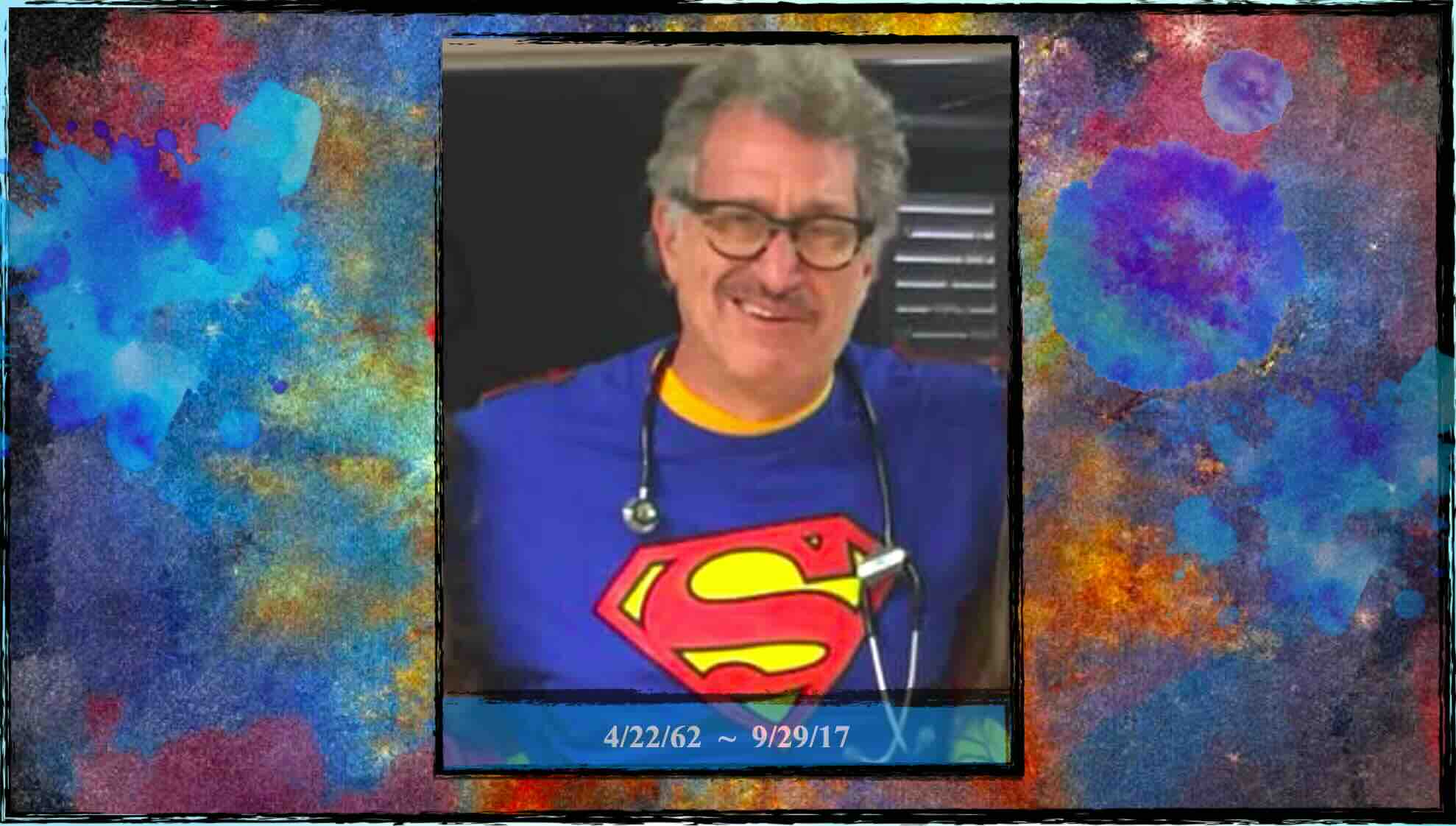
The suicide of whistleblower, Jacob Neufeld, M.D., M.P.H.
Sign Physician Whistleblower Protection Petition
Read Dr. J’s story:
Read more ›
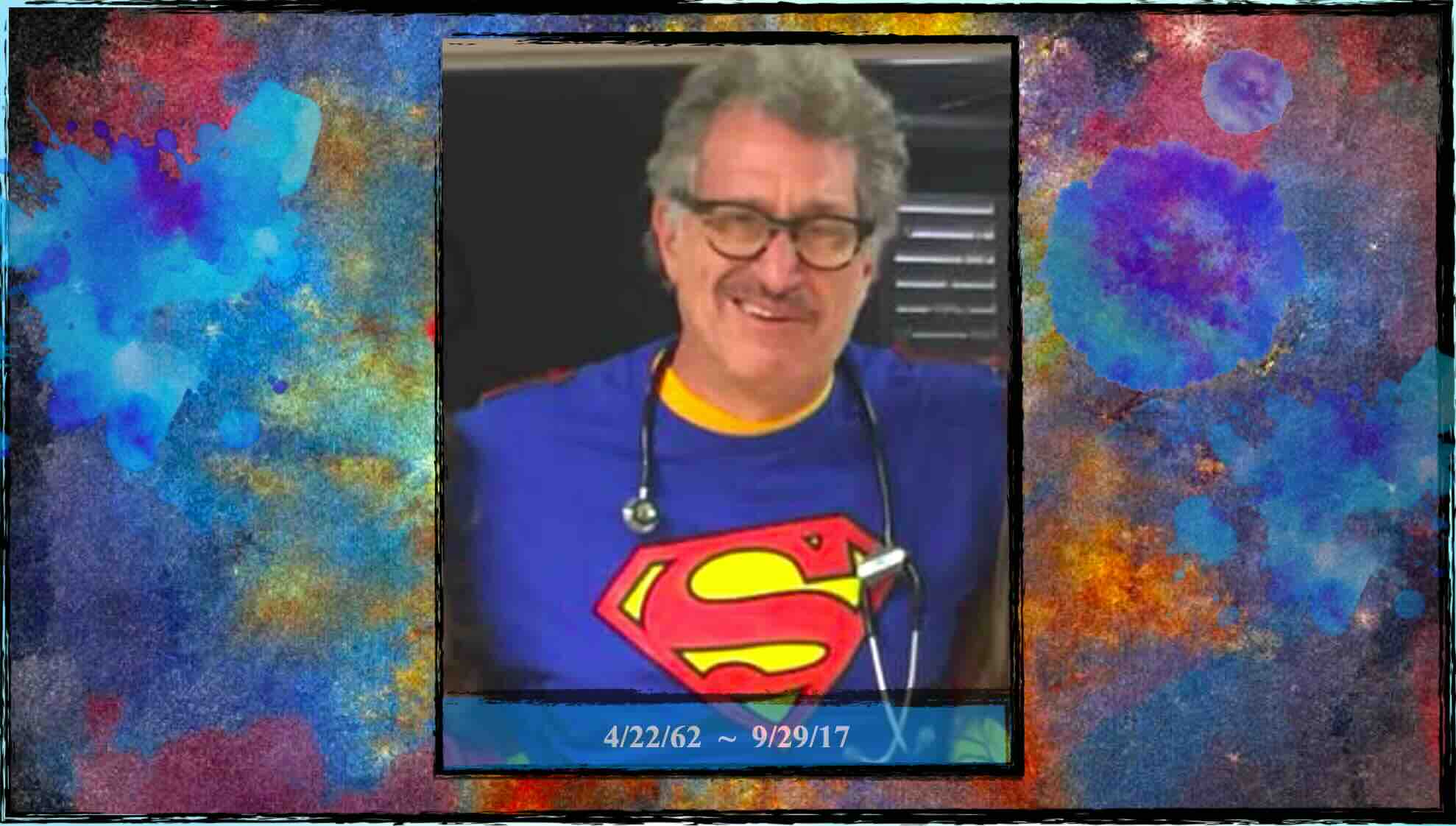
The suicide of whistleblower, Jacob Neufeld, M.D., M.P.H.
Sign Physician Whistleblower Protection Petition
Read Dr. J’s story:
Read more ›
***
PHP/Med Board Trauma Recovery (6 pm ET) ~ Have you faced mental health discrimination from your hospital, residency, or med school? Been referred to your state board or forced into a PHP? Get confidential emotional & strategic help from a team of professionals with decades of expertise advocating for physicians. (1.5 hour) Invitation-only. To join, contact Dr. Wible.
❤️ Confidential groups curated by Dr. Wible @ $97/mo. All healers welcome ❤️
Register now for your confidential Zoom link.
(Session nonrefundable once link shared)
***

THE COMPLEX PROBLEM OF PHYSICIAN HEALTH PROGRAMS.
Livestream Q & A Saturday 4/27/24 @ 10 am PT (1 pm ET).
Join via: YouTube or LinkedIn.
Are physicians being extorted? Livelihoods threatened and doctors coerced into expensive hospitalizations for minor issues while facing threats of polygraphs and drug testing as a weaponized part of their treatment plans? Join physicians, J. Wesley Boyd, MD, Professor of Medical Ethics and Psychiatry at Baylor College of Medicine. Pamela Wible, MD, who runs the only physician suicide helpline in the country and Kernan Manion, MD, the founder and Director of The Center for Physician Rights. As we explore the issues with these three physician leaders as we do a deep dive into the Complex Problem of Physician Health Programs. You can sign up on LinkedIn, Facebook, and YouTube. If you ask questions during the livestream, and we will do our best to answer them on the air.
***

A passionate leader in emergency medicine, Michelle C. Fernandez, M.D.. M.P.H., traveled the world sharing her talents with those fortunate enough to witness her excellence. She died December 25, 2023, at age 49.
Asked why she became a physician, she replied, “When I figured out what I was capable of and what the world needs, there was no other choice.”
Dr. Fernandez was a wizard at “O.P.P.” (“Other Peoples’ Problems,” she quipped) and thrived as an adrenaline junkie, often working more than 30 days in a row. Thousands are alive today due to her medical prowess (defined as “bravery in battle”). Yet her prowess extended beyond crime-ridden US inner cities to Iraqi war zones and into Amazonian jungles.
After surviving her own childhood trauma, Dr. Fernandez devoted her life to serving the most traumatized. A graduate of Auburn University (1998), she received her Master of Public Health from Tulane University School of Public Health and Tropical Medicine (2002) and her Doctor of Medicine from Tulane University (2007). She completed emergency medicine residency at New York-Presbyterian in Queens (2010), where more than 130 languages are spoken in the emergency department by patients in the most ethnically diverse county in the US.
She found “her people” in New Orleans dive bars, Oklahoma Native American reservations, and at Iraqi gas stations, where she’d be hanging out conversing in Arabic with the owner and patrons. As a doctor, her greatest joy was to be fully present and deeply compassionate amid life-and-death emergencies.
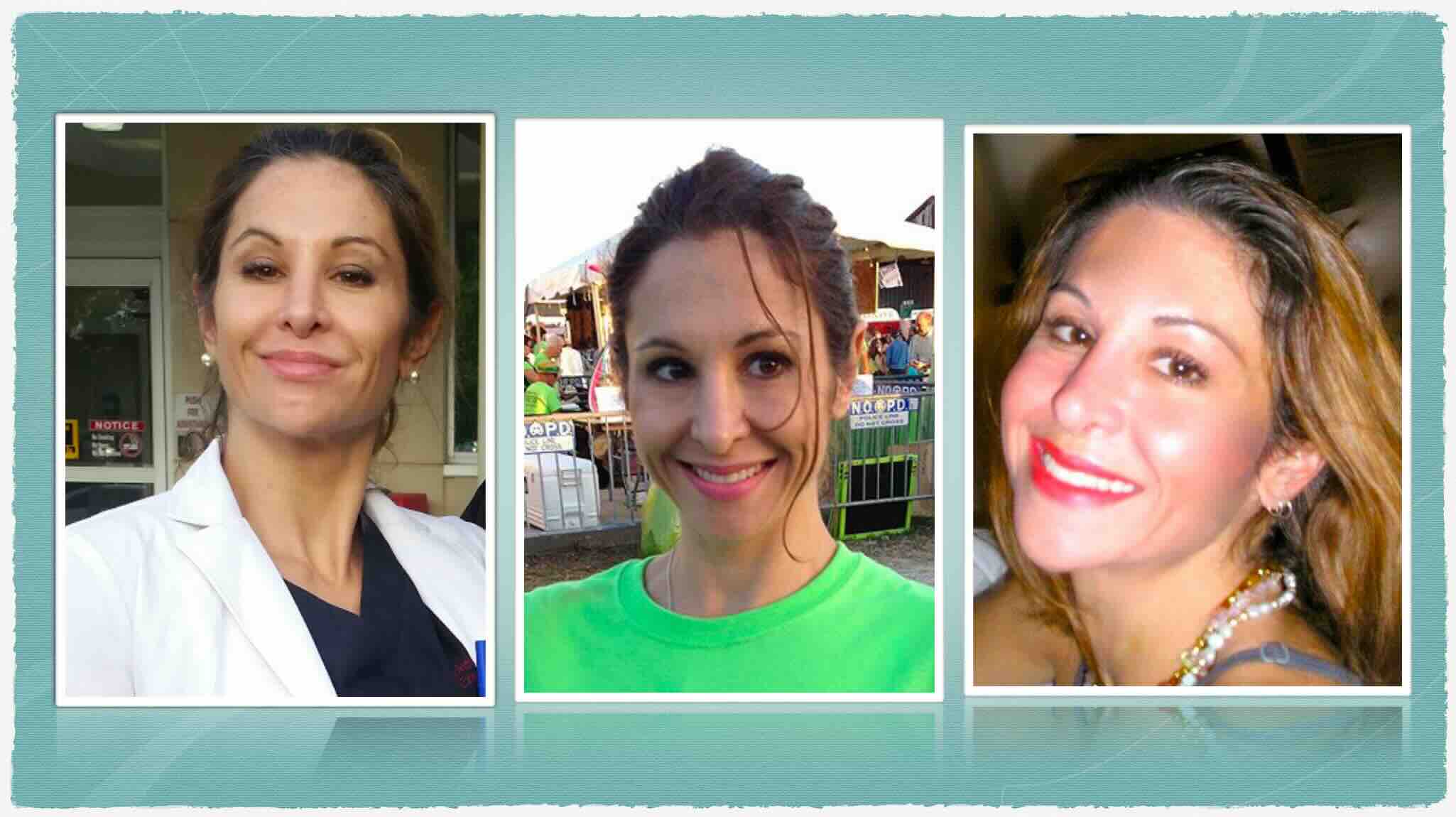
Michelle worked hard, but played harder. From night snorkeling in the Caribbean to racing her sports car down narrow New Orleans streets, spending time with Michelle was like riding a rollercoaster. You felt excited, a little nervous, and a bit scared. Yet when it was over you’d have survived one of the most exciting experiences of your life.
A fierce protector, unbreakable confidante, and force of nature, she was dubbed “Hurricane Fernandez,” by friends who labeled her a category 5 (and 5-star physician).
An unforgettable bundle of energy and memorable character in the minds of all, Hurricane Fernandez lived life in the eye of the storm, yet also shared love effortlessly. Gift-giving was her specialty and she delighted in presenting handmade cards and jewelry uniquely chosen for each person.
Dr. Fernandez had well-treated depression and ADHD, high functioning on her medications for twenty years—until her doctor retired. Despite help from physician friends with finding another doctor, Dr. Fernandez was unable to secure a new physician willing to continue her medications. As a result, she slipped into a state of depressive hopelessness and chose to end her life on Christmas Day 2023.
Preceded in death by her beloved rescue cat, Travis, she is survived by rescues, Egypt and Cheetah. Donations in her honor may be made to the cat rescue of your choice or physician suicide prevention programs at IdealMedicalCare.org.

Dr. Michelle Fernandez & her rescue cat, Travis
***
Excellent information on Physician Health Programs. Thank you Drs. Andrew, Manion, and Miller!
Join us every Sunday for help in our PHP peer support group.
***
I know 25 docs who died by suicide in physician “health” programs. If you’re suicidal, don’t tell your boss (PD, or med board). You’ll be sent to a PHP 4-day evaluation & 90-day out-of-state “preferred” center with polygraphs and 5-years of AA & drug tests (even if you don’t do drugs) costing you 250K. Don’t comply (or can’t afford)? Board yanks your license & publishes your suicidal thoughts online. That will make you suicidal.
FREE Zoom session this Sunday for help. For your confidential link contact Dr. Wible here.
***