mot tell rhe truth about benzodiazapines ? phsyche drugs and akathisia – when u know ? anxiolitics means xanaz ativan valium or klnonopin a then prozac an ssri and seroquel(an an anti phsychotic?) for sleep no less…. this man was posioned plain and simple he could bave alreadt had akathisia to lessor degree with smaller windows of relief from his benzo. The poly phamrmacy may well have turned it acute is my uneducated guess. Pam you know the truths about these meds they are all too quickly prescribed and frequent poly pharm at too high a dose dor too long
There is certainly a huge issue with his benzo withdrawal. That is one of the many concerns I have about these suicides. Choosing to medicate people (or suddenly un-medicate or switch and double med doses) rather than solve some of the underlying issues can be deadly for sure.
I am sure this blog will definitely helps to orthepaedic surgeons and yea i agreed the important things that you have mentioned above, impact on surgeons lifes..
Such glowing comments on Shaffer just because of a job. Was good at insults. Was opposite of nice to me.
On April 13, as fate would have it, Dr. Shaffer’s name came up in a conversation 25 years after I lost touch with him. I was so saddened when a google search revealed that he died in 2015 and stunned when I found this keynote revealing the cause as suicide.
I thank God I was fortunate enough to be his patient. After 5 years and 12 doctors, my severe hip pain remained undiagnosed and with no apparent cause. At 33, I was unable to sleep more than 2 hours, heavily medicated for pain, used a cane to walk and, at times, needed a wheel chair. I was eventually referred to Ben Shaffer. He was kind and caring and smart…he diagnosed my rare hip condition leading to a cure and a comfortable future. I am so sorry to read about his struggles and will be forever grateful that he managed to touch patients throughout his life and in spite of those struggles.
I have read this entire keynote and all related posts with great interest and great concern. I was unfamiliar with this issue and was able to share this new knowledge with my son who is finishing his second year of med school. Thank you Dr. Wible for your work and thank you, once again, to Dr. Shaffer for leading me to this information.
Perhaps you can see that I could not let the April 12 post by Anonymous be the last word on Ben Shaffer. Like all of us, I am sure he was not a perfect man. But he will always be a hero to me. Thank you, Doctor, peace be with you.
Please also see this article from the perspective of a patient who lost her orthopedist: https://www.idealmedicalcare.org/susan-lost-her-doctor-to-suicide-she-wants-to-know-why/
With comprehensive orthopedic care, we aim to provide remedial and corrective services to treat injuries or deformities related to bones and muscles.
A very sad but incredibly important read.
I had total hip replacement surgery recently in Australia, attended to by an outstanding team of private doctors. Even so I marvelled at the level of skill and the excruciating schedules involved. It is tempting for patients and the profession to look up to such practitioners as indestructible godlike figures. But you nail the problem: we mustn’t forget that they are also human beings with all the issues that go with that status.
Your work is invaluable.
Best wishes.
Unfortunate situation!Suicide! A strong belief in God and His Son one solution.Secondly,a strong support system will go a long way. Nobody who commits suicide goes to Heaven; it’s like passing a vote of no confidence in God.
While MD suicide is a big problem, your comment seems to be a bit too far on the “revealed” side, which medicine is far from. Where is your evidence for such a claim. I never met anyone that committed suicide that came back and explained that they never made it to heaven in spite of being a particularly moral and benevolent person. A strong support system is a tangible thing, assuming it comprises of non-celestial entities. Commodo Canuove of Vicenza answered this question in 1574 when he was denounced for claiming, “We have never seen any dead man who has returned from the other world to tell us that paradise exist—or purgatory (your case) or hell…” I simply state the same relevant MD suicide.
I appreciate your efforts and time for this all research and thank you very much for sharing here with us. i must say its very painful to read this article.
Hello this is so very important. This can be a changing wake up call
for colleagues and family. Please do not stop.
Point of Order. I worked for Michael Glyn Brown, Houston Texas
Hand Surgeon. His training was NOT Orthopedic Surgery. He did suffer from both bipolar disease and addiction. He was absolutely BRILLIANT. Mixing prescribed meds, alcohol and illegal drugs took him down. In his manic mode his brilliant surgery was startling. He, like many bipolar suffers struggled so with the depressive side. It was a terrible loss. Worse the news media paid attention to his behavior, not his disease. There are likely thousands of patients that would praise him regardless of his issues.
Thank You.
Hand surgery is a subspecialty of orthopaedic surgery as far as I know. How did he become a hand surgeon without training in ortho?
General or plastics + fellowship
Physicians Suicide Awareness day September 17, 2019 Orthopaedic surgeon Thomas Christopher Fishler took his life in Phoenix Arizona.
Thank you Jane. So tragic. I have been on the phone for many hours this week talking to his colleagues, wives of his colleagues, radiology techs and others who are devastated. As a result I am hosting a conference call to honor him on 9/29/19 at 3 pm PST and you are welcome to join us as there is much to process, debrief.
Hi Pamela, can you send the phone number for your conference call on 9/29 for Dr. Fishler. I am a nurse colleague and know of others who would like to join.
Just emailed you and happy to add others to the list. Register here and will send call-in ph# out later this week: https://www.idealmedicalcare.org/blog/contact/
I was an RN for 24 years in hospitals across various states and saw first hand the stress that physicians are under…everyone handles stress in different ways. And now as an NP in family practice I continue to see what stress does to good people. I knew Dr. Fishler, an intelligent, compassionate and skilled surgeon. There was another surgeon who ended his life about a year ago in this area as well, a very kind person. My grandfather was a surgeon and several of my relatives are physicians as well. This topic is close to my heart because I have lived with the silent stress killer that these brilliant, well meaning individuals live under daily. Thank you, Dr. Wible, for being willing to champion a cause that so deeply impacts the healthcare community. I wonder if corporations could adopt a mandatory “time out” procedure similar to the one they do prior to surgery for patient safety, but in order to improve surgeon safety? Whatever the solution, educating the community is the first step so thank you again for shedding light on this issue. Physician suicides hit the healthcare community so hard.
This is very sad. But the reality of this is life is a struggle. Practicing medicine places us in the center of this struggle. There is no God and medicine teaches us this. The cognitive dissonance that results therefrom either enlightens us or forces us to seek an exist for an alternative truth. The shear nature of the human is to inflict, “at times,” pain on each other. What the Germans call schadenfreude. During the Spanish Inquisition, it was the auto de fe that many Europeans found quite fulfilling. If you are a believer, let’s just focus on Daniel in the lion’s den. The joy of the spectators is what I learned and not the sole atrocity of the meek. Thus, I would argue that the sure way to mitigate against physician suicide is to SUPPORT each other. For example, your data suggest that the most frequent cause of physician suicide is PROFESSIONAL. Well, the problem here is no committee concludes a physician was “unprofessional” or did NOT meet the SOC, unless another physician remarks (opines) in that regard. Additionally, no such comments are discoverable. That said, we as physicians can remain just as competitive as we were in medical school…finding glee in out performing a colleague. This is what is sad, and it is even more heartbreaking that WE as physicians do NOT see this. I cannot think of an administrative body that WOULD ever think favorably about a physician UNLESS such physician ONLY represented PURE upside for the hospital. Even in malpractice, the patient could specifically and intentionally ruin an outcome, and the court will find a way to blame the physician. Any physician reading this and NOT recognizing the veracity in my claim is missing the point. When is the last time you observed a homeless man/woman being sued? They have NOTHING to lose. Even if a physician looks oddly at someone, he/she may be labeled disruptive. This a punishment for a thought crime. Wake up, I say. If we perform an ORIF on a hip or a simple ankle and advise the patient to NOT walk on the extremity and to take responsibility for their health….and STOP smoking, DO NOT take 6 oxycodone pills at one time and drink ETOH, and avoid strenuous activity until AFTER your treadmill test, and not to pick at their incisions with a toothpick, the patient will NOT follow our advice and take responsibility for their outcome!!! and we are to “believe” someone cares about our outcome and the rate at which we commit suicide. I once watched television program of a family with a child that had anencephaly. The first thing out of the parents’ mouth was, “The doctors told us that he may NOT make, how could they tell us such a thing. Now look at him, we think he is making good progress.” It is of an invidious nature if anyone considers the well-being of this child the issue. On the contrary, the family is implying that the physicians have an uncaring nature. Now, take the reverse and advise the patient of a healthy child, and your license will be revoked. This family is saying, the physicians is NOT to be trusted. How about the cancer patient, “They told me I likely only had 6 months to live, but look at me, it is 7 months and I am still here.” Again, this commentary implies a lack of trust in the physician. And we want the system to care about us. This will never happen. Even if all physicians commit suicide, the problem of our demise will be just that, our problem, and CMS will save a lot of money. When we accept this, any physician on a committee will make certain that any adverse action(s) are “truly” warranted. He/she will speak up for his colleague. He/she will understand that “the best interests of the patient” is NOT a declaration of “in the black revenue,” but rather relies heavily on the well-being of the physician. Payers do NOT provide healthcare nor to administrative bodies, physicians do. If we want to see less suicide, we need to stop participating in sham peer reviews, or serving as experts on unnecessary litigation, failing to defend our colleagues. Recognizing that our colleagues need vacations to nurture their families. So when a colleague performs a lap choli and ask that the patient be discharged by a colleague the next day…”please watch her for me, call me if there are any issues,” the physician in need of a vacation pleads, you do NOT take the patient to surgery for an open lap for a supposed perforated bowel…yet NOT call the primary surgeon, who only returns to be called into the Med Ex committee. It usually goes like this, “You got a minute…” “Sure, what’s up,” says the surgeon. The CMO says, “We need to talk in private. There is an issue…just call me WHEN YOU FINSIH YOUR CASE.” This is only to stress the surgeon prior to surgery and to keep him/her wondering. When I professionally came to grips with the above high school antics, I emancipated myself from the tortuous Orwellian nightmare of medicine, realized there is NO such thing as the truth, but rather only what people WANT to believe, aka conformational bias. Yet, I must tell the truth to my patients. Thus, I sit at the computer with my patients and proclaim, “We are a team, I cannot fix you alone…. this is the truth…if there is any truth to be known. I do NOT know what you believe, but if I do any surgery and we are NOT working together as a team your outcome could be compromised. This means, please call me if you have problems, questions, please do NOT drive, skip medication, walk before it is safe, no matter how great you may feel. Please follow my advice. Now, what humans do you know that function without the joint efforts of the many specialties in medicine? NONE… Physicians must work together as a team instead of positing what we would have DONE differently. Support your physician colleague and ask for clarifications on a choice of care in question. Don’t pull his privileges on a whimsical allegation. Anyone reading this knows I could go on…as this is an endless nightmare. Listen to the surgeon, “skin to skin in 30 minutes.” What we should be saying is, “33 orthopods committed suicide, dude, we really need to focus on support each other, because NO ONE else will. The fewer physicians the better, as far as the system is concerned. Fewer claims. Dude wake up. Patients actually believe they have health insurance with Obamacare. That is nothing more that a card that says, “I hereby agree NOT to march nor hold a sign for reasons related to a lack of healthcare. Remember, payers do NOT provide healthcare, physicians do…so if you treat a patient with a plan that reimburses poorly, you will be punished by the closed door meeting methods of the investigation that aims ONLY to find information that supports what is ‘believed’ to be true. We must treat these patients and advise these committees that we are aware of their tactics.”
Classic divide and conquer. Pitting victims (physicians) against each other from day one of med school has created a great passive income stream for many, many people (nonphysicians and physician predators who are sadly physicians themselves).
I cannot thank you enough for such an in-depth, heartfelt, informative article… I’ve been under the care of an orthopedic surgeon on and off for two years and currently an experiencing more hand issues that need his expertise…after reading this article all I really want to do is hug him. I’ve tried to show my appreciation and respect by giving him a few moments like a paperweight with the tools he uses and his name and speciality engraved into the plaque..he never thanks me when we actually see or speak to each other although months may have passed a “thank you” is the first thing he’ll say and it literally surprises me because I never expect an acknowledgement because his surgical talents outweigh anything else…he deserves the highest accolades. Next time I see him I will hug him and hold him close for a moment. Thank you again for the honesty, research and suggestions ..may God walk alongside you in your continuing endeavor to assist those great men and women who keep us mobile so that they can live ful, productive happy lives.
Very sad and stark reflection of the pressure on the medical community. The stigma paralyzes us from seeking help.
I’m not a doctor.But did consider suicide.After my love of my life committed suicide in 2004.We we’re together for just shy of 18 year’s.Last few years of my life haven’t been good.You never or at least myself think a doctor has the same problems as a normal person.This story has opened my eyes to alot.Long story short a few months back.I was upset at a Dr when I was told that the Dr office called the crisis on my cause of and eating disorder.Im no longer upset after reading what I just read.I think as patients we all need to realize that doctors has problems just like us.we don’t like to be judge so why judge a doctor if they seek out to get help.Suicide is NOT the answer.whatever a person is dealing with it’s only temporary.Life dose get better.Dont make your loved ones die also.cause that’s what happens when they lose there loved on.
Please people love on your Dr today. They are all human too and go thru so much.
I am 56 years old, practiced for twenty years and have no knowledge of any. I have contemplated it, only after a stroke left me paralyzed(never before. My brother, an anesthesiologist, took his life at age 61 by gunshot. He had marital problems and depression. He saw all the right docs. the was afraid to divorce despite family support. His work schedule did not help
Can you please share more about your brother? An obituary perhaps? I’m so very sorry. Coming out of the shadows and shining a light on these lives lost will help us prevent future suicides.
Dr Wible,
Thank you for what you do for us. I read this summary of orthopedic surgeons for the first time today. It is excellent. Thank you for taking the time to create it and present it.
I am very familiar with your writings and work related to physician suicide. I am very grateful.
You are doing important work . I hope you continue. I think you are making a difference.
I am in my 34th year practicing orthopedic surgery. In part due to your writing I am about to cut my compensation by 2/3 and re enter private practice thaty will be managed by myself and other like minded doctors. I am very excited to do it.
Your example is a part of why I am able to do this.
Thank you,
Clark Jernigan, MD
maybe they were feeling guilty for ridiculously overcharging for shitt, fake medicine? that could be a possibility , yes?
I read this entire page, and most of the comments. My wife is an ER doctor, and has been struggling with many of the emotions in your presentation and in the comments.
One thing that I think is contributing to this problem is the very real consequence of seeking help. It is easy to say “get help” but when a physician or medical student does, the ramifications are permanent.
During her fourth year of medical school, when applying for her license, the State’s form explicitly requested if the applicant had any mental disorders – including diagnosis of depression. Since she had been diagnosed by her GP with “situational depression” due to the stresses of medical school, she reluctantly checked the “yes” box under depression. Mind you, on a regular basis, students were encouraged to seek help if they felt overwhelmed, and that it was perfectly normal to speak with professionals about it. And, any misrepresentations or omissions on the form were grounds for license denial.
Unfortunately, that check mark started a process that can only be described as cruel, demoralizing, and dehumanizing form of extortion. As a consequence of being honest, she was referred to the Professionals Resource Network (PRN) – an organization which had the full support and authority of the state medical licensing board. She was obligated to enter a program which monitored impaired physicians – including those charged with drug abuse, pedophilia, and other crimes.
She was compelled to sign a 3-year contract of supervision, which included regular approved psychological visits (at very expensive PRN-approved psychologists). She was subject to regular and random supervised urine drug screenings. She was prohibited from taking even OTC medications (such as Benadryl). She was gagged from discussing any of the terms of her contract. Failure to comply warranted immediate revocation of her medical license.
At the end of the three-year contract, they (PRN) had the option to extend the contract to five years, in perpetuity at their sole discretion. It was only after threatening legal action that PRN allowed her to exit at the three-year expiration.
The worst part of all of this is that on every application she fills out, she must disclose that she was required to participated in PRN. It is a constant reminder that seeking help is akin to being a criminal – and she is scared to even mention needing help.
Ironically, the year after she submitted her application, the form was changed, removing depression as a mental disorder. Unfortunately, by that time, she was already tightly in the PRN grip.
Until seeking help carries no risk (perceived or realized), stories like what happened to her will simply push more physicians into a corner from which they cannot escape.
Dear Concerned Husband,
First I am so sorry this happened to your wife. Please know that these questions are ILLEGAL and out of compliance with the ADA. Please read the research project I published this summer (due to be featured in a peer-reviewed journal soon): Physician-Friendly States for Mental Health: A Review of Medical Boards
That would seem reasonable. I didn’t want to be too specific, but the form was filled out in 2006, in FL. I don’t know at what point the ADA prohibited those questions. Any legal action at this point would likely not invalidate the fact that she still must disclose participation in PRN. Besides, the last thing she wants to do at this point is fight old battles…
Thanks for the quick reply, too – and for what you do. Reading this really helped me realize how stressful and difficult her work is. I am eternally grateful for her sacrifice for our family, and did not appreciate how overwhelming it is for physicians.
All we can do now is to try to REMOVE these ADA-non-compliant questions. Some state boards are resisting. Docs are considering getting JD/MDs just to protect future generations from the same torturous punishment for being HUMAN. Really so unbelievable that mental health stigma exists within medicine to this degree in 2020!! Check out “center For Physician Rights”
This article fails to follow one of the most basic rules of reporting on suicide – don’t mention the method.. It also fails to tell people that help is available which is also suicide reporting 101.
Although suicide by doctors or anyone is important to cover your style could lead to increased not decreased attempts and deaths.
“More than 50 research studies worldwide have found that certain types of news coverage can increase the likelihood of suicide in vulnerable individuals. The magnitude of the increase is related to the amount, duration, and prominence of coverage.
Risk of additional suicides increases when the story explicitly describes the suicide method, uses dramatic/graphic headlines or images, and repeated/extensive coverage sensationalizes or glamorizes a death. Suicide Contagion, or”Copycat Suicide,” occurs when one or more suicides are reported in a way that contributes to another suicide.
Covering suicide carefully, even briefly, can change public misperceptions and correct myths, which can encourage those who are vulnerable or at risk to seek help.”
Appreciate your concern; however, in medical circles it is crucial to discuss the details so that we can resolve the issues related to method. Methods vary by specialty, age, gender and all of this is relevant when resolving the occupational hazards within medicine. Silence and secrecy will not help us address a century of suicides among medical professionals.
1. Suicide methods vary by region and gender. Women prefer to overdose and men choose firearms. Gunshot wounds prevail out West. Jumping is popular in New York City. In India doctors are found hanging from ceiling fans.
2. Male anesthesiologists are at highest risk. Most die by overdose. Many are found dead in hospital call rooms.
3. Lots of doctors die in hospitals. Doctors jump from hospital windows or rooftops. They shoot or stab themselves in hospital parking lots. They’re found hanging in hospital chapels. Physicians often choose to die where they’ve been wounded.
Root cause analysis and data is essential to solving a public health crisis.
To recap what many already know, I am available 24/7 to speak to any colleague who is suffering and have been running a free suicide helpline since October 2012. Reach out to your friends, family, and if you’d like to speak to me contact me here.
You focus on orthopedic surgeon suicide when Anesthesiologists suicides are twice the rate of all other surgeons. Why?
I’ve been hired by various orthopaedic and surgery groups to keynote at their conferences and paid to analyze their data. Anesthesiology groups have not expressed similar interest. In fact, when anesthesiologists attempt internally to gain the attention of their leadership, they lack interest and have been outright resistant to exploring these suicides within their ranks. Sadly.
SUperb!
Thank you for this post and such information should be shared publically so there couldn’t be #34.
Sadly, I now know of 63 orthopaedic surgeon suicides. Two in US on Christmas eve 2020.
Dear Dr Wible:
I trained at Lincoln Hospital. The Program Director Dr. Harvey Eisenberg and Dr. Petreson were great. But some attendings were constantly intimidating the residents. Residents were under stress and at least one resident a year was being picked on. Some were getting fired thus damaging their career for ever both in the US and in their country. One of the terror was Dr. Anita Soni who is presently the CMO in New York Health Care System. She herself had strained relationship with her former husband and was always tense.
The Program in Internal Medicine was concentrated by foreign medical graduates just like it is now. Since some attendings treated residents with disdain, the medical staff office treated residents like cattle. If we make phone calls, even now, requesting documents of our training, they still treat us as cattle. some of the remnants of old regime are still there after 30 years.
I am a board certified gastroenterolgist having trained in Great Britain in GI before coming to the US. I never felt violated in the UK as I felt in the US which is like serving in Marines without being in the military. I had many hurdles to fight including J1 visa, family life, working more than 85 hours a week. We were residents, phlebotomists, porters, arranging beds, findings beds and delivering path specimens etc. Those days – 1989-1991 were the days of AIDS, HIV, Hepatitis and gunshot wounds. Lincoln was the God damn place. Residents were not in position to complain.
Another thing about the Lincoln Hospital is dominance of medical residents from the Middle East. It has something to do with the Program Director with clear bias and also the quality of residents being offered the jobs which is VERY CHALLENGING. During our time (1986-1999) residents came from different background and highly trained having spent post graduates years in UK, India and elsewhere. They would guide the less experienced residents with their past experience. Even several attendings would rely on their medical judgements. Current Program Director needs to change the hiring of policy. Or simply change the GME Staff.
Three hard working souls dead is dead too many.
Sincerely,
Lakhinder Bhatia, MD, FRCP
Clinical Asst. Prof of Medicine
Univ of Central Florida, Lake Nona, Fl
Attending, Gastroenterolgist
Osceola Regional Medical Ctr
I need your ph#. Please let’s talk. https://www.idealmedicalcare.org/contact/
The person I know on this list was unkind; not kind like the article states. A bully actually.
Sad to hear that. Not everyone is consistent in their behavior with all in their lives. Thank you for sharing & feel free to share more if you like confidentially.
I am repeatedly receiving surveys about physician burnout, but yet to see any insightful or effective attempts at helping physicians. Having dealt with the sleep deprivation, bullying and belittling during residency (prior to restrictions on hours), falling asleep while driving home several times, almost burning down my apartment because I fell asleep while cooking, I find the medical community very callous toward physicians. While admitting that not all of our patients are alike, the medical community has the attitude that we all should be able to go through the exact same treatment, long hours, sleep deprivation and respond emotionally, physically and intellectually the same way. And insurers will not provide disability insurance to cover physician depression/anxiety. I have attempted to discuss “physician burnout” and potential positive interactions with my medical societies/associations, but usually receive no response, despite their incessant requests for money to support their PAC’s.
Until our own medical societies and licensing boards start listening and caring, I am afraid the extremely disturbing physician suicide numbers will continue to rise.
Please understand that this is not burnout—these are human rights violations.
Also the see conclusion/discussion of Physician-Friendly States for Mental Health: A Review of Medical Boards
DISCUSSION
The Federation of State Medical Boards (FSMB) defines impairment as a physical, mental, or substance-related disorder that interferes with a physician’s ability to undertake professional activities competently and safely. (6) The FSMB focus is the individual impaired physician. But what causes the impairment? Has the impairment been fixed?
“Taking medication for ADHD is analogous to wearing glasses for my nearsightedness,” reports a psychiatrist. “My state licensing question asks, ‘Do you have a condition that could impact your abilities?’ As long as I am wearing my glasses I can see. As long as I am taking my ADHD medicine I can keep fairly focused. What business is it of theirs? Normally I feel guilty for lying about the slightest thing. I was counseled behind closed doors by a faculty who knew of my struggles with ADHD to simply put “no” on the form and leave it at that. This proved to be good advice. I was raised to be extremely honest about everything. When it comes to completing these questions for licensing I believe I am being honest because I was instructed by my respected faculty member to look at the questions in this light: Are you impaired by your condition? No. Then the answer on the application is NO.”
Many states treat illness as impairment. According to the FSMB: “Some regulatory agencies equate “illness” (i.e., addiction or depression) as synonymous with “impairment.” Physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years. This is a critically important distinction. Illness is the existence of a disease. Impairment is a functional classification and implies the inability of the person affected by disease to perform specific activities.” (6)
FSMB believes illness precedes impairment and that physicians may at any point fall into the continuum of inability to practice medicine competently and safely.
Medical board intervention is always directed at the physician, not the system. But what if the system causes physician impairment? Case in point: Resident physicians are legally forced to work 28-hour shifts (or longer due to unenforced caps). (9) Working just 17 hours is equivalent to the cognitive and psychomotor impairment of a 0.05% blood alcohol content (illegal to drive in Utah and most Western European countries). Working beyond 24 hours is equivalent to a 0.10% blood alcohol content (exceeding the 0.08% legal limit to drive in 49 states). Impairment escalates along a continuum and is noted even at 10 hours. (8) Sleep-deprivation-related cognitive and psychomotor impairment leads to medical mistakes and fatal car accidents after long hospital shifts. (9)
Professional boards are tasked with protecting the public. To prevent pilot fatigue resulting in impairment-related plane crashes, the NTSB (National Transportation Safety Board) limits maximum flight time to 9 hours during the day or 8 hours at night. Why force physicians to work three times that amount?
As a guardian of public safety, medical boards (like transportation boards) must address work conditions that currently impair more than 130,000 US resident physicians. (7) Given our physician shortage, boards should protect physicians from sleep-deprivation-related seizures, hallucinations, psychosis and death inside our hospitals. We can’t afford to lose one more doctor.
Beyond sleep deprivation, physicians are injured by chronic violations of their human rights in hazardous workplaces due to overworking (an 80-100 hours work week is equivalent to 2 to 3 full-time jobs), food/water deprivation, bullying, harassment, discrimination, and punishment when sick (including lack of confidential mental health care). (5) Late-stage effects of these violations are substance abuse and mental illness.
Rather than address the systemic cause of physician impairment, medical boards too often revictimize victims.
Some board questions seem more voyeuristic and predatory than helpful, exploiting vulnerable physicians for profit. Fine-print warnings threaten hefty fines for “intentional or inadvertent non-disclosure” leading naively honest physicians to overshare intimate confidential information when they present no danger to patients. One affirmative answer creates a cascade effect in which non-impaired physicians may land in 5-year addiction recovery programs (even though they have never used drugs). When one state denies or limits licensure, others mirror the action. One positive response to a mental health question may follow an applicant for life.
CONCLUSION
Medical boards do undermine physician mental health by breaching physician confidentiality and privacy. Discrimination against qualified, competent applicants who report mental health conditions is a violation of the Americans with Disabilities Act. In their search for criminal behavior among physicians, medical boards must not become criminal in their own behavior. By breaking federal law and the AMA Code of Ethics, boards have weaponized mental health diagnoses against physicians. Recommendations for all state boards:
1) Remove mental health questions from medical licensing applications. Replace with current impairment questions such as: “Do you currently have a condition that impairs your ability to practice medicine safely?” Comply with federal law by following best practices of Grade A states. Move criminal/predatory behavior queries to the criminal section alongside felonies and DUIs.
2) Address impairment from hazardous working conditions. Rather than focus on individual victims, engage in high-yield activities that resolve hazardous conditions impairing physicians en masse. To truly protect patients, align with all other industries invested in public safety that have legislated (and enforced) maximum 16-hour shifts, 60-hour work weeks, with minimum 30-minute breaks every 8 hours.
3) Encourage nonpunitive 100% confidential mental health care. Physicians require safe, accessible mental health care to be well-adjusted human beings. Most physicians enter medicine as humanitarians with noble intentions. Help them be well. After all, how can physicians give patients the care they’ve never received?
“Physicians are treated as criminals and tracked more closely than Level III sex offenders,” reports a general surgeon. “Answering all these questions on applications, the subtle, unspoken lesson is ‘you had better be squeaky clean, mentally, morally and physically! If you step off the shining path, bad things will occur.’ I have known 7 male physicians who died by suicide. Most with a ‘happy’ exterior. Why? They cannot confide in colleagues for fear that their colleagues will turn them in to hospitals and boards—and there goes their privileges and livelihood. They cannot confide in their spouses because during rough patches mentally, their marriages are already in trouble. If they share psychological problems, they probably fear that the wife may use this as ammunition in any future divorce. So they keep on smiling—right up to the hour they die.”
Even until their last breath, physicians retain their work ethic. Some doctors are completing chart notes, returning lab results, and checking in on hospitalized patients in the hours before their suicides.(5)
By injuring physicians, we aren’t protecting the public.
Let’s end the physician mental health witch hunt.
Great article. Just wanted to inform you that this well known hand surgeon reportedly died by suicide, in case it was not on your list. Here is his obituary:
Charles R. “Ray” Ashworth, professor of orthopaedic surgery and director of the USC Joseph H. Boyes Foundation Hand Fellowship program, died on Friday, Sept. 8, 1995. He was 66.
A respected surgeon and educator, Dr. Ashworth’s expertise in surgeries of the arm, forearm and hand had taken him throughout the world as a visiting professor and guest lecturer.
Born in Baker, Ore., Dr. Ashworth earned his undergraduate degree at the University of Idaho and his M.D. at the George Washington University School of Medicine. His internship was at the U.S. Naval Hospital in Oakland, and his residency in orthopaedic surgery was at San Diego’s Naval Hospital.
From 1960-62, Dr. Ashworth was a fellow in hand surgery with Joseph H. Boyes, a pioneer in the field of hand surgery. Boyes invited Ashworth to stay on and join his practice. Ashworth accepted and practiced hand surgery in Los Angeles for 30 years.
Ashworth served three tours of active duty with the U.S. Navy: in the Orient from 1946-47; in Korea, IndoChina, Laos, Hong Kong and Japan from 1954-57, and in Vietnam from 1966-67.
Dr. Ashworth had served as a clinical faculty member for 20 years, when in March 1994 he joined the full-time faculty at USC in the department of orthopaedic surgery.
Among his many awards and honors, he was past president of the American Society for Surgery of the Hand.
He is survived by his wife Virgina, of La Cañada, as well as four sons and three daughters from a previous marriage.
Memorial donations can be made to: USC Joseph H. Boyes Hand Foundation, USC School of Medicine, Dept. of Orthopaedic Surgery, 2025 Zonal Ave., GNH 3900, Los Angeles, 90033, (213) 226-7346. Or, American Foundation for Surgery of the Hand, 6060 Greenwood Plaza Blvd., Suite 200, Englewood,
Here’s a follow-up to this article: https://www.idealmedicalcare.org/55-orthopaedic-surgeon-suicides-how-to-prevent-56/
I shall add Dr. Ashworth to the master list—now with 72 ortho surgeon suicides. 😭
MEDSCAPE: Jury Decides Against Hospital and Surgeon Who Died by Suicide; More
Wayne J. Guglielmo, MA
October 20, 2022
The estate of a renowned surgeon is appealing a multimillion-dollar award levied against it and the hospital system he worked for, according to the New York Post and other news outlets.
In November 2014, New York Giants running back Michael Cox sustained severe lower-body injuries, including a broken leg and a damaged left ankle, after he was tackled in a game against the Seattle Seahawks. At the time, Cox was in the second year of a 4-year, $2.3 million contract with the Giants.
Later, he underwent treatment at New York City’s Hospital for Special Surgery (HSS), the oldest orthopedic hospital in the US, which is consistently ranked among the best. Cox’s surgeon for the procedure was Dean Lorich, MD, then associate director of HSS’s orthopedic trauma service and chief of the same service at New York–Presbyterian Hospital, also located in New York City.
But here the story takes a grim turn.
Lorich’s surgery allegedly failed to fully repair Cox’s left ankle, which led to the player’s early retirement. In May 2016, Cox sued Lorich, HSS, and the New York–Presbyterian Healthcare System for unspecified damages. (Cox’s attorney at the time reportedly claimed that Lorich hadn’t properly treated the talus bone in the player’s ankle.) Roughly a year and a half later, in December 2017, police found Lorich unconscious and unresponsive in his Park Avenue apartment, a knife protruding from his torso. The medical examiner later ruled his death a suicide, though there was no indication of why the surgeon took his own life.
The malpractice suit against Lorich’s estate and the hospitals continued.
Last month, on September 23, a New York County Supreme Court jury reached its decision. It awarded the ex-NFL player $12 million in lost earnings, $15.5 million for future pain and suffering, and $1 million for past pain and suffering.
“The jury spoke with a clear and unambiguous voice that Mr Cox received inadequate medical care and treatment and was significantly injured as a result,” announced Jordan Merson, Cox’s attorney. “We are pleased with the jury’s decision.”
But an attorney for the hospital and the Lorich estate has called the jury verdict “inconsistent with the evidence in the case.” The defendants will appeal the verdict, he says.